* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Drug Regimen Review
Survey
Document related concepts
Drug interaction wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Drug discovery wikipedia , lookup
Medical prescription wikipedia , lookup
Compounding wikipedia , lookup
Prescription costs wikipedia , lookup
Intravenous therapy wikipedia , lookup
List of comic book drugs wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Theralizumab wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Transcript
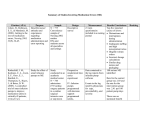
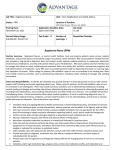
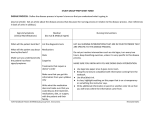
CHAPTER 13 MONITORING DRUG THERAPY IN THE NURSING HOME (THE MEDICATION REGIMEN REVIEW) 13.1 NURSING HOME MONITORING DRUG THERAPY IN THE NURSING HOME I. Types Of Medication Regimen Reviews 1. Prospective MRR – the review of drug therapy is done at the time of admission 2. Concurent MRR – the review of drug therapy is completed while the therapy is in progress 3. Retrospective MRR – the review of drug therapy is completed after the therapy has been completed or the patient has been discharged *II. The key areas of the chart reviewed by the Consultant Pharmacist and the information obtained from each area of the chart 1. The Physician Order Sheet (P.O.S.) • • • • • • • • Current medication orders including the drug name, strength, frequency and possibly the length of therapy Cumulative diagnoses on the patient. In some cases the P.O.S. will also identify supporting diagnoses for each routine drug in use. The prescriber for each medication Ancillary orders Diet Physician signature indicating the date of his/her review The P.O.S. may also include new orders written in-house since the beginning of the month 2. The Telephone Orders written since the last review • • • • New medication orders written since the beginning of the month Discontinued orders since the beginning of the month Whether the prescriber has reviewed and countersigned the telephone order The T.O. may also include a supporting diagnosis for the new order 3. The Medication Administration Record (M.A.R.) & PRN sheets • • • • • • • The administration times for each medication in use All medications that have been discontinued since the first of the month All new medications started since the first of the month Doses of medication held and the reason they were held Charting omissions that may compromise the effectiveness of the therapy The use of PRN doses for the patient and the effectiveness of each dose Doses that are being crushed or administered through a tube 4. The Psychoactive Drug Flow Sheet • • • • • The target behavior being measured to document therapy effectiveness The frequency of behaviors by day and shift Non-drug interventions that may be effective in controlling behaviors Side Effects identified that are possibly related to the psychoactive therapy The impact of dosage adjustments on the frequency of target behaviors 13.2 5. The Nursing Notes • • • • • • • • • Vital signs Bowel and bladder function Pain levels Falls and other incidents Resident comments that may indicate mental state Sleep patterns Symptoms of developing conditions such as edema, cough, temperature Side effects of current therapy such as drowsiness, GI pain, constipation Effectiveness of new therapy 6. The Physician Progress notes • • • The physician’s assessment of the patient’s condition The physician’s rationale for choosing a new medication The physician’s plan for treating the patient 7. Lab reports taken since the last review • • • • Date and “draw time” for all laboratory tests completed Type of labs completed Previous labs for comparison with current results Sub-therapeutic and toxic levels 8. The M.D.S. • • • • • • Former habits and work history Pain status History of falls History of depression and other behavioral symptoms History of chronic disease that may not appear on the P.O.S. History of medications and allergies 9. The resident’s Care Plan • • • • • The proposed treatment plan The effectiveness of previous therapy The impression of facility staff regarding patient’s rehab potential Mental status and the results of non-drug interventions Future plans for care and therapy III. Federal Indicators used in the Medication Regimen Review *1. F329 - Unnecessary Medications *2. F428 - Drug Regimen Review *3. F425 - Pharmacy Services 4. F272 - Resident Assessment 5. F315 - Urinary Incontinence 6. F319 - Mental and Psychosocial Functioning (* - of primary importance) 13.3 NURSING HOME *IV. What are we looking for during the Medication Regimen Review? 1. 2. 3. 4. 5. 6. 7. 8. 9. Review new orders to rule out the possibility of treating an unidentified adverse effect Review nursing notes to rule out unidentified adverse drug reactions Make sure that all doses are within normal geriatric range Make sure duration of therapy is appropriate Make sure that dosage reductions are attempted on the anxiolytic and antipsychotic drugs Make sure there is a supporting diagnosis for each order Make sure there are no untreated conditions Review PRN drug usage to ensure they are not becoming routine orders Review Lab values to identify sub-therapeutic or toxic levels or Irregularities caused by current therapy 10.Pharmacy service issues such as untimely deliveries and out of stock medications that may adversely affect the patients outcome. V. Other issues that may be picked up during the MRR 1. Physician orders not being signed monthly 2. Telephone Orders not signed in a timely manner 3. New orders written in the chart but never ordered from pharmacy or initiated on the Medication Administration Record (MAR) *VI. Documentation required by the consultant to prove the MRR was completed 1 Review the drug therapy of each resident at least monthly. Unstable patients or high acuity facilities may require more frequent chart reviews by the consultant pharmacist. As an example, a sub-acute facility may require weekly or every other week medication regime reviews 2. Sign and date each Resident’s chart monthly 3. Document any areas of concern in a written note 4. Document “No Irregularities Noted” if there are no concerns 5. Prepare a monthly report that summarizes the entire M.R.R. for the Director of Nursing and Medical Director 6 Follow up on previous recommendations to ensure that every Prescriber has responded 7. Prepare a quarterly report that summarizes the past 3 months of consultant activities in the facility 13.4 NURSING HOME SAMPLE POLICY & METHODS Medication Regimen Review Policy: The consultant pharmacist or his agent will review the drug regimen of each Resident at least monthly and report, in writing, any irregularities. For the purposes of this policy, the term irregularity shall mean failing to be in accord with what is usual, proper, accepted, or right. Methods: 1. The consultant pharmacist will provide the facility with documentation that each resident’s drug regimen has been reviewed by signing and dating the monthly physician’s drug summary. 2. The consultant pharmacist will provide to the director of nursing each month a written report with a statement about each resident and any irregularities found. If no irregularities were noted this shall be so noted. This report will be signed and dated by the consultant pharmacist and all irregularities will be highlighted to indicate that some action is required by nursing. The director of nursing will respond in writing on the report what action had been taken on those irregularities so reported. This completed report will be made available to and signed by the administrator and medical director and retained in the facility for one year. A summary of these reports will be made quarterly by the consultant pharmacist to the Quality Assessment and Assurance Committee. 3. The consultant pharmacist will provide a copy of the above report to the medical director each month. The medical director will review, make comments, and sign the report. It shall be returned to the director of nursing and retained in the facility for one year. 4. The consultant will be available by pager or cell phone and should be contacted by nursing whenever a new patient is admitted or a drug related event is suspected by the nursing staff. The consultant will make arrangements to review the apparent event (or new admission) and provide the facility with a written report within 24 hours of the review. 5. The facility will forward the interim consultant review to the attending physician via fax followed by a phone call (when necessary) so that any identified problems can be addressed by the prescriber in a timely manner. 13.5 Extracted from: Nursing Homes - Clarification of Guidance related to Medication Errors and Pharmacy Services - CMS November 2012 III. Medication Regimen Reviews for Stays under 30 days and Changes in Condition Consultation (including medication regimen review) by the pharmacist can promote safe and effective medication use. The regulation at F428-Medication Regimen Review requires that a licensed pharmacist review each resident’s medication regimen at least once a month. The facility is expected to have a proactive, systematic and effective approach to monitoring, reporting, and acting upon the effects, risks, and adverse consequences of medications. The pharmacist may need to conduct the medication regimen review more frequently (for example weekly), depending on the resident’s condition and the risks for adverse consequences related to current medications. The requirement for the medication regimen review applies to all residents, including residents receiving respite care, residents at the end of life or who have elected the hospice benefit, residents with an anticipated stay of less than 30 days, or residents who have experienced a change in condition. Complex residents generally benefit from a pharmacist’s review during the transition from hospital to skilled nursing facility.8 This review may prevent Errors due to drug-drug interactions, omissions, duplication of therapy or miscommunication during the transition from one team of care providers to another. 13.6 The current guidance at F425-Pharmacy Services provides examples of how the facility, in collaboration with the pharmacist and medical director, can establish procedures to address medication regimen reviews for residents whose anticipated stay is less than 30 days. According to the guidance, facility procedures are expected to address how and when the need for a consultation will be communicated, how the medication review will be handled if the pharmacist is off-site, how the results or report of the pharmacist’s findings will be communicated to the provider, the expectations for the provider’s response and follow up, and how and where this information will be documented. Survey Implications: Both the previous and the current guidance at F428-Medication Regimen Review have identified that the pharmacist may need to review a medication regimen more frequently, depending on the resident’s condition and the risk for adverse consequences associated with the medications. Efforts to prevent medication-related adverse consequences and to recognize existing or emerging complications are a significant focus of clinical care in nursing homes. If there is evidence the pharmacist should have conducted more frequent reviews, surveyors should consider consulting an advanced practitioner, pharmacist or physician at the State Survey Agency or Regional Office to review cases in which this practice may be considered deficient. If non-compliance has been identified at F428, then additional requirements may also be considered and investigated such as F385-Physician Supervision; F329-Unnecessary Medications; or F501-Medical Director. For questions on this memorandum, please contact [email protected]. Effective Date: Immediately. This policy should be communicated with all survey and certification staff, their managers and the State/Regional Office training coordinators within 30 days of this memorandum. 13.7 SAMPLE PROSPECTIVE MEDICATION REGIMEN REVIEW CHECKLIST Resident:___________________________________Date:_______________Facility:________________Wing:___ ___________________________ Room #:______________ Physician:__________________________ Pharmacist Reviewer: _____________________________ R.Ph. Phone:_______________________ The following recommendations were made: No Recommendations Made. Drug Stop Date Request:______________________________________________________________ Drug information Request Provided to Nurse or Physician:___________________________________ Regarding the following:_____________________________ Reference(s):_____________________ More information needed before request can be processed. Explain: ___________________________ AIMS review with antipsychotic use initially and every 6 months. Drug Therapy Intervention Requests. If accepted by MD, must have a separate physician order. Drug Directions Recommendation Reason Reason: 1-Change to formulary drug, 2-Therapeutic interchange, 3-Less cost, 4-Improved patient care, 5-Incomplete directions, 6-Not for use in elderly, 7-Duplicate therapy, 8-Inappropriate dosing, 9-Allergy, 10-Drug interaction, 11-Drug/disease interaction. Medications Requiring Diagnosis(es). Fax to Pharmacy when Complete. Medication Diagnosis Nurse:_______________________________ Date:________________________________ Request for Laboratory Monitoring: ___Glucose Frequency:________________ ___Potassium Frequency:________________ ___Digoxin Level Frequency:________________ ___CBC Frequency:________________ ___Carbamazepine Frequency:________________ ___Valproic Acid Frequency:________________ ___PT/INR Frequency:________________ ___Phenytoin Level Frequency:________________ ___TSH Frequency:________________ ___BUN/Creatinine Frequency:________________ Physician:_________________________________ Date:______________________________________ 13.8 PROSPECTIVE MEDICATION REGIMEN REVIEW CHECKLIST Resident:___________________________________Date:_______________Facility:______________________Wi ng:______________________________ Room #:______________ Physician:__________________________ Pharmacist Reviewer: _________________________________R.Ph. Phone: ___________________________ The following recommendations were made: No Recommendations Made. Drug Stop Date Request:_____________________________________________________________________ Drug information Request Provided to Nurse or Physician:__________________________________________ Regarding the following:____________________________________ Reference(s):_____________________ More information needed before request can be processed. Explain:___________________________________ AIMS review with antipsychotic use initially and every 6 months. Drug: ______________________________ The following is a condensed list of medications that may require additional clinical monitoring. The proposed monitoring are recommendations only, however they do reflect recommendations found in Tag F329. If monitoring took place in the hospital and results are available to the facility it may be appropriate to delay additional laboratory testing at this time. DRUG LAB TEST & FREQUENCY ACE Inhibitors Drug: _______________________________ Angiotensin Receptor Blockers:_______________________ Chem-7 Q 6-12 months Chem-7 Q 6-12 months Allopurinol (Zyloprim) Chem-7, Uric Acid Q 6-12 months Aminoglycosides Antibiotics (Gentamycin, Tobramycin) & Vancomycin Peak and trough levels + Creatinine Clearance Amiodarone (Cordarone) LFT's, TSH, CBC Q 6-12 months Anticoagulants CBC Q6 months Appetite Stimulants Drug:______________________ Appetite and weight should be monitored and agent should be dc'ed if there is no improvement Atypical Antipsychotics (Abilifty, Geodon, Risperdal, Seroquel & Zyprexa) Fasting Bloog Glucose monthly x 3 months then quarterly. Lipid profile (including Total Cholesterol) baseline + annually. Carbamazepine (Tegretol, Carbatrol) LFT's, CBC, Serum level Q6 months + Serum level 7 days after each dosage adjustment Cholestyramine (Questran) May interact with medications given at the same time. Separate by at least 1 hour before or 4 hours after Questran dose. Lipid Profile Q6-12 months Clozapine (Clozaril) CBC weekly or bi-weekly depending on past lab history Digoxin (Lanoxin) Serum Digoxin level Q6-12 months and whenever side effects are suspected. Pulse daily Diuretics Drug:________________________ Erythropoiesis Stimulating Agent (Epogen, Procrit & Aranesp) Folic Acid Chem-7 and or Electrolytes within 30 days of therapy initiation + Q6 months. Blood Pressure weekly. CBC twice weekly during dose adjustments and monthly therafter. Some insurance plans require Ferritin & TIBC levels for prior approval. CBC Q6 months. Folate level if needed Glyburide (Diabeta) & Chlorpropamide (Diabinese) Fasting Blood Glucose at least Q60 days + HgA1c quarterly. These products should be avoided in the elderly due to their long half life and greater risk of hypoglycemia Heparin SQ CBC baseline Hydrochlorthiazide Chem-7 and or Electrolytes within 30 days of therapy initiation + Q6 months. SCr Q6 months. Blood Pressure weekly. Insulin Fasting Blood Glucose at least Q60 days + HgA1c quarterly Drug: _________________________ FACILITY NAME: __________________________ RESIDENT’S NAME: ____________________________ 13.9 DRUG LAB TEST & FREQUENCY Iron Supplements Drug: _______________________ CBC within 30 days of therapy initiation then Q6 months. TIBC, Serum Ferritin, Serum Iron yearly (CBC, TIBC, Serum Ferritin, Serum Iron, Reticulocyte Count, Transferrin Saturation to determine Iron deficiency anemia) Lithium (includes Lithobid & Lithium Citrate) Serum level Q week until stable, then monthly. Chem-7, TSH and CBC Q6 months Metformin (Glucophage) SCr, BUN Q6 months, Fasting Blood Glucose Q60 days + HgA1c quarterly. This drug has been linked to lactic acidosis especially in males with serum creatinine > 1.5mg/dL and in females with serum creatinine > 1.4mg/dL Nitrofurantoin (Macrodantin or Macrobid) SCr, BUN within 30 days of starting therapy then Q6 months Should not be used if renal function is impaired (CrCl <60) due to decreased effectiveness & increased side effects Non-Steroidal Anti-Inflammatory Drugs (NSAID) Drug_______________________ CBC, Chem-7 Q 6months. Monitor closely for bleeding especially when coadministered with Aspirin >325mg/day or when used with platlet inhibitors or anticoagulants Oral Hypoglycemics Fasting Blood Glucose at least Q60 days + HgA1c quarterly Phenobarbital Serum level Q6 months + Serum level 7 days after each dosage adjustment Phenytoin (Dilantin) CBC, Serum Albumin and Serum level Q6 months + Serum level 7 days after each dosage adjustment Potassium Supplements Drug:___________________ Chem-7 Q6 months Rosiglitazone (Avandia) & Pioglitazone (Actos) These agents can cause weight gain and edema. Monitor weight. Statin Drugs Drug: __________________________ Baseline LFT's before starting therapy, then in 12 weeks after starting therapy or increasing dose. LFT's and Lipid Profile Q6-12 months Synthetic Heparin products (Lovenox, Fragmin, etc) CBC baseline Theophylline Serum Theophylline level Q6 months Thyroid Supplements TSH, annually and 6 weeks after each dosage adjustment Urinary anti-infectives Chronic infections treated with prophylactic therapy - UA 30 days following the start of therapy Valproic Acid (includes Depakene & Depakote) LFT's, CBC, Serum level Q6 months + Serum level 7 days after each dosage adjustment Vitamin B-12 CBC Q6 months. B-12 level if needed Warfarin (Coumadin) INR daily to weekly on initiation until stable - then INR weekly to monthly [ ] Hospital Lab results are available in chart. MISSING DIAGNOSES DRUG SUPPORTING DIAGNOSIS DRUG INTERACTION NOTIFICATION The following medication(s) may have the potential to result in a drug interaction. Please assess the risk versus benefit for the concomitant use of the following medications: [ ] I authorized the above recommendations [ ] I do not wish to implement the above recommendations Physician:_________________________________ 13.10 Reason: _______________________________ Date:______________________________________ CONSULTANT PHARMACIST M.R.R. SIGNATURE LOG YEAR: MONTH PATIENT NAME: SIGNATURE REVIEW DATE ____________________ NOTES JANUARY [ ] No Irregularities Noted FEBRUARY [ ] No Irregularities Noted MARCH [ ] No Irregularities Noted APRIL [ ] No Irregularities Noted MAY [ ] No Irregularities Noted JUNE [ ] No Irregularities Noted JULY [ ] No Irregularities Noted AUGUST [ ] No Irregularities Noted SEPTEMBER [ ] No Irregularities Noted OCTOBER [ ] No Irregularities Noted NOVEMBER [ ] No Irregularities Noted DECEMBER [ ] No Irregularities Noted 13.11 CONSULTANT PHARMACIST M.R.R. SIGNATURE LOG YEAR: MONTH JANUARY FEBRUARY MARCH APRIL PATIENT NAME: NOTES _______________________________ REVIEW DATE SIGNATURE B.P. WEIGHT [ ] No Irregularities Noted [ ] No Irregularities Noted [ ] No Irregularities Noted [ ] No Irregularities Noted MAY [ ] No Irregularities Noted JUNE [ ] No Irregularities Noted JULY [ ] No Irregularities Noted AUGUST SEPTEMBER OCTOBER NOVEMBER DECEMBER DATE [ ] No Irregularities Noted [ ] No Irregularities Noted [ ] No Irregularities Noted [ ] No Irregularities Noted [ ] No Irregularities Noted LABS 13.12 13.13 13.14 NURSING HOME CONSULTANT PHARMACIST PROGRESS REPORT SAMPLE FACILITY Date : 1/30/13 Name: Doctor: DOB: Status: Diet: Diagnosis Misc Info: ADAMS, GUS Station: SOUTH ATHER Room: 201A 05/12/21 ADMIT 12/1/00 2000 CAL ADA – 2GM SODIUM N/A ASHD, CHF, COPD, DIABETES MELLITUS, PACEMAKER, ANEMIA, OBS WITH DELUSIONAL PSYCHOSIS Patient prefers to have meds crushed and in applesauce or pudding Lab Due Dates: ELECTROLYTES 2/12/13 Lab Due Dates: CHEM-30 2/12/13 Jan 2013 Comments : Dr Ather – Mr Adams is currently being treated with Lanoxin 0.125mg qd and Furosemide 40mg qd for CHF. Worsening edema is documented in nursing notes over the past 6 weeks. Please review current therapy for possible addition of an ACE Inhibitor ______________________________________________________ Consultant Pharmacist Date : 1/30/13 Physician Follow-Up :____________________________________________________ Nursing Follow-Up :____________________________________________________ 13.15 NURSING HOME CONSULTANT PHARMACIST PROGRESS REPORT SAMPLE FACILITY Date : 2/20/13 Name: Doctor: DOB Status Diet Diagnosis: Misc Info: ADAMS, GUS Station: SOUTH ATHER Room: 201A 05/12/21 ADMIT 12/1/00 2000 CAL ADA – 2GM SODIUM N/A ASHD, CHF, COPD, DIABETES MELLITUS, PACEMAKER, ANEMIA, OBS WITH DELUSIONAL PSYCHOSIS Patient prefers to have meds crushed in applesauce or pudding Lab Due Dates: ELECTROLYTES 08/12/13 Lab Due Dates: CHEM-30 08/12/13 Feb 2013 Comments : Progress Note – Dr Ather has agreed to add an ACE Inhibitor to current therapy in response to last months comment. Prinivil was added on 2/2/13 and edema began improving within 10 days. B.P. and Pulse remain W.N.L. _______________________________________________ Consultant Pharmacist Date: 2/20/13 Physician Follow-Up :____________________________________________________ Nursing Follow-Up :____________________________________________________ (This is a sample of how a consultant might follow-up on a previous recommendation. This note acknowledges that the MD responded to last months comment and identifies the “outcome” of the change in therapy). 13.16 NURSING HOME CONSULTANT PHARMACIST PROGRESS REPORT SAMPLE FACILITY Date : 12/7/2012 Name: Doctor: DOB: Status: Diet: Diagnosis: Misc Info: ADAMS, GUS Station: SOUTH ATHER Room: 201A 05/12/21 ADMIT 12/1/94 2000 CAL ADA – 2GM SODIUM N/A ASHD, CHF, COPD, DIABETES MELLITUS, PACEMAKER, ANEMIA, DIABETIC NEUROPATHY Patient prefers to have meds crushed and in applesauce or pudding Lab Due Dates: ELECTROLYTES 02/12/03 Lab Due Dates: CHEM-30 02/12/03 Dec 7, 2012 Comments : Phenytoin's effective level may be estimated by multiplying the patient's phenytoin level x 4.4 divided by serum albumin. Since many geriatric patients have low serum albumin levels (3 - 3.5 g/l) the effective dose of phenytoin in these patients is actually 25% to 50% higher than the reported levels. This is due to decreased serum albumin binding and a higher "free drug fraction". DR ATHER - your progress note on 12/5/2012 indicated that you are considering a psych consult due to early symptoms of dementia. Please note that current dilantin level of 14.0 mcg/ml actually is equivalent to a dilantin level of 20 mcg/ml due to a low albumin level (3.0). Cognitive changes may actually be related to dilantin toxicity _____________________________________________ Consultant Pharmacist Date : 12/7/2012 Physician Follow-Up :____________________________________________________ 13.17 COMMUNICATION SKILLS YOUR STYLE WILL IMPACT PRESCRIBER RESPONSE DO’s: 1. Always give the prescriber the benefit of the doubt since they may know more about the patient than you do 2. Address the patient by name in your comment 3. Include relevant information since the prescriber may be reviewing your comments outside of the facility (ex. Side effect occurred after a dose was increased) 4. Whenever possible leave the prescriber’s options open 5. Keep the comment concise and on point 6. Always write comments as a request (ex. “please consider”…. Or “Please review”) 7. If you anticipate a negative reaction to your comment consider talking to the physician in person. DON’Ts: 1. Don’t diagnosis in your consultant comment 2. Don’t write comments that will be perceived as increasing the prescriber’s liability 3. Don’t make jumps in logic that cannot be supported by the clinical information available 4. Don’t give the prescriber 1 solution to the problem when multiple options exist. CLINICAL SITUATION: This 89 y/o female patient is currently taking captopril as part of her CHF therapy. Nursing notes indicate that a cough developed 2 weeks ago. There are no cold symptoms noted or indications of worsening CHF. The consultant needs to address the cough in his/her chart review Consultants may communicate with different levels of effectiveness based on their communication skills ------------------------------------------------------------------------------------------------------Consultant 1 Dr Smith: Mrs. Jameson has had a chronic cough for the past 2 weeks. Please DC captopril order. ------------------------------------------------------------------------------------------------------Consultant 2 Mrs. Jameson is currently taking captopril 12.5mg T.I.D. for treatment of CHF. She has had a chronic cough for the past 2 weeks which is being caused by the captopril. Please stop the drug as soon as possible. -------------------------------------------------------------------------------------------------------Consultant 3 Mrs. Jameson is currently taking captopril 12.5mg T.I.D. for treatment of CHF. Patient developed a cough 2 weeks ago. Please DC captopril and start losartan 25mg daily since cough is a side effect of captopril. --------------------------------------------------------------------------------------------------------Consultant 4 Mrs. Jameson is currently taking captopril 12.5mg T.I.D. for treatment of CHF. Patient developed a cough 2 weeks ago, shortly after increasing the dose of captopril from BID to TID. Nursing reports no indications of cold symptoms or edema. Please review to determine if cough is related to the increase in ACE therapy. Consider a dosage reduction in captopril or a change to ARB therapy if you feel this may be a side effect of current therapy. 13.18 USING CONSULTANT COMMENTS TO REDUCE YOUR LIABILITY As mentioned in the previous section, Federal guidelines do not require the consultant to address issues that have already been addressed by the attending physician. However, acknowledgement of these issues in your consultant records provides evidence that you were aware of the issue, that it was addressed by the physician (or facility) and may reduce your liability in the event of legal action. Examples of Consultant Comments: A. Documenting Irregular Labs 1. Laboratory results on 12/1/12 identify multiple irregularities on CBC. These irregularities are consistent with current diagnosis of chronic leukopenia. Dr Ather is aware of these irregularities as indicated in 12/7/12 progress note. 2. Phenytoin level on 12/17/12 was low (8.0mcg/ml). Patient has had no seizure activity and has had fluctuations in phenytoin levels over the past year. Dr Smith (neurologist) is aware of current level and has elected to keep Phenytoin dose at 300mg/day and repeat levels in 4 weeks. B. Documenting the Effectiveness of Pain Medications 1. Mrs James is taking PRN Vicodin for left hip pain approximately 5 to 6 times per week. Nursing notes indicate that patient is requesting Vicodin prior to bedtime since her hip pain interferes with sleep. Nursing notes and PRN sheet indicate good results within 1 hour of dosing. All reports of pain throughout the day in nursing notes have been addressed by nursing staff. C. Rationalizing why you did not write an expected recommendation 1. Mrs. Howell is due for 6 month dosage reduction attempt for Risperdal 0.5mg QAM & 1mg at HS. Dr James (psychiatrist) saw patient last week and notes that behaviors have escalated recently due to death of husband. He does not feel a dosage reduction attempt is appropriate at this time. Dr Adams (attending) agrees with Dr James. I will hold comment for dosage reduction attempt for 1-2 months and address at that time. D. Recording an observation in progress notes 1. Mr Smith has been experiencing cough over the past several weeks. Patient is currently taking captopril 12.5mg T.I.D. for CHF. Dr Casey indicates in 11/26/12 progress note that he does not feel that cough is related to ACE therapy. He is treating cough with PRN Guiatuss DM. 13.19 E. Creating a plan of action 1. I will monitor PRN dose of Temazepam 7.5mg at bedtime. Usage has increased recently and appears to be related to nursing changes on this unit. Will discuss with DON to determine if patient’s insomnia has increased, if patient is requesting dose or whether nursing staff is initiating the PRN order. In each of these examples it could be argued that no consultant comment was required. Adding these comments to your monthly documentation will increase the time for each chart review. However, they will serve as an excellent chronology of your assessment and actions long after nursing notes and charting records have been “thinned” from the chart. This may ultimately save you time in subsequent months. In addition, these comments will help establish for the surveyor that you identified these apparent irregularities and documented why no action was taken. 13.20 SAMPLE OF A MONTHLY SUMMARY REPORTS SAMPLE FACILITY Date : 12/31/12 Page 1 Report is for Month: December 2012 Dear Mrs. Smith: Enclosed is a summary of this month's consultant pharmacist reports for your patients at Shady Rest. Name: Nursing Station: Doctor: ADAMS, GUS SOUTH ATHER Room No.: Maintenance RX’s: PRNRX’s: 201A RX’s 2 December Comments : Phenytoin's effective level may be estimated by multiplying the patient's phenytoin level x 4.4 divided by serum albumin. Since many geriatric patients have low serum albumin levels (3 - 3.5 g/l) the effective dose of phenytoin in these patients is actually 25% to 50% higher than the reported levels. This is due to decreased serum albumin binding and a higher "free drug fraction" DR ATHER - Your progress note on 12/1/12 indicated that you are considering a psych consult due to early symptoms of dementia. Please note that current dilantin level of 14.0 mcg/ml actually is equivalent to a dilantin level of 20 mcg/ml due to a low albumin level (3.0). Cognitive changes may actually be related to dilantin toxicity. --------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: CONRAD, FRANKLIN NORTH MEYER Room No.: Maintenance RX’s: PRN RX’s: 125A 5 1 December Comments: *No Irregularities Noted. --------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: EMMETT, ESTHER NORTH MEYER Room No. Maintenance Rx;s: PRN RX’s: 124A 3 2 December Comments: *No Irregularities Noted. -------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: EMMETT, MELVIN NORTH MEYER Room No: Maintenance RX’s: PRN RX’s: 124B 6 3 December Comments : DR MEYER - PLEASE REVIEW THE CURRENT ORDER FOR ZANTAC 150MG BID FOR POSSIBLE DOSAGE REDUCTION. THIS ORDER HAS BEEN USED IN THERAPEUTIC DOSES SINCE 7/13/12. 13.21 NURSING HOME SAMPLE OF A MONTHLY SUMMARY REPORTS SAMPLE FACILITY DATE: 12/31/12 Page 2 Name Nursing Station: Doctor: GRIFFIN, ELVA SOUTH ATHER Room No.: Maintenance RX’s: PRN RX’s 208B 7 1 December Comments : *No Irregularities Noted * --------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: KOEHLER, JANE SOUTH MEYER Room No.: Maintenance RX’s: PRN RX’s 220A 5 0 December Comments: DR MEYER - TO COMPLY WITH FEDERAL INDICATORS PLEASE REVIEW CURRENT ORDER FOR LORAZEPAM 0.5MG TID (STARTED 9/1/12) FOR POSSIBLE DOSAGE REDUCTION. -------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: OWENS, ROBERT NORTH MEYER Room No.: Maintenance RX’s: PRN RX’s: 126A 4 3 December Comments : No Irregularities Noted --------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: ROBERTS, HARRIET NORTH ATHER Room No.: Maintenance RX’s: PRN RX’s: 127A 5 1 December Comments : * No Irregularities Noted * --------------------------------------------------------------------------------------------------------------------------------Name: Nursing Station: Doctor: WATERS, WALTER SOUTH MEYER Room No.: Maintenance RX’s: PRN RX’s: 130A 3 2 December Comments : DR MEYER - TO COMPLY WITH FEDERAL INDICATORS COULD WE OBTAIN A CARDIAC DIAGNOSIS TO SUPPORT THE USE OF NITROGLYCERIN SR CAPSULES. 13.22 NURSING HOME SAMPLE OF A MONTHLY SUMMARY REPORTS SAMPLE FACILITY Date: 12/31/12 Page 3 Name: Nursing Station: Doctor: WINTERS, MARTHA SOUTH MEYER Room No.: Maintenance RX’s: PRN RX’s: 204A 3 2 December Comments : PHARMACY NOTE - PATIENT WAS HOSPITALIZED ON 12/1/2012 WITH S.O.B. CONFUSION AND FEVER. PATIENT RETURNED WITH DIAGNOSIS OF PNEUMONIA AND IS CURRENTLY RECEIVING ROCEPHIN The Totals are for all patients in facility : Average Number of Maintenance per Patient Average Number of PRN per Patient Average Number of Drugs per Patient 4.6 1.7 6.3 Sincerely, ______________________________________ Consultant Pharmacist 13.23 ICF –DD QUARTERLY PROGRESS REPORT (SAMPLE) Date : 12/31/2012 Name: Doctor: DOB: Status: Diet: JOHNSON, THOMAS ATHER 05/12/69 ADMIT 12/1/01 REGULAR Diagnosis: MENTAL RETARDATION, OBS W PSYCHOSIS, ESSTENTIAL TREMOR, RHINITIS Patient prefers to have meds crushed and in applesauce or pudding Misc Info: Station: Room: SOUTH 201B Lab Due Dates: ELECTROLYTES 02/12/12 Lab Due Dates: CHEM-30 02/12/12 Dec 31, 2012 Comments : General health remains stable at this time although tremor still noted. These fine tremors are unchanged in frequency or intensity and do not affect ADL’s. Dr Thomas provided annual eye exam on 11/4/12 – normal eye exam – no new orders. Dr. Adams provided psych review on 11/1/12. He notes Thomas is doing well on current orders for Thioridazine 100mg TID, Clonazepam 0.5mg TID and Benztropine 1mg TID – no new orders as of this review. Repeat psych review on 12/6 indicates some “weird” behaviors with an increase in “spaciness” and wandering. Dr Adams requested an EKG due to black box warning on Thioridazine. Elimite treatment completed on 11/30 and 12/6 for scabies outbreak. Infection resolved as of this review with no adverse effects from Elimite therapy. U/A and C&S was ordered on 12/10 for cloudy urine. Based on results of C&S Levaquin 500mg qd x 7days was ordered for UTI. Infection resolved by 12/17. EKG was completed on 12/18. Results were abnormal with suspect evidence of inferior infact. Referred to Dr Hogan (cardiologist) for consult. Dr Hogan has ordered echocardiogram but will not see patient until January 6th. Psych review meeting on 12/30 – discussed dc’ing Thioridazine due to cardiac issues however the team agreed that Thioridazine will be continued until after the cardiology workup is completed. Continue to monitor frequency of tremor and for EPS and TD secondary to Thioridazine therapy. DISCUS review should be completed before January 15th. Current therapy should not affect dietary requirements. There are no significant food-drug interactions noted. _____________________________________________ Edward Meyer - Consultant Pharmacist Date : 12/31/12 13.24 NURSING HOME SAMPLE REPORT QUARTERLY PHARMACY REVIEW OF SAMPLE FACILITY JULY 2012 THROUGH SEPTEMBER 2012 A Total of 55 Hours Of Consultant Time Was Spent In The Facility During This Quarter. A Total of 68 Recommendations Have Been Left This Quarter. These Recommendations Can Be Broken Down Into The Following Categories: 0 - Involved Missing Blood Pressures When Required 7 - Involved Missing Pulses When Lanoxin Was In Use 0 - Involved Missing Or Incomplete Diagnosis 27 -Involved Charting Omissions 2 - Involved Incomplete Documentation On Administered Prn's. 2 - Involved Suggested Changes In Current Therapy. 0 - Involved Suggested Lab Work 7 - Involved Missing Information On Prn Order 15 -Involved An Antipsychotic Order 8 - Involved An Anxiolytic Order I. PATIENT MEDICATIONS The meds were found to be well organized with current labels. There were minimal duplications noted. All liquid containers and liquid cabinets were found clean. No outdated patient meds were found this quarter. II. TREATMENT CARTS Treatment cabinets and carts were found very neat throughout the quarter. There were no outdated products found. All treatments contained current labels. No discontinued products were noted. III. REFRIGERATED MEDS All three refrigerators were found to be in the safe zone throughout the quarter. There was no frost build-up and no food products were found this quarter. Puncture dates and expiration dates on insulin and miacalcin remained clean this quarter. IV. MEDICATION RECORD SHEETS Medication sheets were in general neat and orderly. Charting omissions were down this quarter. The reporting of episodes and side effects on antipsychotic and anxiolytic flow sheets remains good during the past quarter. V. CONTROLLED SUBSTANCES Controlled substances were destroyed during August. VI. REFERENCE MATERIALS All needed reference materials are present at each nursing station. The procedure manual was completely reviewed and updated during september. VII. EMERGENCY BOXES All 3 EDK's were found to be in good order throughout the quarter. 13.25 VIII. PRESCRIPTION USAGE 1ST FLOOR 2ND FLOOR 3RD FLOOR JULY 8.6 6.7 9.4 AUGUST 8.6 6.3 9.3 SEPTEMBER 7.9 6.5 9.0 FACILITY AVERAGE 8.0 8.0 7.8 IX. PSYCHOACTIVE USE IN THE FACILITY PATIENTS % OF POP AS OF 12/2012 PATIENTS PATIENTS PATIENTS PATIENTS ON ANTIPSYCHOTICS ON ANXIOLYTICS ON ANTIDEPRESSANTS W O.B.S. OR DEMENTIA 22 28 30 79 18% 23% 25% 66% AS OF 9/12 PATIENTS PATIENTS PATIENTS PATIENTS ON ANTIPSYCHOTICS ON ANXIOLYTICS ON ANTIDEPRESSANTS W O.B.S. OR DEMENTIA 27 42 41 68 23% 35% 34% 57% AS OF 6/12 PATIENTS PATIENTS PATIENTS PATIENTS ON ANTIPSYCHOTICS ON ANXIOLYTICS ON ANTIDEPRESSANTS W O.B.S. OR DEMENTIA 21 40 34 70 17.5% 33% 28% 58% AS OF 3/12 PATIENTS PATIENTS PATIENTS PATIENTS ON ANTIPSYCHOTICS ON ANXIOLYTICS ON ANTIDEPRESSANTS W O.B.S. OR DEMENTIA 27 35 36 71 22.5% 29% 30% 59% SINCERELY, CONSULTANT PHARMACIST (Note: There is no standard format for the quarterly report. This represents just one example of how quarterly report can be structured.) SAMPLES OF CHARTING MATERIALS 13.26 13.27