* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pharyngitis - Michele Jones`Professional Portfolio
Survey
Document related concepts
Transcript
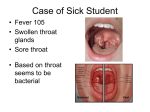
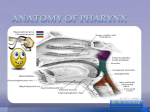
Pharyngitis Michele Morrison BS RN CCRN State University of New York Polytechnic Institute Family Primary Health Care I October 2016 What is pharyngitis? • Inflammation of the pharynx • “Sore throat” • Can be infectious, does not have to be (Dunphy, Winland-Brown, Porter, & Thomas, 2011) Etiology Caused by viral infection Caused by bacterial infection • • • • • • • • • • • Group A beta hemolytic streptococcus • Gonorrhea • Chlamydia • Corynebacterium • Diptheria • Mycoplasma pneumoniae • Pertussis • Tonsillitis Measles Adenovirus (common cold) Chickenpox Croup Influenza Mononucleosis HIV Rhinovirus Coronavirus Cocksackie virus Other cause: • Second-hand smoke • Kawasaki disease (Martel & Cherney, 2015) (Dunphy, Winland-Brown, Porter, & Thomas, 2011) Pathophysiology • Infective cause enters pharyngeal mucosa • Inflammation • Nasal secretions (Dunphy, Winland-Brown, Porter, & Thomas, 2011) Incidence • • • • • • • • 11 million people annually Adults 2x/year Children 5x/year 40-60% viral 15% strep 10% strep in adults (once every 8 years) 20-30% strep in children (once every 4 years) Increased occurrence during colder weather (30%) (Linder, Chan, & Bates, 2006) Screening and Risk Factors Screening • Assess if high risk patient for strep pharyngitis • History of rheumatic fever • Close contact with person with history of rheumatic fever • AHRQ algorithm • Modified Centor Score (Clinical Alignment and Performance Excellence University of Michigan, 2013) (Karla, Higgins, & Perez, 2016) Risk Factors • Frequent cough • Exposure to inhaled toxins (exhaust, cleaning fluids) • Illnesses that cause pharyngitis • Environmental allergies • Smoke • Immunocompromised • Increased stress • Alcohol in excess • Age (5-15) (Dunphy, Winland-Brown, Porter, & Thomas, 2011) (Bisno, Gerber, Gwaltney, Kaplan, & Schwartz, 2002) (Clinical Alignment and Performance Excellence University of Michigan, 2013) (Clinical Alignment and Performance Excellence University of Michigan, 2013) Modified Centor Score • http://www.mdcalc.com/modified-centorscore-for-strep-pharyngitis/ Clinical Findings • • • • • • • Sore throat Scratchy throat Throat red Throat edema Throat white spots or exudate Difficulty swallowing Painful swallowing (U.S. Department of Health and Human Services, 2013) Clinical Findings • • • • • Fever Swollen tonsils Tonsillar exudate Anterior cervical lymphadenopathy Cervical lymph node tenderness • NO cough, conjunctivitis, rhinorrhea if bacterial (U.S. Department of Health and Human Services, 2013) (Vincent, Celestin, & Hussain, 2004) Clinical Findings Group A Streptococcus Pharyngitis • • • • Pharyngeal swelling Tonsillar swelling Petechiae on palate Anterior cervical lymphadenopathy (Vincent, Celestin, & Hussain, 2004) Differential Diagnosis VIRAL INFECTIONS • • • • • • • • • • Measles Adenovirus (common cold) Chickenpox Croup Influenza Mononucleosis HIV Rhinovirus Coronavirus Cocksackie virus (Martel & Cherney, 2015) (Dunphy, Winland-Brown, Porter, & Thomas, 2011) Differential Diagnosis • • • • • • • • BACTERIAL INFECTIONS Group A beta hemolytic streptococcus Gonorrhea Chlamydia Corynebacterium Diptheria Mycoplasma pneumoniae Pertussis Tonsillitis (Martel & Cherney, 2015) (Dunphy, Winland-Brown, Porter, & Thomas, 2011) Social and Environmental Considerations • • • • • • Humans only reservoirs for group A strep Direct contact with infected person Saliva, nasal discharge 2-5 day incubation Crowded areas Generally not infectious after 24 hours of antibiotics • Stay home until afebrile for 24 hours (Centers for Disease Control and Prevention, 2016) Laboratory Tests and Diagnostics • Rapid antigen/rapid strep • Throat culture • Monospot test (Vincent, Celestin, & Hussain, 2004) Management Pharmacological Treatment Cough suppressant Acetaminophen Positive for Group A Strep Antibiotics (Centers for Disease Control and Prevention, 2016) Management Antibiotics for streptococcus pharyngitis Penicillin V: Children 250 mg po 2-3 times/day x 10 days Adults 250 mg po 4 times/day x 10 days Amoxicillin: 50 mg/kg once daily x 10 days Penicillin G: < 27 kg 600,000 units x 1 dose > 27 kg 1,200,000 units x 1 dose No reports of resistance to penicillin or amoxicillin Resistance noted to azithromycin and clarithromycin (Centers for Disease Control and Prevention, 2016) Management Antibiotic therapy with penicillin allergy Cephelexin: 20 mg/kg/dose po BID max 500 mg/dose x 10 days Cefadroxil: 30 mg/kg/dose (max 1 GM) po once daily x 10 days Clindamycin: 7 mg/kg/dose po TID max 300 mg/dose x 10 days Azithromycin: 12 mg/kg (max 500) po once daily x 5 days Clarithromycin: 7.5 mg/kg/dose (max 250/dose) po BID x 10 days (Centers for Disease Control and Prevention, 2016) Management Non-pharmacological Treatment Warm salt-water gargle Humidifier Fluids Rest Hot tea with honey and lemon (Linder, Chan, & Bates, 2006) Treatment Guidelines Viral • Warm salt-water gargle • Acetaminophen Bacterial • Antibiotics Surgery may be indicated to remove tonsils if associated with chronic infection Treatment Guidelines Infectious Disease Society of America Guidelines for initiating antibiotic therapy Patients at high risk for Group A strep – rapid antigen If rapid antigen positive – start antibiotics If rapid antigen negative – throat culture If throat culture positive – antibiotic therapy (Bisno, Gerber, Gwaltney, Kaplan, & Schwartz, 2002) Complications • • • • • Rheumatic fever Scarlet fever Peritonsillar abscess Glomerulonephritis Infectious mononucleosis – airway obstruction (Linder, Chan, & Bates, 2006) Follow-up • Worsening symptoms • Symptoms do not resolve • Recurrence (Karla, Higgins, & Perez, 2016) Counseling and Education • Avoid triggers (smoking, alcohol, crowded areas, contact with infected people) • Take full course of antibiotics • Use back-up contraception if on oral contraception and antibiotics • Incubation period 2-5 days • Transmitted via saliva and nasal secretions • Hand washing (Centers for Disease Control and Prevention, 2016) Consultation and Referral • Laryngoscopy if recurrent • ENT Consult if recurrent (Vincent, Celestin, & Hussain, 2004) Multiple Choice Questions 1. Which symptoms are associated with viral infectious causes of pharyngitis? A. cough, diarrhea, rhinorrhea B. Tonsillar exudate C. Anterior cervical adenopathy D. Positive throat culture Answer A. cough, diarrhea, rhinorrhea These are common symptoms associated with viral pharyngitis. The other choices are all associated with bacterial pharyngitis. Multiple Choice Questions 2. Which is not a common cause of pharyngitis? A. Group A streptococcus B. Anemia C. Adenovirus D. Cocksackie virus Answer B. Anemia Anemia is not known to cause pharyngitis Group A streptococcus is a common bacterial cause of pharyngitis Adenovirus and cocksackie virus are common viral causes of pharyngitis Multiple Choice Questions 3. What is the recommended first line treatment for group A streptococcus pharyngitis? A. Cephelexin B. Azithromycin C. Penicillin D. Levofloxacin Answer C. Penicillin Penicillin is the first choice for treatment of group A streptococcus pharyngitis Cephalexin and azithromycin are options if the patient has an allergy to penicillin Levofloxacin is not recommended for the treatment of group A streptococcus pharyngitis Multiple Choice Questions 4. Who is more likely to test positive for group A streptococcus pharyngitis? A. A 65 year old male with a cough and sore throat B. An 8 year old female with a fever and sore throat C. A 35 year old female with a sore throat and is a current every day smoker D. A 3 year old male with a sore throat with white patches on their tonsils Answer B. An 8 year old with fever and sore throat Group A streptococcus pharyngitis is most common in children 5-15 years and is associated with fever Patients 65 years old are unlikely to have group A strep and a cough is likely to have a viral cause A 35 year old is less likely to have group A strep and smoking is a cause of non-bacterial pharyngitis Positive group A strep is rare in a 3 year old Multiple Choice Questions 5. Which is a recommended treatment for pharyngitis with presumed viral etiology? A. Hot tea with honey and lemon B. Antibiotics C. Laryngoscopy D. Surgery Answer A. Hot tea with honey and lemon Supportive therapy is recommended for viral pharyngitis Antibiotics are not effective against viral infections Laryngoscopy and surgery are invasive and would not be warranted for a viral pharyngitis which is typically self-limiting Multiple Choice Questions 6. What is the pathophysiology that causes pharyngitis? A. Pharyngitis is not real, patients report having a sore throat to get out of work B. An infectious agent invades the pharyngeal mucosa causing irritation and inflammation C. Pharyngitis is only associated with tobacco use D. Pharyngitis is only associated with throat cancer Answer B. Pharyngitis is caused by an infectious agent that invades the pharyngeal mucosa Pharyngitis is a real diagnosis that is very common Tobacco and throat can cancer can increase the incidence of pharyngitis but are not the only cause Multiple Choice Questions 7. Group A streptococcus pharyngitis has been reported to have isolated strains resistant to which antibiotic? A. Penicillin B. Azithromycin C. Amoxicillin D. Clindamycin Answer B. Azithromycin Group A streptococcus pharyngitis is only known to have strains resistant to azithromycin and clarithromycin Multiple Choice Questions 8. Which is a complication of untreated group A streptococcus pharyngitis? A. Typhoid fever B. Yellow fever C. Rheumatic fever D. Cabin fever Answer C. Rheumatic fever Rheumatic fever is a known complication of untreated group A streptococcus Group A streptococcus is not associated with typhoid fever or yellow fever Multiple Choice Questions 9. Which is not a risk factor for group A streptococcus pharyngitis? A. Age 5-15 years B. Immunocompromised patient C. Contact with person infected with group A strep D. Age 65 years and older Answer D. Age 65 years and older The age group at highest risk for group A streptococcus is 5-15 years Immunosuppression and contact with people infected with group A strep increase the risk of becoming infected with group A strep Multiple Choice Questions 10.Which is a screening tool that can be used as a guide for testing and treatment of pharyngitis? A. Modified Centor Score B. Pharyngeal Assessment Tool C. Brown’s Sore Throat Measurement D. Wagner’s Strep Swallow Assessment Answer A. Modified Centor Score The Modified Centor Score was developed by Dr. Centor as a tool to determine patients at high risk for group A strep The other choices are not recognized assessment tools for pharyngitis THANK YOU! References • • • • • Centers for Disease Control and Prevention. (2016). Pharyngitis (strep throat). Retrieved from http://www.cdc.gov/groupastrep/diseases-hcp/strep-throat.html Clinical Alignment and Performance Excellence University of Michigan. (2013). Pharyngitis guidelines for clinical care: Ambulatory. Retrieved from http://www.med.umich.edu/1info/FHP/practiceguides/pharyngitis/pharyn.pdf Dunphy, L. M., Winland-Brown, J. E., Porter, B. O., & Thomas, D. J. (2011). Primary care: The art and science of advanced practice nursing (3rd ed.). Philadelphia, PA: F.A. Davis Company. Karla, M. G., Higgins, K. E., & Perez, E. D. (2016). Common questions about streptococcal pharyngitis. American Family Physician, 94(1), 24-31. Retrieved from www.aafp.org/afp Linder, J. A., Chan, J. C., & Bates, D. W. (2006). Evaluation and treatment of pharyngitis in primary care practice. Journal of American Medical Association, 166, 1374-1379. Retrieved from www.archinternmed.com References • • • Martel, J., & Cherney, K. (2015). Pharyngitis. Retrieved from http://www.healthline.com/health/pharyngitis U.S. Department of Health and Human Services. (2013). Pharyngitis. Retrieved from https://www.guideline.gov/summaries/summary/46947/pharyngitis Vincent, M. T., Celestin, N., & Hussain, A. N. (2004). Pharyngitis. American Family Physician, 69(6), 1465-1470. Retrieved from http://www.aafp.org/afp/2004/0315/p1465.html