* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download APPENDIX The Cytochrome P450 System
Compounding wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Metalloprotease inhibitor wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug design wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Drug discovery wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
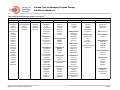
APPENDIX The Cytochrome P450 System Contents SUBSTRATES ..............................................................................................................................4 INHIBITORS...............................................................................................................................7 INDUCERS ..................................................................................................................................8 REFERENCES ..............................................................................................................................9 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook The Cytochrome P450 System Cytochrome P450 (CYP450) is a “superfamily” of more than 100 enzymes found in greatest abundance in the liver and small intestine, although they are also found in the kidneys, lungs, and other organs.1,2 The number 450 refers to a spectrographic measure of the enzymes’ pigment.3 About 30 of these enzymes are largely responsible for metabolism of many drugs in the pharmaceutical armamentarium today.1 CYP450 enzymes are principally active in Phase I of drug metabolism, which involves oxidation and reduction of lipophilic drugs to hydrophilic compounds prior to excretion.4 The most important CYP450 enzymes involved in drug metabolism include those designated CYP1A2, CYP2C9, CYP2C19, CYP2D6, CYP2E1, and the CYP3A subfamily, including 3A4, 3A5, and 3A7.1,2,4 The nomenclature used to identify CYP450 enzymes is not as confusing as it may at first appear. The CYP designation is followed by a number that identifies the gene family to which the particular enzyme belongs. That number is followed by a letter that designates the subfamily (if there is more than one). The final number designates the individual gene, within the subfamily.5 Whereas many drugs serve as substrates of CYP450 enzymes, others are enzyme inducers or inhibitors. A substrate is a drug that is metabolized by an enzyme. An inhibitor is a drug that slows the activity of an enzyme. Inhibiting the activity of an enzyme has the effect of increasing the plasma concentrations of drugs that are substrates of that enzyme. Drugs that are inducers of a given enzyme increase the metabolizing activity of that enzyme. This generally dilutes the effect of drugs that are substrates of that enzyme by increasing the rate at which they are metabolized and excreted.5,6 A notorious historical example of CYP450 drug interactions involved the antihistamine terfenadine.6,7 Terfenadine is a substrate of the CYP3A4 enzyme. The antifungal agent ketoconazole is a CYP3A4 inhibitor. Taking the two drugs concurrently sometimes resulted in high plasma concentrations of terfenadine, and some patients experienced serious cardiac arrhythmias as a result. Similar reactions sometimes occurred when terfenadine was taken concurrently with the antibiotic erythromycin, also a CYP3A4 inhibitor.1 Ultimately, terfenadine was withdrawn from the market. Clinicians should also keep in mind that there are individual differences in rates of drug metabolism. Because of their genetic makeup, some people break down certain drugs more slowly than normal (“poor metabolizers”) and therefore may be at increased risk of side effects. Others break down certain drugs more rapidly than normal (“ultra-extensive metabolizers”) and therefore may need a higher dosage. People who metabolize drugs “normally” are often called “extensive metabolizers.”8,9 Clinical trials are increasingly incorporating genotyping to evaluate this issue. Some of these polymorphisms are characteristic of particular ethnic groups. For example, about 7% to 10% of whites are recognized as poor metabolizers of drugs that are substrates of the CYP2D6 enzyme,2 compared with 4% of African Americans and <1% of Asians.1 Patients with that deficiency will have limited ability to metabolize CYP2D6 substrates (eg, many psychotropic drugs) and may Appendix. The Cytochrome P450 System Page 2 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook therefore experience toxicity even at normal doses.1 In addition, they may have difficulty converting prodrugs (eg, codeine) that are metabolized by CYP2D6 to their active metabolite, and thus may receive little or no pharmacologic benefit from those drugs.1 As noted in earlier chapters of this handbook, many of the targeted therapies used to treat solid tumors are substrates, inhibitors, or inducers of CYP450 enzymes, and thus have potential interactions with other drugs that are also substrates, inhibitors, or inducers of CYP450 enzymes. The Table can serve as a reference for determining how other commonly used drugs might be expected to affect targeted therapies. Listed are the most prominent and clinically significant CYP450 enzymes and drugs that are substrates, inhibitors, and/or inducers of each (Table).10 Appendix. The Cytochrome P450 System Page 3 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook Table. Cytochrome P450 Substrates, Inhibitors, and Inducers.10 Substrates 1A2 2B6 2C8 2C19 2C9 2D6 2E1 3A4,5,7 Acetaminophen Amitriptyline Caffeine Clomipramine Clozapine Cyclobenzaprine Estradiol Fluvoxamine Haloperidol Imipramine Mexiletine Naproxen Olanzapine Ondansetron Phenacetin Propranolol Riluzole Ropivacaine Tacrine Theophylline Tizanidine Verapamil R-warfarin Zileuton Zolmitriptan Bupropion Cyclophosphamide Efavirenz Ifosfamide Methadone Amodiaquine Cerivastatin Paclitaxel Repaglinide Torsemide Proton Pump Inhibitors E-3810 Lansoprazole Omeprazole Pantoprazole Rabeprazole NSAIDs Diclofenac Ibuprofen Lornoxicam Meloxicam S-naproxen Piroxicam Suprofen Beta Blockers Carvedilol S-metoprolol Timolol Anesthetics Enflurane Halothane Isoflurane Methoxyflurane Sevoflurane Macrolide Antibiotics Clarithromycin Erythromycin Telithromycin Miscellaneous Acetaminophen Aniline Benzene Chlorzoxazone Ethanol N,N-dimethylformamide Theophylline Anti-arrhythmics Quinidine Appendix. The Cytochrome P450 System Anti-epileptics Diazepam Phenobarbitone Phenytoin S-mephenytoin Miscellaneous Amitriptyline Carisoprodol Citalopram Chloramphenicol Clomipramine Clopidogrel Cyclophosphamide Hexobarbital Imipramine Indomethacin R-mephobarbital Moclobemide Nelfinavir Nilutamide Primidone Progesterone Proguanil Oral Hypoglycemic Agents Glipizide Tolbutamide Angiotensin II Blockers Irbesartan Losartan Sulfonylureas Glimepiride Glipizide Glyburide/glibenclamide Tolbutamide Miscellaneous Amitriptyline Celecoxib Fluoxetine Fluvastatin Glyburide Nateglinide Antidepressants Amitriptyline Clomipramine Desipramine Imipramine Paroxetine Antipsychotics Haloperidol Perphenazine Risperidone Thioridazine Zuclopenthixol Miscellaneous Alprenolol Amphetamine Aripiprazole Atomoxetine Bufuralol Chlorpheniramine Chlorpromazine Codeine Debrisoquine Dexfenfluramine Dextromethorphan Duloxetine NOT azithromycin Benzodiazepines Alprazolam Diazepam Midazolam Triazolam Immune Modulators Cyclosporine Tacrolimus HIV Antivirals Indinavir Nelfinavir Ritonavir Saquinavir Antihistamines Astemizole Chlorpheniramine Terfenadine Page 4 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook Substrates (cont.) 1A2 2B6 2C8 2C19 2C9 2D6 Propranolol Teniposide R-warfarin Phenytoin Rosiglitazone Tamoxifen Torsemide S-warfarin Encainide Flecainide Fluoxetine Fluvoxamine Lidocaine Metoclopramide Methoxyamphetamine Mexilletine Minaprine Nebivolol Nortriptyline Ondansetron Oxycodone Perhexiline Phenacetin Phenformin Promethazine Propafenone Propranolol Sparteine Tamoxifen Tramadol Venlafaxine 2E1 3A4,5,7 Calcium Channel Blockers Amlodipine Diltiazem Felodipine Lercanidipine Nifedipine Nisoldipine Nitrendipine Verapamil HMG CoA Reductase Inhibitors Atorvastatin Cerivastatin Lovastatin Simvastatin NOT pravastatin NOT rosuvastatin Steroid 6beta-OH Estradiol Hydrocortisone Progesterone Testosterone Miscellaneous Alfentanyl Aprepitant Aripiprazole Buspirone Cafergot Caffeine Cilostazol Appendix. The Cytochrome P450 System Page 5 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook Substrates (cont.) 1A2 2B6 2C8 2C19 2C9 2D6 2E1 3A4,5,7 Cinacalcet Cocaine Codeine-N-demethylation Dapsone Dexamethasone Dextromethorphan Docetaxel Domperidone Eplerenone Ergotamine/dierGotamine Fentanyl Finasteride Haloperidol Irinotecan LAAM Lapatinib Lidocaine Methadone Nateglinide Ondansetron Pimozide Propranolol Quetiapine Quinine Risperidone Salmeterol Sildenafil Sirolimus Tamoxifen Taxol Terfenadine Trazodone Vincristine Zaleplon Ziprasidone Zolpidem Appendix. The Cytochrome P450 System Page 6 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook Inhibitors 1A2 2B6 2C8 2C19 2C9 2D6 2E1 3A4,5,7 Amiodarone Cimetidine Ciprofloxacin Fluoroquinolones Fluvoxamine Furafylline Interferon Methoxsalen Mibefradil Thiotepa Ticlopidine Gemfibrozil Glitazones Montelukast Quercetin Trimethoprim Proton Pump Inhibitors Lansoprazole Omeprazole Pantoprazole Rabeprazole Amiodarone Fenofibrate Fluconazole Fluvastatin Fluvoxamine Isoniazid Lovastatin Phenylbutazone Probenicid Sertraline Sulfamethoxazole Sulfaphenazole Teniposide Voriconazole Zafirlukast Amiodarone Bupropion Celecoxib Chlorpheniramine Chlorpromazine Cimetidine Cinacalcet Citalopram Clemastine Clomipramine Cocaine Diphenhydramine Doxepin Doxorubicin Duloxetine Escitalopram Fluoxetine Goldenseal Halofantrine Histamine H1 receptor antagonists Hydroxyzine Levomepromazine Methadone Metoclopramide Mibefradil Midodrine Moclobemide Paroxetine Perphenazine Quinidine Ranitidine Red-haloperidol Ritonavir Sertraline Diethyldithiocarbamate Disulfiram HIV Antivirals Atazanavir Indinavir Nelfinavir Ritonavir Saquinavir Appendix. The Cytochrome P450 System Miscellaneous Chloramphenicol Cimetidine Felbamate Fluoxetine Fluvoxamine Indomethacin Ketoconazole Modafinil Oxcarbazepine Probenicid Ticlopidine Topiramate Miscellaneous Amiodarone Aprepitant Chloramphenicol Delaviridine Cimetidine Clarithromycin Diethyl-dithiocarbamate Diltiazem Erythromycin Fluconazole Fluvoxamine Gestodene Grapefruit, grapefruit juice Imatinib Itraconazole Ketoconazole Mibefradil Mifepristone Nefazodone Norfloxacin Norfluoxetine Star fruit Telithromycin Troleandomycin (TAO) Verapamil Voriconazole Page 7 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook Inhibitors (cont.) 1A2 2B6 2C8 2C19 2C9 2D6 2E1 3A4,5,7 Terbinafine Ticlopidine Tripelennamine Inducers 1A2 2B6 2CB 2C19 2C9 2D6 2E1 3A4,5,7 Broccoli Brussels sprouts Char-grilled meats Insulin Methylcholanthrene Modafinil Nafcillin Betanaphthoflavone Omeprazole Tobacco Phenobarbital Rifampin Rifampin Carbamazepine Norethindrone Prednisone Rifampin Rifampin Secobarbital Dexamethasone Rifampin Ethanol Isoniazid HIV Antivirals Efavirenz Nevirapine NOT pentobarbital Miscellaneous Barbiturates Carbamazepine Dexamethasone Glucocorticoids Modafinil Oxcarbazepine Phenobarbital Phenytoin Pioglitazone Rifabutin Rifampicin Rifapentine Rifampin St. John’s wort Troglitazone With permission from Flockhart DA. Drug Interactions: Cytochrome P450 Drug Interaction Table. Indiana University School of Medicine (2007). Appendix. The Cytochrome P450 System Page 8 Caring for Oncology Patients Tips and Tools for Managing Targeted Therapy Side Effects eHandbook References 1. Brown CH. Overview of drug interactions modulated by cytochrome P 450. U.S. Pharmacist. 2001;26:HS26-HS45. 2. Cupp MJ, Tracy TS. Cytochrome P450: new nomenclature and clinical implications. Am Fam Physician. 1998;57:107-116. 3. International Society for the Study of Xenobiotics. Cytochrome P450. Available at: http://www.issx.org/i4a/pages/index.cfm?pageid=3352. Accessed October 1, 2008. 4. Food and Drug Administration. Preventable adverse drug reactions: a focus on drug interactions. Available at: http://www.fda.gov/CDER/DRUG/drugReactions/. Accessed October 1, 2008. 5. Beaird S. HMG-CoA reductase inhibitors: assessing differences in drug interactions and safety profiles. J Am Pharm Assoc. 2000;40:637-644. 6. NursingLink. Clinically significant drug interaction with the cytochrome P450 enzyme system. Available at: http://www.nursinglink.com/training/articles/320-clinically-significant-drug-interaction-with-the-cytochrome-p450-enzymesystem. Accessed October 1, 2008. 7. Food and Drug Administration. Seldane (terfenadine) [press release]. Available at: http://www.fda.gov/bbs/topics/NEWS/NEW00286.html. Accessed October 1, 2008. 8. Flockhart DA, Tanus-Santos TE. Implications of cytochrome P450 interactions when prescribing medication for hypertension. Arch Intern Med. 2002;162:405-412. 9. Genelex. DNA drug reaction profile test results: cytochrome P450 2D6 test. Available at: http://www.healthanddna.com/2D6poormetabolizer.pdf. Accessed October 1, 2008. 10. Flockhart DA. Drug interactions: cytochrome P450 drug interaction table. Available at: http://medicine.iupui.edu/flockhart/table.htm. Accessed October 1, 2008. Appendix. The Cytochrome P450 System Page 9










![[4-20-14]](http://s1.studyres.com/store/data/003097962_1-ebde125da461f4ec8842add52a5c4386-150x150.png)