* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Bradycardia and Pacing
Survey
Document related concepts
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Transcript
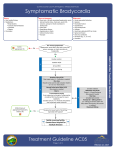
Bradycardia and Pacing Sinus brady • Fit • Cold • Drugs- β-blockers, CCBs, digoxin • • Sick-sinus syndrome Hypothyroidism Heart blocks st • 1 degree – Prolonged PR interval >0.2s nd • 2 degree – Mobitz I (Wenkebach) • Progressive PR prolongation until a beat is dropped – Mobitz II • PR interval is constant, dropped beat randomly rd • • 3 degree (complete) – Complete dissociation between P waves and QRS complexes Pacing – Mobitz II – Complete Treatment Is the patient compromised? o Chest pain o Altered LOC o Hypotension o CCF Atropine 0.5mg-1.5mg IV q 15 minutes Pacing If pacing not available consider o Isoprenaline 10-20mcg IV followed by infusion (may exacerbate hypotension) o Adrenaline 10-20mcg IV Associated with MI o In inferior MI is usually transient o In anterior MI is usually permanent and a poor prognostic indicator- need pacing Life-Threatening Drug Toxicities β-blockers Overdose Highest risk with propranolol (widens QRS and seizures) and sotalol (prolongs QT) PR prolongation may be the earliest sign May have associated hypoglycaemia Atropine is only temporising Rx= high dose insulin euglycaemic therapy (1u/kg IV insulin followed by 1-2u/kg/hr infusion with 10% dextrose) QRS widening rx= sodium bicarbonate QT prolongation rx= magnesium, isoprenaline, overdrive pacing www.emergencypedia.com Westmead JMO After-hours STAR Program Glucagon is no longer commonly used Calcium channel blocker Overdose Highest risk with verapamil and diltiazem May be associated with hyperglycaemia Decontamination is a priority o Charcoal if within 1 hour of ingestion for standard preparations, or 4 hours for extended release preparations o Whole bowel irrigation after charcoal in extended release preparations Rx o Calcium chloride 10% 20ml or calcium gluconate 10% 60ml o Atropine is temporising o High dose insulin euglycaemic therapy Digoxin Toxicity Differentiate acute (supratherapeutic ingestion) v chronic (normal doses in patients with dehydration/ renal or hepatic impairment) Levels are more useful in chronic than acute toxicity (although a level over 15 predicts lethality in acute ingestions) Predictors of lethality in acute ingestion o o o o o ingested dose (more than 10 mg in adults, more than 4 mg in children) cardiac arrest potassium concentration above 5.0 mmol/L life-threatening ventricular arrhythmias decompensation (hypotension) from bradyarrhythmias Atropine is temporising, pacing is rarely effective, and tachyarrhythmias often resistant to cardioversion Rx= Digibind (Fab freagments) – suggested resource – “Tox Handbook” (Elesevier). Tox Reg (Page 8333) o Acute HD stable = 5 vials o Acute HD unstable = 10 vials o Acute cardiac arrest = 20 vials o Chronic = 2 vials Haemodialysis Treat hyperkalaemia aggressively with insulin-dextrose and sodium bicarbonate. There is a theoretical risk of “stone heart syndrome” with calcium administration but this is not based on more than case reports. Transcutaneous Pacing Indications o bradycardia unresponsive to drug therapy o 3rd degree heart block o Mobitz type II second-degree heart block when haemodynamically unstable or operation planned o overdrive pacing for Torsades (due to prolonged QT) o not likely to be effective in asystole (can trial if clear reversible cause) Set intial milliamps (mA) and desired rate to 70 Start pacing and increase the mA looking for electrical capture and then feeling for mechanical capture Once captured set mA 5-10 above the capture threshold www.emergencypedia.com Westmead JMO After-hours STAR Program