* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biomedical Instrumentation
Voltage optimisation wikipedia , lookup
Switched-mode power supply wikipedia , lookup
Alternating current wikipedia , lookup
Resistive opto-isolator wikipedia , lookup
Wireless power transfer wikipedia , lookup
Immunity-aware programming wikipedia , lookup
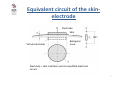
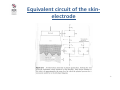
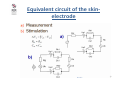
Ground (electricity) wikipedia , lookup
Stray voltage wikipedia , lookup
Mains electricity wikipedia , lookup
Resonant inductive coupling wikipedia , lookup
Rectiverter wikipedia , lookup
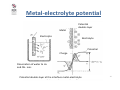
University of Zagreb Faculty of Electrical Engineering and Computing Biomedical Instrumentation - Transducers and sensors - Biopotential amplifiers - Electromagnetic interference prof.dr.sc. Ratko Magjarević June 2012 Electrodes • Bioelectrical potentials - recall: bioelectrical potentials occur at the cell membrane due to difference in ions concentration (mostly Na +, K + and Cl-) in intracellular fluid and in the extracellullar space • Potential difference at the cellular membrane may be in the range within 5mV and 100mV • This potential difference is called the resting potential 2 Electrodes • Bioelectrical resting potentials: – resting potential inside the cell is negative comparing to the environment – resting potential of nerve and muscle cells is typically -70mV to -85mV 3 Electrodes • Action potentials: when the cell membrane is stimulated, there is a sudden change in membrane conductance, first for sodium ions (cell depolarization), and then to potassium ions (repolarization) • Negative potential inside the cell reduces, such that short-term potential may become positive • Such a potential difference is called the action potential 4 Electrodes • How to access the cell and measure bioelectrical potentials? – a) individual cells • thickness of the semi-permeable membrane approx. 10nm • measurement of in vivo or in vitro – b) groups of cells - tissue or organ • access to tissue or organ - a non-invasive (bloodless) or invasive measurements • mutual influence of different tissues /organs (potentials, impedance) 5 Electrodes Electrode is an interface • to connect the measurement devices and measure bioelectrical potentials, electrode is used as an interface, however.. The electrode is also a transducer • exchange charge carriers : – in electrical circuits, electrons are charge carriers – in the body, ions are charge carriers • connects to the surface of the body (skin, mucous membranes) or on/in the organ inside the body 6 Electrodes • Most of bioelectric potentials strive to measure noninvasively, e.g. from the surface of the body, by placing electrodes on the skin • Electrical characteristics of different tissues – specific conductivity (specific resistance) – specific dielectric constant • Characteristics of biological tissue are: – nonlinearity (dependence on frequency and current density), – inhomogenity (unequal material properties of the body) – anisotropy (different properties in different dirrections, typically along the fiber-cells) 7 Electrodes • Using a model of the interface for better understanding of the interface electrode -tissue • Passive electrical characteristics of the skin - electrode interface strive to express by ideal electric components with intent parameters – Resistance – Capacity • This model can be used for measurement electrodes in limited frequency range 8 Equivalent circuit of the skinelectrode Electrode Skin Virtual electrode Biological issue Electrode – skin intarface and its simplified electrical circuit 9 RP Equivalent circuit of the skinelectrode d = ρ A µ - charge mobility ρ = CP 1 µ qn A = ε d q - charge n - number of electrons in volume unit Rp - resistance between the electrode and the well-conductive layer of tissue (virtual electrode) d – skin thickness A - electrode surface ρ - specific resistance Cp - capacity between the electrode and virtual electrode ε - dielectric constant of the skin 10 Equivalent circuit of the skinelectrode 11 Equivalent circuit of the skinelectrode 12 Nonlinearity of the electrode interface 13 Metal-electrolyte potential Potential double-layer Metal Electrolyte Electrolyte Potential Charge Dissociation of water to H+ and OH- ions Potential double-layer at the interface metal-electrolyte 14 Metal-electrolyte potential Standard electrode potential relative to standard hydrogen electrode at 20°C 15 Metal-electrolyte potential • If you plunge a metal in a solution of its salt, the half cell potential E0 M appears, also the voltage dependent on the concentration of metal ions in solution: RT E0.5 M = E0 M 1 − ln cM 1 nF • If there is some other metal also immersed in a solution of its own ions, its potential will be E 0 .5 M RT ln cM 2 = E0 M 2 − nF 16 Polarization voltage • If these two solutions are separated with semi-permeable membrane to allow passage of ions, and to avoid the original combination of solutions, the potential difference between the solutions can be measured according to the formula E = E0.5 M 1 − E0 M 2 RT [cM 1 ] = E0 M 1 − E 0 M 2 − ln nF [cM 2 ] • Each electrode that comes in contact with the electrolyte will have the potential of the expression above. This potential is undesirable in the measurement of biological voltage because when using high gain dc amplifier, it causes saturation of the amplifier. To avoid saturation, amplifier with less gain in the input is used and the next stages of amplification are separated with condenser. 17 Dry electrodes • Used to avoid the appearance of polarization voltage. • The problem is in large input impedance, which makes them susceptible to interference. • Therefore, the electrode itself incorporates an amplifier designed to reduce the high input resistance to a small value and thus reduce the impact of interference. 18 Dry electrodes with integrated amplifier Microelectrodes • They are used to measure the biological potential of the cells 19 Microelectrodes • cell attached recording: – pipette touching the membrane and forming a high-ohmic junction (~ 1GOhm) • whole cell recording: – by suction through a pipette the membrane breaks - solution in the pipette and inside of the cells become uniform 20 Microelectrodes Extracellular recording 21 Microelectrodes Action potentials recorded extracellularly 22 Subcutaneous electrodes • They are used, for example, to measure the voltage on the individual muscle fibers or groups of neurons in the brain Subcutaneous needle electrodes a) monopolar, b) bipolar c) wire d) electrode array d) cortical 23 Subcutaneous electrodes • Example of subcutaneous electrodes used for deep brain stimulation • Example of electrode implantation for deep brain stimulation 24 Subcutaneous electrodes 25 Surface EEG electrodes • EEG electrodes (passive, active) • Conductive paste and gel 26 Surface EEG electrodes • 10-20 system - standards for placing EEG electrodes 27 EEG recording 28 Surface ECG electrodes • Adhesive: • Suction (pump to suck air) 29 Surface ECG electrodes • Electrodes for extremities (hands and feet): • EKG recodring 30 EMG electrodes • Surface • Subcutaneous 31 EMG recording 32 Surface electrodes - more examples • EOG electrodes: • Electrodes for electrostimulation 33 Electrocardiograph • The apparatus that records the ECG is called the electrocardiograph • If a patient needs continuous monitoring during hospitalization, the ECG in “monitored” on a ECG monitor together with other physiological parameters 34 ECG Amplifier • The most important part of any equipment recording bioelectric potentials is the input amplifier • Most important characteristics: – Differential measurement (differentia or instrumetation amplifier) – High gain (input signal 50uV to 1 mV) – High common mode rejection ratio (CMRR) – Frequency range typically from 0,05 Hz to >=100 Hz – Very high input impedance – Low noise 35 ECG Input Signal • Composite signal – useful signal – ECG: amplitude span from 50 uV to 1 mV – polarisation voltage (electrochemical contact potential @ electrodes) – DC component, up to 300 mV – interference – mains (50 Hz or 60 Hz), up to 100 mV – interference voltages – defibrilator shock (n x 1000 V) or RF surgery equipment voltages 36 ECG Output • multichannel output – 15 seconds time frame, channels synchroneous • Print out – sensitivity: 2,5 mm/mV; 5 mm/mV; 10 mm/mV; 20 mm/mV – pape speed: 10mm/s, 25 mm/s, 50mm/s, 100 mm/s • Data storage – different formats – MIT BIH signal database (scientific) – interoperability 37 ECG Equipment classification • ECG recorders – classification to the number of channels • • • • • 1 channel ECG 3 channel ECG 6 channel ECG 12 channel ECG > 12 channel ECG 38 Symplified ECG Block Diagram Protection circuit Lead Selector Preamplifier Calibration Circuit (1mV step) Isolation Circuit Processing (analog or digital) Electrodes Driver Amplifier + Recorder - Printer 39 Amplifier Circuits - DC coupled 40 40 Common Mode Rejection Ratio (CMRR) • • • • The ratio of the differential gain over the common-mode gain Expressed in decibels Typically 100 – 120 dB for integrated instrumentation amplifiers Function of frequency and source-impedance unbalance. 41 Measurement of CMRR AD H= AZ uizlD AD = uulD ∆ ∆uizlZ AZ = uulZ 42 Amplifier Circuits - AC coupled 43 43 44 44 45 45 Auto-zero amplifiers • Automatic nihilation of amplifier offset voltage ∆u = u + − u − u− = A2 ⋅ uizl = A2 ⋅ A1 ⋅ ∆u uizl = A1 ⋅ ∆u ∆u = u+ − A2 A1 ⋅ ∆u u+ = ∆u (1 + A1 A2 ) ∆u = ∆u = A1 ⋅ uoff A1uoff u+ = = 1 + A1 A2 1 + A1 A2 A1 A2 uoff A2 46 Isolation amplifiers • Galvanic isolation of sensory and the measurement part of the measurement system (attached to the patient) and the processing and display part, usually powered by mains • Floating principle of measurement of biopotentials • The aim is also to protect the patient from the potentially dangerous voltages or currents comming from the un-isolated (mains powered part) of the system Biopotential Isolation Amplifier 48 48 Principle of floating measurements Ad lim H = =∞ ∆u 2 i u1i za Z n → ∞ Isolation amplifiers • Design of isolation amps: – Optical coupling • • • • • Isolation voltage typ. 4 – 7 kV fast cheap Nonlinear – digitazing of signals before the isolation gap Noice high – Electromagnetic coupling • Isolation voltage up to 10 kV • Resolution typ. 12 bit, max. 16 bit • fg low, max 1 kHz – Capacitive coupling • Characteristics worse than other types, but cheapest Otically coupled isolation amp 51 Linearisation u2 = f −1 u1 R1 u3 = f ' ( u2 ) R3 i2 = f ( u1 ) i2 ' = f ' ( u3 ) −1 u1 u3 = f ' f R3 R1 −1 u1 u1 u3 = f ' f = R3 R1 R1 u3 R3 f ( u1 ) = f ' ( u3 ) = u1 R1 u1 = u3 Linearisation EM coupled amps - AD 215 Capacitavly coupled isolation amps ISO 124 The input signal is frequency modulated fosc 500 kHz; Vizo = 2,4 kVef Capacitively coupled isolation amps 56 Digital isolation amp principles Preamplifier - Instrumentation Amplifier 58 ECG Shematic Diagram Texas Instrument's ADS1298 family of fully integrated analog front ends (AFEs) created to make much more portable ECG equipment possible 59 ECG Shematic Diagram Single channel ECG Source: A. Šantić, Biomedicinska elektronika, Školska knjiga, Zagreb 60 Signal and Noise Problems http://medstat.med.utah.edu/kw/ecg/image_index/index.html 61 ECG Interference Sources • Noise originating from sources external to the patient – – – – in most cases power-line interference (50 or 60 Hz) also Electrosurgical Unit (ESU) interference - high-frequency signals during operation Electrostatic Sources Electromagnetic Induction • Artifacts originating from the patient • Artifacts originating from patient-electrode contact 62 Artifacts in ECG • Artifacts originating from the patient – Movement Artifacts due to patient movement – Baseline Wander - ECG waveform baseline drifting up and down slowly, usually because of the patient breathing – EMG Interference – muscle contractions during recording the ECG. 63 Artifacts in ECG • Artifacts originating from patient-electrode contact – electrodes not tightly coupled to the patient so there is a change in electrode to skin impedance during the recording 64 Electromagnetic compatibility (EMC) • the degree to which an electronic system is able to function compatibly with other electronic systems • not susceptible to interference • not produce interference • Opposite: Electromagnetic interference (EMI) 65 Electromagnetic interference (EMI) • disturbance that affects an electrical circuit due to – electromagnetic radiation – electromagnetic conduction (bellow ~50 MHz) – electrostatic discharge • emitted from a source – external – internal • may interrupt, degrade or obstruct the performance of an electronic circuit 66 Electromagnetic interference (EMI) • Inductive coupling – Inductive coupling occurs where the source and receiver are separated by a short distance (typically less than a wavelength). Strictly, "Inductive coupling" can be of two kinds, electrical induction and magnetic induction. It is common to refer to electrical induction as capacitive coupling, and to magnetic induction as inductive coupling. • Capacitive coupling – Capacitive coupling occurs when a varying electrical field exists between two adjacent conductors typically less than a wavelength apart, inducing a change in voltage across the gap. 67 Electromagnetic interference (EMI) Conductive coupling – Conductive coupling occurs when the coupling path between the source and the receptor is formed by direct contact with a conducting body, for example a transmission line, wire, cable, PCB trace or metal enclosure. • Conduction modes – Conducted noise is also characterised by the way it appears on different conductors: • Common-mode or common-impedance[1]) coupling: noise appears in phase (in the same direction) on two conductors . • Differential-mode coupling: noise appears out of phase (in opposite directions) on two conductors. 68 Electromagnetic interference (EMI) • Magnetic coupling – Inductive coupling or magnetic coupling (MC) occurs when a varying magnetic field exists between two parallel conductors typically less than a wavelength apart, inducing a change in voltage along the receiving conductor. • Radiative coupling – Radiative coupling or electromagnetic coupling occurs when source and victim are separated by a large distance, typically more than a wavelength. Source and victim act as radio antennas: the source emits or radiates an electromagnetic wave which propagates across the open space in between and is picked up or received by the victim. 69 AC Mains interference • Capacitive paths 70 ECG Amplifier with input guarding 71 ECG Amplifier with Right Leg Drive • An operational amplifier which derives common mode voltage, inverts it and returns to the patient through the right leg. The patient is not grounded. 72 ECG input protection 73 Amplifier input protection Protection of the amplifier input against high-voltage transients. a) The connection diagram for voltage limiting elements with two optional resistors R for current limitation b) Typical current-voltage characteristic of voltage-limiting elements, Vb – breakdown voltage c) anti-parallel connection of diodes d) anti-parallel connection of Zener diodes e) gas-discharge tubes 74 Protection against overvoltage 12 600 600 600 10 500 500 500 8 400 400 400 6 300 300 300 V V V kV 1 kV/µs 4 200 200 200 2 100 100 100 0 0 20 40 µs UB = 24 V 60 0 0 1 2 0 µs 0 1 0 2 µs L = 10 µH tinjalica 0 1 2 µs L = 10 µH VDR otpornik Valni puls obliciat pojedinih točaka višestepene zaštite od prenapona Typical overvoltage mains connector and protection with gas discharge tubes, VDR (voltage dependent resistor) and a surge diode zaštitna dioda Protection of input against RF noise x 10-15mH 100n x 100n 0.5-1M8 y 3n3 RSO - filtar y 3n3 Protection of common mode and differential noise at the mains connector of the device EMI to Medical Devices Documented cases: • a ventilator suddenly changes its breath rate • an electric powered wheelchair suddenly veers off course • an apnea monitor fails to alarm...... Casamento JP, Ruggera PS.Applying standardized electromagnetic compatibility testing methods for evaluating radiofrequency interference with ventilators, Biomed Instrum Technol. Witters D.M. and P. S. Ruggera, EMC of Powered Wheelchairs and Scooters, Proc. RESNA '94 77 Solving EMI at System Level • EMI involves: – the device itself – the environment in which it is used – anything that may come into that environment • EMI - a systems problem requiring a systems approach • EMI solution requires involvement of – the (medical) device industry, – the EM source industry (power industry, telecommunications industry....), – the clinical user and patient 78 IEC Classification • • • International Electrotechnical Commission (IEC) classification of EM environment Conditions for the location and power of local EM energy sources (e.g., transmitters) Table 1 indicates the general classifications and the upper range of radiated EM field strength specified for each environment. 79 Sources of EMI • Radio broadcasting • Television • Public safety (police, fire, highway, forestry, and emergency services) • Land transportation (taxis, trucks, buses, railroads) • Amateur radio • Cellular phones and paging systems • Industrial, scientific, and medical • Citizens' band (CB) radio • Radar ..... 80 Model of Interference from: S. Hrabar, Analysis of EMI between mobile telephone and impllanted medical device, Ph.D. thesis, 1999 81 81 Literature • John G. Webster: Medical Instrumentation, Chapter 5, Biopotential Electrodes; Chapter 6, Biopotential Amplifiers 82