* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 9/09 Aortic Regurgitation
Survey
Document related concepts
Transcript
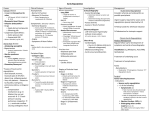
IMAGING CONFERENCE: AORTIC REGURGITATION September 16, 2009 Ali R. Rahimi, MD MPH Patient A: What is the Story? Patient B: What is the Story ? Patient B: Patient A: Patient A: Patient A: Patient B: Patient B: Patient B: Patient B: Patient B: Diagnosis Patient A 48 yo M PMH cocaine induced aortic arch dissection s/p repair c/b recurrent VRE AV (Bicuspid) Endocarditis and 2-3+ AR Mobile vegetation on LVOT side of Posterior Leaflet Patient B 47 yo M PMH AV (Bicuspid) Endocarditis c/b 4+ AR Two separate, mobile, moderate-sized vegetations (0.8cm x 0.5cm, 0.6cm x 0.6cm) located on the two leaflets of the aortic valve which prolapse across the LVOT during systole (larger vegetation on posterior leaflet) Aortic Regurgitation Diastolic reflux of blood from Aorta LV Incidence of clinically significant AR increases with age Typical peak in 4th to 6th decade of life More common in men than women Prevalence 4.9% in Framingham Heart Study Congenital or Acquired Caused by abnormalities of aortic root or AV Etiology Dilation of Aortic Root and Annulus Hypertension Marfan Syndrome Syphilitic Aortitis Cystic Medial Necrosis Aortic Dissection Osteogenesis Imperfecta Ankylosing Spondylitis Ehlers-Danlos Syndrome ≥ 2mm dilation at sinotubular junction can cause AR Etiology Aortic Valve Bicuspid Aortic Valve Rheumatic Heart Disease Degenerative Calcific AV Disease Infective Endocarditis Other Trauma Membranous Subaortic Stenosis Rheumatoid Arthritis Fenfluramine and Dexfenfluramine Deterioration of AVR Bioprosthesis Acute Aortic Regurgitation Most commonly due to endocarditis, aortic dissection, or blunt chest trauma Sudden large regurgitant volume imposed on LV Abrupt increase in LVEDV Rapid increase LVEDP & LAP Inability of ventricle to develop compensatory chamber dilatation acutely results in a decrease in forward SV Congestive Heart Failure, Myocardial Ischemia and/or Cardiogenic Shock Chronic Aortic Regurgitation Early Compensated Enlarged chamber size ↑ afterload hypertrophy of LV which preserves compliance normal filling pressures LVH ↑ LV mass normal LV vol/mass ratio & EF Progressive LV dilation and systolic HTN ↑ wall stress and vol/mass ratio ↑ wall stress eventually leads to overt LV dysfunction. Decompensated LV systolic dysfunction accompanied by decreased LV diastolic compliance due to hypertrophy and fibrosis Leads to high filling pressures and CHF symptoms Exertional dyspnea common; angina can occur due to reduced coronary flow reserve with predominantly systolic coronary flow Courtesy: Ali Mahajerin, MD Stages Bekerdjian R, et al. Circulation 2005; 112: 125-134 Physical Exam - Auscultation A2 often soft/absent, P2 normal S3 if LV function severely depressed High frequency decrescendo diastolic murmur over the 3rd or 4th intercostal space at left sternal border Best heard sitting up, leaning forward at end expiration Austin Flint murmur: mid-to-late diastolic apical rumble, possibly due to vibration of anterior mitral leaflet as it is struck by a posteriorly directed AR jet. Physical Exam - Peripheral Findings Corrigan’s pulse – bounding “waterhammer” carotid pulse deMusset’s sign – head bob with each heart beat Mueller’s sign – systolic pulsation of uvula Traube’s sign – pistol shot pulse over the femoral artery Duroziez’s sign – systolic and diastolic bruits heard when femoral artery partially compressed Becker’s sign – visible pulsations of retinal arteries and pupils Hill’s sign – popliteal cuff systolic pressure exceeding brachial pressure by more than 60 mmHg Mayne’s sign – more than 15 mmHg decrease in diastolic blood pressure with arm elevation Rosenbach’s sign – systolic pulsations of the liver Gerhard’s sign – systolic pulsations of the spleen Diagnosis and Initial Evaluation Class 1 Echo: confirm presence and severity of acute or chronic AR. (Level of Evidence: B) Echo: diagnosis and assessment of the cause of chronic AR (including valve morphology and aortic root size and morphology) and for assessment of LV hypertrophy, dimension (or volume), and systolic function. (Level of Evidence: B) Echo: in patients with an enlarged aortic root to assess regurgitation and the severity of aortic dilatation. (Level of Evidence: B) Echo: periodic re-evaluation of LV size and function in asymptomatic patients with severe AR. (Level of Evidence: B) Echo: re-evaluate mild, moderate, or severe AR in patients with new or changing symptoms. (Level of Evidence: B) **Radionuclide angiography or MRI: initial and serial assessment of LV volume and function at rest in patients with AR AND suboptimal echocardiograms. (Level of Evidence: B) Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 M-Mode Imaging Aortic jet across anterior MV creates High-frequency fluttering requiring rapid sampling rate Increased duration between E and A peaks Increased distance between the maximal anterior motion of MV in early diastole (E point) and the most posterior motion of the IVS (e.g., increased E-point septal separation) Acute AR premature closure of MV Rapidly increasing LVEDP M-Mode Imaging 2-Dimensional Imaging Focus on AV and Root Endocarditis Dissection Dilation Perivalvular leaks around aortic prosthesis Assessment of LV size and function Dilation Response to volume overload 2-Dimensional Imaging AVR - Dilated Aortic Root Marfans - Dilated Aortic Root 2-Dimensional and Color Flow Aortic Regurgitation due to AV Endocarditis 2-Dimensional and Color Flow AV Prosthesis: Aortic Root Abscess and Perivalvular Regurgitation 2-Dimensional and Color Flow LV Dilated-Spherical due to Chronic Severe Aortic Regurgitation Doppler Imaging: Color Flow Critical since 2-D may at times be “unremarkable” despite severe aortic regurgitation Most common technique to visualize AR Sensitivity > 95% False negatives can occur in tachycardia with mild AR Frame rate allows only a few diastolic frames to be displayed Can be overcome by using CW -- has a higher sampling rate Specificity ~100% Detects even trivial AR Less than1% of normal subjects under age 40 10-20% of patients greater than age 60 Vast majority of individuals greater than age 80 Doppler Imaging: Color Flow Composed of 3 distinct segments: Proximal flow convergence zone = area of flow acceleration into the orifice Vena contracta = narrowest and highest velocity region of the jet at or just downstream from the orifice The jet itself occurs distal to the orifice in the LV cavity Measurement of the jet area or penetration into the LV cavity is not accurate in assessing AR severity, though: If jet width/LVOT width < 25% specific for mild AR If jet width/LVOT width > 65% specific for severe AR This works best when regurgitant orifice is relatively round in shape. Doppler Imaging: Vena Contracta The narrowest diameter of flow stream Independent of volume flow rate and driving pressure, relatively unaffected by instrument settings Narrow range of values though, so care needed to obtain optimal images. Ideal sample is: Perpendicular to jet width In zoom mode Narrow sector Minimum depth For AR, vena contracta can be measured in parasternal long-axis view preferably in zoom mode Doppler Imaging: Vena Contracta Vena contracta width of ≥ 6 mm correlates with severe AR (sensitivity 95%, specificity 90%) Vena contracta width of < 3 mm specific for mild AR Enriquez-Sarano M, et al. NEJM 2004; 351: 1539-1546. Doppler Imaging: Color Flow Mild Moderate Severe Doppler Imaging: Color Flow Jet Width/LVOT Width < 25% Mild MR Jet Width/LVOT Width > 65% Severe AR Bekerdjian R, et al. Circulation 2005; 112: 125-134. Doppler Imaging: Color Flow Limitations as indicator for AR severity: Eccentric jets entrained along LV wall Jet is 3-D thus need multiple planes Changes in instrument gain, color scale, transducer frequency and wall filters will affect AR appearance, independent of severity ROA in chronic AR usually decreases during diastole Thus temporal variability Tendency to overestimate since visualized jet area would reflect peak rather than mean orifice area Doppler Imaging: Pulsed Wave Relies on demonstration of turbulent flow in LVOT on ventricular side of AV Due to high AR velocity, aliasing occurs, with prescence of turbulence establishing the diagnosis Highly sensitive but requires methodical search for AR False-Positive in setting of Mitral Stenosis or Prosthetic MV with turbulent diastolic flow Assumption the AR is centrally located and can be tracked toward apex Holodiastolic flow reversal in descending aorta correlated with severe AR 2-Dimensional and Doppler Imaging Eccentric AR Jet Displacement of Anterior MV Doppler Imaging: Continuous Wave Due to high velocity AR jet, CW necessary for contour of the envelope to be recorded Density of jet ≈ volume of regurgitation Approximation of number of RBCs being sampled Velocity of AR jet and Rate of Deceleration of retrograde flow can be measured AR results in increased antegrade volume flow rate across AV, which is reflected in an increase in the antegrade velocity across the valve The greater the severity of AR, the higher the antegrade velocity across the AV Must also consider possibility of coexisting AS Helpful to distinguish AR from Mitral Stenosis Jet Based on velocity and contour of jet Doppler Imaging: Continuous Wave Compare AR signal to Antegrade Flow AR Antegrade Weak mild Equal severe Doppler Imaging: CW and PHT AR velocity reflects pressure gradient between aorta and LV throughout diastole Early diastole – gradient is the highest with velocity 4-6 m/sec, depending on BP Diastole progresses – gradient diminishes as aortic pressure decreases and LV pressure increases Mild AR – compliant LV allows a slow and modest increase in LVEDP and Ao EDP is maintained throughout AR velocity remains high and CW envelope appears flat Severe AR – increasing LVEDP and more rapid decrease Ao pressure leads to a more rapid decel of AR velocity Doppler Imaging: CW and PHT Flat slope (P1/2 > 500 msec) mild AR Steep slope (P1/2 < 200 msec) severe AR Limitations of pressure half-time assessment: Aortic compliance, BP, and LV size/compliance will affect measures Pressure half-time sensitive to chronicity of AR Acute AR leads to much shorter values than chronic AR when LV is dilated with increased compliance Thus, a rapid P1/2 is more indicative of acuity than severity Pressure half-time varies with SVR Vasodilators may shorten the pressure half-time even as the aortic regurgitant fraction improves. Doppler Imaging: CW and PHT Acute AR due to Aortic Dissection Chronic AR due to Ca AV disease Doppler Imaging: Regurgitant Volume and Fraction Can compare flow through AV versus MV or PV Stroke volume at any valve annulus is derived as the product of CSA and TVI of flow at the annulus In the absence of regurgitation, SV determinations at different sites should be equal In the presence of regurgitation of one valve, without any intracardiac shunt the flow through the affected valve is larger than the other valves RV is the difference between the two flows RF = RV/ Forward SV through the regurgitant valve Doppler Imaging: Regurgitant Volume and Fraction Regurgitant Volume (fraction): Mild: < 30cc (< 30%) Mild-Moderate: 30-44cc (30-39%) Mod-Severe: 45-59cc (40-49%) Severe: ≥60cc (≥50%) Limitations: Assumes normal flow through comparison valve Cannot be used in presence of shunts Sensitive to small measurement errors (measurement errors of the radius and tracing the VTI) Summary: Zoghbi WA, et al. JASE 2003; 16: 777-802 Serial Testing by Echocardiography If chronic nature of lesion uncertain and no initial surgical indication, should repeat exam and echo within 2-3 months after initial evaluation Asx, mild AR, little/no LV dilation, normal LV systolic function: see yearly, echo q2-3 years Asx, severe AR, significant LV dilation (LVEDD > 60 mm), normal LV fx: echo q6-12 months Asx, severe AR, severe LV dilation (LVEDD > 70 mm), normal LV fx: echo q4-6 months. Repeat echo for onset of symptoms, equivocal history of changing symptoms or exercise tolerance, or clinical findings to suggest worsening regurgitation or progressive LV dilatation. Bonow RO, et al. J Am Coll Cardiol, 2008; 52:1-142 Management Strategy for Patients With Chronic Severe Aortic Regurgitation Bonow, R. O. et al. J Am Coll Cardiol 2008;52:e1-e142 Copyright ©2008 American College of Cardiology Foundation. Restrictions may apply. THANK YOU