* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Coeliac Plexus Block mgmc
Survey
Document related concepts
Transcript
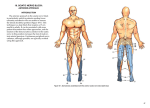
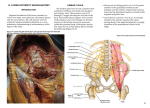
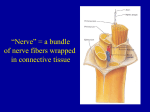
Coeliac Plexus Block Dr. S. Parthasarathy MD., DA., DNB, MD (Acu), Dip. Diab. DCA, Dip. Software statistics Ph D physiology. Mahatma gandhi medical college and research institute, puducherry, India Definition- what is this coeliac plexus ?? • A complex network of nerve fibres • The coeliac plexus is the largest of the autonomic plexuses and is located in the abdomen surrounding the coeliac and superior mesenteric arteries Introduction • The coeliac plexus contains visceral afferent and efferent fibers derived from T5 to T12 by means of the greater, lesser, and least splanchnic nerves. • The plexus has no somatic fibers and is composed of a number of ganglia and nerve fibers. • It innervates most of the abdominal viscera. Coeliac plexus HISTORY 1914 – KAPPIS – first block in lateral position 1920 – WELDING – anterior approach. 1927 – LABAT – now followed retrocrural approach in prone position. 1982 – SINGLERS – CT guided transcrural approach 1983– ISCHIA – posterior transaortic approach Indications: • Abdominal pain associated with malignancy. • ( Local anaesth. Or neurolysis) • Nonmalignant abdominal pain ( neurolysis controversial). Is it worth ?? • In carefully selected patients with pancreatic cancer, • provide partial to complete pain relief for 90% patients for up to 3 months and 7090% up until end of life. • Pain relief for all types of upper GI cancer has been reported to be between 70 and 97%. Indications • can be combined with an intercostal block to provide anaesthesia for intraabdominal surgery. • Because it results in blockade of the autonomic nervous system, may help reduce stress and endocrine responses to surgery. Anatomy • The coeliac plexus -- solar plexus. • main junction for autonomic nerves supplying the upper abdominal organs (liver, gall bladder, spleen, stomach, pancreas, kidneys, small bowel, and 2/3 of the large bowel). • The celiac plexus proper consists of the celiac ganglia with a network of interconnecting fibers. . Anatomy • Sympathetic-supply: Greater splanchnic nerve (T5/6 to T9/10) Lesser splanchnic nerve (T10/11) Least splanchnic nerve (T11/12) The upper abdominal organs receive their parasympathetic supply from the left and right vagal trunks, which pass through the coeliac plexus but do not connect there Anatomy • L1 vertebra. – posterior • The vena cava lies anteriorly to the right, and on the left anteriorly is the aorta., with the pancreas anterior. • The kidneys lie laterally • The number of ganglia varies from one to five, and each ganglion is 0.5 to 4.5 cm in diameter. Left-sided ganglia are usually lower than those on the right. Coeliac plexus Technique • prone position and a pillow beneath the abdomen • intravenous sedation, local anaesthetic infiltration of the superficial layers • Iv fluids • Needle entry – below tip of twelfth rib Technique Technique • L1 spinous process(A) • inferior edge of the 12th rib at a point 78cm lateral of the midline(points B and C). Connect these points to form a triangle, the base of which is passing over the inferior edge of the L1 spinous process Technique • Aseptic preparation of the skin, • infiltrate the skin and muscle with local • use a 12-18 cm long ,20-22 gauge needle and introduce(the left side needle first) at a 45degree angle relative to the sagittal plane • The direction is towards the L1 spine and proceeds to hit on the L1 vertebral body. • (more superficial bony contact may be the L1 transverse process) Finger as control Technique • The needle contacts the L1 vertebral body at a depth of. 7-10 cm. • A skin marker is placed on the needle. • The needle is then withdrawn • re introduced laterally until it just slips from the lateral border of the vertebral body Slowly advance the needle further, feeling for the transmitted pulsations of the aorta and stop advancing once pulsations are felt. • On the right side advance further 1 cm. Points A,B,C and 2 needles Fluroscopy CT guided Other techniques Paramedian approach: Needle is inserted caudad to 12 th spinous process at a point 3 cm lateral to the midline in a plane perpendicular to the skin Anterior approach: Through the anterior abdominal wall under fluoroscopic and ultrasound guidance. USG guided anterior approach Newer approaches • “transdiscal percutaneous approach of splanchnic nerves”, • which is carried out under • CT control, improves accuracy, reduces complications Surgical approach Transgastric approach Endoscopic Ultrasound Drugs • Agents used for blockade are 0.5% bupivacaine with adrenaline1:200000 around 30ml, 15 ml on either side with or without dexa for chronic pain • Neurolytic blockade is indicated in abdominal malignancies where alcohol 50-100% or 10% phenol is used. • The pain on injection of alcohol can be minimised with combination of bupivacaine 1:1 ratio How to know it works ?? • The signs of successful block is • hypotension • patient may feel an urge to empty bowel. Contraindications • Bleeding disorders and infection • Aortic aneurysm • Non autonomic pain Complications • Severe hypotension may result, even after unilateral block. • Bleeding due to aorta or inferior vena cava injury by the needle. • Intravascular injection (should be prevented by checking the needle position with radio-opaque dye). • Upper abdominal organ puncture with abscess/cyst formation. Complications • Paraplegia from injecting phenol into the arteries that supply the spinal cord (prevented by checking the needle position with radio-opaque dye). • Sexual dysfunction (injected solution spreads to the sympathetic chain bilaterally). Intramuscular injection into the psoas muscle. • Lumbar nerve root irritation (injected solution tracks backwards towards the lumbar plexus). Complications • More from neuro lytic blocks Thank you all