* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Absolute and relative exercise risk for patients with arrhythmias
Heart failure wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
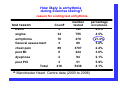
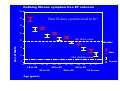
BACR Conference Exercise risk for patients with arrhythmias: a safe and pragmatic approach Prof. Patrick Doherty [email protected] Question? – Are all patients with arrhythmia and those with an ICD truly high risk? – We know exercise is effective so why not allow patients with arrhythmia to be benefit? – Is it safe? • Does the type of exercise matter – How to exercise with reduced risk? Why is exercise still considered risky: Paradox! A lack of regular physical activity and exercise carries a higher risk for early heart disease and premature death. However, sometimes trained and apparently healthy athletes die suddenly during or immediately following exercise For example James Fixx, the celebrated American marathon runner wrote, prior to his premature death from a MI, "...runners are much like ordinary mortals. They can, sad to say, get sick. They can even die” Arrhythmia risk in people presumed healthy: USA data on marathon running (vigorous by any definition) over a 30-year period (215,413 runners) found the overall prevalence of sudden cardiac death during the marathon was thus 0.002%, strikingly lower than for several other variables of risk for premature death. The authors concluded that: Although highly trained athletes may harbor underlying and potentially lethal cardiovascular disease, the risk of sudden cardiac death associated with marathon running was exceedingly small (1 in 50,000) Timothy D Noakes http://www.sportsci.org/jour/9804/tdn.html How often and where does arrhythmia occur? • Sudden Cardiac Arrest (SCA) occurs at a maximum rate of 100,000 per year in the UK with a 5% survival rate • 80% of arrhythmias are due to ventricular tachyarrhythmia and HEART FAILURE is strongly associated with arrhythmia (Bryant et al 2005, HTA Review) • Question. Is exercise to blame for this rate of death: • Answer: NO • Why: Because 70% of UK adults are considered sedentary so exercise, alone, can’t explain the incidence of SCA What does the literature say about the likelihood of cardiac events with exercise Beckerman et al (2005) more often than not only vigorous testing and vigorous exercise is effective at provoking arrhythmias. Pina et al 2003: between 4 to 20% of MI’s occur during or soon after exercise and the risk increases in persons who do not regularly exercise Pigozzi et al (2004) found that vigorous exercise training is not associated with prevalence of ventricular arrhythmias in elderly athletes. Lauer et al (2005) Men whose heart rate decreased less than 25 beats in the minute after they stopped the exercise test more than doubled their risk of sudden death than those whose rate returned to normal faster. Thompson et al (2003) approximately 5% to 10% of myocardial infarctions are associated with vigorous physical activity in novice performers Belardinelli R. (2003) Exercise can induce or prevent arrhythmias dependent on dose Conclusion: The relative risk of both exercise-related myocardial infarction and sudden death, due to cardiac arrest, is greatest in individuals who are the least physically active and perform unaccustomed vigorous physical activity Greatest risk: exercise or sedentary periods Normal sleep: Bradyarrhythmias consisting of sinus bradycardia, sinus arrest and second degree heart block are not uncommon in young adults Corrado et al (2001) With aging, bradyarrhythmias decrease in frequency while atrial arrhythmias and ventricular ectopy increase (Nademanee et al (1997) Shepard (1992) NEGRUSZ-KAWECKA et al (1999) Sedentary behaviour: People with cardiac disease are seven times more likely to die suddenly during sedentary activities than during jogging (moderate activity) Giri et al (1999) The rate MI with vigorous exertion was 12 times higher than at rest, and the risk was greatest among the least active Holter monitoring of daily activity, including rest, is more effective, than exercise testing, at revealing cardiac arrhythmia Arrhythmia risk cont. • Although some ARVC/D patients may demonstrate exercise induced, catecholamine related, arrhythmias those with right ventricular anterior wall involvement share, along with patients with Brugada, a propensity to die from non-exercise-related cardiac arrest (Corrado et al., 2001) • Among 112 patients with sustained ventricular tachycardia, 15 (14%) were found to have exercise-induced symptomatic ventricular tachycardia. Re-entry at any time of the day or night is the most likely electrophysiologic mechanism (RODRIGUEZ et al 1990) • Between 1981 and 1988, the Centers for Disease Control and Prevention reported a very high incidence of sudden death among young male Southeast Asians who died unexpectedly during sleep. The pattern of death has long been prevalent in Southeast Asia and is associated with Right bundle-branch block Nademanee et al., (1997) • Habitual snoring has long been associated with an increased risk of sudden death during sleep. In patients with clinically significant obstructive sleep apnoea, there is reasonable information indicating excessive mortality in the absence of treatment. This mortality is predominantly cardiovascular and tends to occur during sleep. Shepard, (1992) Factors that influence the likelihood of arrhythmia during exercise Autonomic neural dominance Circulating catecholamines A Hemodynamics L T E R Psychological state E Cardiac condition D Metabolism Electro physiology Arrhythmia Reduced parasympathetic tone (start of exercise) Developed from: Young et al (1984), Gibbons et al (1989), Pashkow et al (1997) 9 How likely is arrhythmia during Exercise testing? reason for ending test arrhythmia DVLA Count 3 number tested 149 percentage occurance 2.0% angina 34 755 4.5% arrhythmia 76 279 27.2% General assessment 3 80 3.8% chest pain 89 3707 2.4% post MI 8 224 3.6% dyspnoea 2 94 2.1% post PCI 3 51 5.9% 218 5339 4.1% a test reason Total a. Manchester Heart Centre data (2000 to 2006) Is cardiac rehab exercise safe? • One nonfatal cardiac complication per 35,000 patient hours of exercise participation (Haskell 1978) • One fatal event for every 116,000 patient hours of exercise participation • How does it compare to cardiology exercise testing: – Four non-fatal complications per 10,000 • (Fletcher et al 2001) • Why such a difference? ***CR exercise is much easier than vigorous exercise testing Important points from the literature and clinical settings: • Most patients referred with arrhythmia tend to end the test due to fatigue • Approximately 1:4 cardiac patients referred with arrhythmia will demonstrate arrhythmias during or shortly after exercise • Exercise arrhythmias tend to occur at relatively high levels of aerobic fitness (>8METs) or cardiac demand (RPP>280) • A very small percentage of patients referred with chest pain are likely to end the test due to arrhythmia • Patients unaccustomed to vigorous exercise have a far higher likelihood of exercise induced arrhythmia • Immediate cessation of strenuous exercise is an arrhythmia provoking situation ICD patients have taught us plenty about exercise and arrhythmia Arrhythmia & ICD: Points to consider prior to exercise • Adapt ET protocol and exercise regime so that warm up and cool down are default characteristics • Essential information required prior to exercising: – ICD parameters: • • • • • – VT or VF settings including SVT criteria ATP or Shocks therapy Detection threshold Rapid onset criteria Sustained rhythm criteria Beta blockade usage and dose Doherty, P (2006) British Journal of Cardiac Nursing, 1(7):327-31 ICD scrutiny during exercise 2. Comparison of: •ECG intervals •Atria vs ventricle rate •VT or VF rate Heart rate (bpm) 250 200 1. ICD threshold e.g 190 bpm 150 3. Onset 4. Stability over time 100 50 1 2 3 4 5 6 Exercise time (minutes) 7 8 9 Important aspects of the exercise session • Warm-up and cool down period, lasting between 10 to 15 minutes, so that the cardiovascular system has time to adjust to increasing demand (Fletcher et al., 2001, Pina et al., 2003) • The main part of the training programme should consist of: – graded aerobic circuit training approaches, lasting 30 to 40 minutes – incorporate multijoint movements with body weight and moderate resistance – Pacing and rating their own exertion is very important • (ACSM, 2006a, Duncan et al., 2005, Fitchet et al., 2003, Fletcher et al., 2001, Lampman and Knight, 2000, Pashkow et al., 1997). Exercise dose response • Frequency and intensity relationship – RCT of intensity and frequency in 492 sedentary, healthy ♂ & ♀aged between 40 and 60 years, • walking was the primary intervention Duncan et al. (2005). – Walking (hard or moderate intensity) led to significant improvement in fitness (10%) and improved lipid profile, over two years – This raises questions about how fit people need to be? Defining fitness: symptom free ET outcome 18 How fit does a patient need to be? 16 14 12 UK, DVLA value 95% CI METs 10 Gender 8 Male 6 USA disability value Female 4 N= 77 34 190 92 18 to 29 351 154 391 202 40 to 49 30 to 39 Age (years) 218 130 92 64 60 to 69 50 to 59 70 & over Exercise considerations (cont) • In general most exercises should be performed in standing, with horizontal and seated arm exercises kept to a minimum. • Seated arm exercise is associated with: – reduced venous return, reduced end diastolic volume, a concomitant decrease in cardiac output and increased likelihood of arrhythmia (Fitchet et al., 2003, Lampman and Knight, 2000, Pashkow et al., 1997). – If seated exercise is to be performed: • the intensity of exercise should be lowered • the emphasis placed on muscular endurance. • Mild leg exercise combined with arm exercise, reduces the haemodynamic response compared with strict arm work (Toner et al., 1990). • Breath holding and sustained isometric muscle work of the abdominal region, especially during arm exercise, needs to be kept to a minimum in patients with low FC and arrhythmia risk Meeting the minimum requirements for health • Continuous physical activity of 30 minutes or more is considered most effective, although multiple activity sessions of 10 to 15 minutes duration, on the same day, have also demonstrated significant health improvement (ACSM, 2006a, Blair et al., 2004, Fletcher et al., 2001). • Physical fitness is soon lost if training is not continued at a level sufficient to maintain the effect (ACSM, 2006a, Fitchet et al., 2003, Fletcher et al., 2001, Franco et al., 2005, Pina et al., 2003, Rees et al., 2004). • You need to be sure that patients have considered how and where they will continue their moderate physical activity programme when they finish with you. Summary • Arrhythmia or the presence of an ICD should not preclude patients from exercise • An evidence based CR exercise session is very safe and highly effective • The risk of arrhythmias within well designed, moderate intensity, exercise programmes in far less than the risk encountered as part of a normal daily life • At the very least all patients should be advised about physical activity: – – – – Benefits Safe exercise principles Best practice Need for a sustained approach • If you don’t advise them no one else will!! • Thank you for listening! • Bibliography • (ACSM), A. C. O. S. M. (2005) Guidelines for Exercise Testing and Prescription, Philadelphia, Lippincott Williams & Wilkins. BECKERMAN, J., WU, T., JONES, S. & FROELICHER, V. F. (2005) Exercise testinduced arrhythmias. Prog Cardiovasc Dis, 47, 285-305. BELARDINELLI, R. (2003) Arrhythmias during acute and chronic exercise in chronic heart failure. International journal of cardiology, 90, 213-8. BLAIN, G., MESTE, O. & BERMON, S. (2005) Influences of breathing patterns on respiratory sinus arrhythmia in humans during exercise. Am J Physiol Heart Circ Physiol, 288, H887-95. BLAIR, S. N., LAMONTE, M. J. & NICHAMAN, M. Z. (2004) The evolution of physical activity recommendations: how much is enough? Am J Clin Nutr, 79, 913S920S. BRYANT, J., BRODIN, H., LOVEMAN, E., PAYNE, E. & CLEGG, A. (2005) The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review. Health Technol Assess, 9, 1-150, iii. CORRADO, D., BASSO, C., BUJA, G., NAVA, A., ROSSI, L. & THIENE, G. (2001) Right bundle branch block, right precordial st-segment elevation, and sudden death in young people. Circulation, 103, 710-7. EMPANA, J. P., JOUVEN, X., LEMAITRE, R. N., SOTOODEHNIA, N., REA, T., RAGHUNATHAN, T. E., SIMON, G. & SISCOVICK, D. S. (2006) Clinical depression and risk of out-of-hospital cardiac arrest. Arch Intern Med, 166, 195-200. • • • • • • • • • • • • • • • • • FITCHET, A., DOHERTY, P. J., BUNDY, C., BELL, W., FITZPATRICK, A. P. & GARRATT, C. J. (2003) Comprehensive cardiac rehabilitation programme for implantable cardioverter-defibrillator patients: a randomised controlled trial. Heart, 89, 155-60. FLETCHER, G. F., BALADY, G. J., AMSTERDAM, E. A., CHAITMAN, B., ECKEL, R., FLEG, J., FROELICHER, V. F., LEON, A. S., PINA, I. L., RODNEY, R., SIMONS-MORTON, D. A., WILLIAMS, M. A. & BAZZARRE, T. (2001) Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation, 104, 1694-740. LAMPMAN, R. M. & KNIGHT, B. P. (2000) Prescribing exercise training for patients with defibrillators. Am J Phys Med Rehabil, 79, 292-7. NADEMANEE, K., VEERAKUL, G., NIMMANNIT, S., CHAOWAKUL, V., BHURIPANYO, K., LIKITTANASOMBAT, K., TUNSANGA, K., KUASIRIKUL, S., MALASIT, P., TANSUPASAWADIKUL, S. & TATSANAVIVAT, P. (1997) Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation, 96, 2595-600. NEGRUSZ-KAWECKA, M. & ZYSKO, D. (1999) [Studies of arrhythmia incidence and heart rate variability in patients with stable angina pectoris]. Pol Arch Med Wewn, 101, 15-22. PASHKOW, F. J., SCHWEIKERT, R. A. & WILKOFF, B. L. (1997) Exercise testing and training in patients with malignant arrhythmias. Exerc Sport Sci Rev, 25, 235-69. PIGOZZI, F., ALABISO, A., PARISI, A., DI, S. V., DI, L. L. & IELLAMO, F. (2004) Vigorous exercise training is not associated with prevalence of ventricular arrhythmias in elderly athletes. The Journal of sports medicine and physical fitness, 44, 92-7. PINA, I. L., APSTEIN, C. S., BALADY, G. J., BELARDINELLI, R., CHAITMAN, B. R., DUSCHA, B. D., FLETCHER, B. J., FLEG, J. L., MYERS, J. N. & SULLIVAN, M. J. (2003) Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation, 107, 121025. RODRIGUEZ, L. M., WALEFFE, A., BRUGADA, P., DEHARENG, A., LEZAUN, R., STERNICK, E. B. & KULBERTUS, H. E. (1990) Exercise-induced sustained symptomatic ventricular tachycardia: incidence, clinical, angiographic and electrophysiologic characteristics. Eur Heart J, 11, 225-32. SHEPARD, J. W., JR. (1992) Hypertension, cardiac arrhythmias, myocardial infarction, and stroke in relation to obstructive sleep apnea. Clin Chest Med, 13, 437-58.