* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Recent Developments
Survey
Document related concepts
Transcript
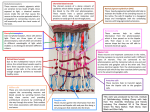
RECENT DEVELOPMENTS IN RETINAL DEGENERATION. A/Prof Erica Fletcher, The University of Melbourne It has been clear for a long time that RP is a difficult disease, both to understand and to treat. Over the last five years, however, there have been considerable advances in our knowledge of the pathogenesis of inherited retinal degenerations and this has lead to the development of some very promising treatments. Below, we have summarized some of the recent research that has lead to the testing of novel treatments in clinical trials or that are showing great promise in animal models of inherited retinal degenerations. Broadly, research into treatments for those with inherited retinal degeneration can be broken down into ways to slow photoreceptor death ways of replacing the function of lost photoreceptors, or gene therapies that correct the causative genetic mutation. i) Slowing photoreceptor death: A number of approaches have been investigated over recent years to slow photoreceptor death. It is now known that growth factors are required to maintain photoreceptors. Promising clinical trials are underway to examine whether treating those with the dry form of Age Related Macular Degeneration and also RP with a growth factor called CNTF slows the loss of cones. In the past, promising protective effects have been shown when rodent models of inherited retinal degeneration and dogs with achromatopsia were treated with CNTF. One of the more interesting effects noted in animals treated with CNTF was that regeneration of the cone structure. This observation means that treatment can be initiated even when cone function may be lost. It is hoped these preclinical results can now be translated into the clinical setting for those with advanced Age Related Macular Degeneration. ii) Novel ways of replacing lost photoreceptors: The two most exciting developments to restore vision in those who have few photoreceptors remaining are the development of electronic implants, and the use of gene therapy to target visual pigments to the remaining neurons of the inner retina. There are currently over 30 groups world wide including two large groups in Australia developing electronic implants to restore vision. One group in the USA, called Second Sight has approval to market a device that is inserted onto the surface of the retina to restore vision in those with severe vision loss. This device (called Argus II) has been extensively tested in clinical trials with patients reporting the ability to read large letters and recognize objects. In Australia, Bionic Vision Australia has developed a wide-field device that sits underneath the retina, and another high visual acuity device that is designed to target the output neurons of the retina. Three people have received the wide field device with promising results reported. The high visual acuity device is currently undergoing preclinical testing. A second group, based at Monash University is designing an implant to be inserted into the visual area of the brain. This device, is intended to restore vision in those who have no remaining ganglion cells or an intact optic nerve. Currently this device is undergoing extensive preclinical development. Although gene therapy is normally associated with correcting a mutant gene, it can also be used to incorporate a visual pigment into neurons that remain in the retina. The inner retina of those with inherited retinal degeneration is usually intact. By using gene therapy, inner retinal neurons can become light sensitive, performing the duties of photoreceptors. These studies are very exciting because the technology can be used in most patients with inherited retinal degeneration irrespective of the specific genetic cause of a person’s disease. Stem cells have been recently used to replace lost photoreceptors and also damaged RPE cells. Two different approaches have been trialled in animal models of inherited retinal degeneration. First, precursor cells (a more mature stage than embryonic stem cells) have been transplanted into the region of the retina, where photoreceptors would normally reside, and shown that they change into photoreceptors and form new connections with downstream neurons. In addition, these experiments show that this method restores some vision in blind animals. These are very exciting results, however, there is quite a lot of scientific work still needed to demonstrate that this approach is safe for patient use. A different type of stem cell is currently being trialled in patients with advanced Age Related Macular Degneration and Stargardts disease. In a clinical trial being conducted in the UK, RPE cells that have been derived from human embryonic stem cells are injected under the retina and to replace the lost RPE cells. The first results in three patients were reported in early 2012, and show that the approach is feasible, safe and can lead to a modest gain in vision. Lastly, scientists know a great deal now about how cells change in the retina during the late stages of retinal degeneration. Glial cells, a type of support cell in the retina, change gradually during retinal degeneration. In particular, a very small number of glial cells start proliferating during late stages of retinal degeneration, and can differentiate into photoreceptors. Scientists are currently trying to understand what signals are required to make glial cells proliferate and change. It is hoped that if the signalling mechanisms are known, then more glial cells can be encouraged to change into photoreceptors. (iii) Gene therapy: Gene therapy involves injecting a virus like molecule called a vector underneath the retina, so that the genetic material carried by the vector can incorporate into the cell of interest and correct the disease causing genetic mutation. A clinical trial in patients with Leber Congenital Amaurosis that is caused by a mutation in RPE65 was first reported in 2008 and is ongoing. Recent results of the first cohort of patients (treated in 2008) show that the gains in vision these patients had after only 6 months are stable and maintained for 3 years. These results, are extremely exciting because they not only show restoration in vision in those who have inherited this mutation, but also demonstrate that gene therapy is technically possible and safe in people. Along side these results, there have been a number of studies carried out in animal models showing that gene therapy can be used to restore vision caused by a range of other mutations. With the combination of laboratory work, studies in animal models and now the results of clinical trials, it is hoped gene therapy may be soon a reality for patients who have inherited some of the more common gene mutations. In summary, over the last few years our knowledge of inherited retinal degeneration has increased dramatically, to the point where treatments are now being tested in patients, with exciting results.