* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Pericarditis, Endocarditis, Myocarditis
Pericardial heart valves wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Mitral insufficiency wikipedia , lookup
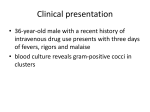
Pericarditis, Endocarditis, Myocarditis Victor Politi, M.D., FACP Medical Director, SVCMC, School of Allied Health Professions, Physician Assistant Program The Pericardium • Two layers - composed of fibrous tissue – inner visceral layer, attached to epicardium – outer parietal layer • stabilizes heart in anatomic position • protects heart - (contact with surrounding structures) The Pericardium • Can be – a primary site of disease – involved in other disease processes that affect the heart – affected by other diseases of adjacent tissue The pericardium can permit moderate changes in cardiac size, however, it cannot stretch rapidly enough to accommodate rapid dilation of the heart or accumulation of fluid w/o increasing intrapericardial/intracardiac pressure Acute Pericarditis • Acute inflammation of the pericardium • Origin – infectious,systemic diseases,malignancy, radiation,drug toxicity,hemopericardium,other inflammatory processes in the myocardium or lung • Pathologic process often involves both the pericardium and the myocardium Acute Pericarditis • Presentation & course may vary depending on the cause • syndromes often associated with – chest pain (pleuritic/postural) – dyspnea – pericardial friction rub (with or w/o evidence of fluid accumulation or constriction) – Fever & leukocytosis Acute Pericarditis • Chest x-ray – may show cardiac enlargement or pleural dx • ECG – generalized ST and T wave changes – characteristic progression (ST elevation, return to baseline, T wave inversion) • Echocardiogram – often normal in inflammatory pericarditis – may show pericardial effusions Acute Pericarditis- Causes • viral infection – most common coxsackievirus, & echovirus • also- HIV,influenza,Epstein-Bar, varicella, hepatitis, mumps • bacterial infection – staphylococcus, Strep pneumoniae, Bhemolytic streptococci, Mycobacterium tuberculosis, lyme dz • Fungal infection • Malignancy Acute Pericarditis - Causes • Drugs – procainamide,hydralazine,minoxidil • • • • • • radiation connective tissue disease(lupus,rheum) uremia myxedema post-MI (Dressler’s syndrome) Idiopathic Acute Pericarditis Clinical Features • Sudden or gradual onset of sharp or stabbing chest pain that radiates to the back, neck, left shoulder, arm, or trapezial ridge • Pain aggravated by movement or inspiration and by lying supine • sitting up and leaning forward reduces the pain Acute Pericarditis Clinical Features • Associated symptoms include; – low grade intermittent fever, dyspnea, dysphagia • transient, intermittent friction rub heard best at the lower left sternal border or apex is the most common physical finding Acute Pericarditis Clinical Features • Pericardial effusion – As the pericardium stretches, • effusions that develop slowly, even large ones, may not produce hemodynamic changes • However …. • those that appear rapidly (even small effusions) can cause tamponade Acute Pericarditis Clinical Features • Tamponade – elevated intrapericardial pressure (>15 mm Hg), that restricts venous return and ventricular filling - resulting in decreased stroke volume /pulse pressure and increased heart rate/venous pressure – most common complaints;dyspnea and decreased exercise tolerance – common symptoms; weight loss, pedal edema, ascites Acute Pericarditis Clinical Features • Tamponade – Physical Findings; tachycardia, low systolic BP, narrow pulse pressure, pulsus paradoxus, neck vein distention, distant heart sounds, RUQ pain Acute Pericarditis - Diagnosis • ST-segment elevation • Pericarditis w/o other underlying cardiac disease does not typically produce dysrhythmias • Chest x-ray usually normal - but should be done to rule out other disease • Echocardiography Acute Pericarditis - Diagnosis • Other Tests – CBC w/diff – BUN – Creatinine – streptococcal serology – appropriate vial serology – other serology (antinuclear and anti-DNA antibodies) – thyroid function studies – Sed rate, creatinine kinase levels w/isoenzymes Viral Pericarditis – Most commonly caused by coxsackievirus, & echovirus – Can also be caused by HIV, influenza, Epstein-Bar, varicella, hepatitis, mumps – Most commonly affects males < age 50 – Diagnosis usually clinical – rising viral titers in paired sera may be obtained for confirmation of diagnosis – cardiac enzymes may be slightly elevated indicating myocarditic component Viral Pericarditis- Treatment • • • • Generally symptomatic Tx aspirin or NSAIDs Corticosteroids -(unresponsive cases) Symptoms generally subside over several days to weeks • May be recurrences - during first few weeks - months • Rarely, patients suffer from chronic recurrences resulting in constrictive pericarditis • Major early complication - tamponade (< 5% of cases) Bacterial Pericarditis – staphylococcus, Strep, pneumoniae, Bhemolytic streptococci, Mycobacterium tuberculosis – Usually direct result from pulmonary infection – patients often present in a critically ill state – Borrelia burgdorferi (Lyme Disease organism) can also cause myopericarditis Tuberculous Pericarditis • Rare in developed countries - common elsewhere • Results from direct lymphatic or hematogenous spread • commonly have associated pleural effusions & small to moderate pericardial effusions • subacute presentation/non-specific symptoms (fever, night sweats, fatigue) • Diagnosis inferred if acid-fast bacilli found elsewhere • Usual therapy - standard antituberculous drug • Complication- if therapy unsuccessful- constrictive pericarditis Uremic Pericarditis • Complication of renal failure • Occurs in untreated uremia and in stable dialysis patients • Presents with or w/o symptoms, typically afebrile • tamponade is common • usually resolves with institution or more aggressive dialysis • pericardiectomy may become necessary • indomethacin & systemic glucocorticoids ineffective for uremic pericarditis Neoplastic pericarditis • Commonly caused by – breast and renal cell carcinoma, Hodgkin's Disease and lymphomas • neoplastic processes involving the pericardium are the most common cause of pericardial tamponade in many countries • presenting symptoms relate to the hemodynamic compromise of the primary disease process • MRI/CT Neoplastic pericarditis • Prognosis poor - only small minority survive >year • Effusion can be drained, chemotherapeutic agents or tetracycline may prevent recurrence • pericardial windows rarely effective, partial pericardiectomy from a subxiphoid incision may be successful Radiation Pericarditis • Usually occurs within the first year after exposure but can be delayed for many years • Symptomatic therapy - initial approach but recurrent effusions and constriction require surgery Post MI or Postcardiotomy Pericarditis • An inflammatory reaction to transmural myocardial necrosis that usually occurs 2-5 days after infarction • typically presents as pain recurrence • audible rub, repolarization changes • spontaneous resolution usually occurs after a few days • Aspirin, NSAID’s -symptomatic relief Dressler’s Syndrome • Occurs weeks to several months after MI or open heart surgery • Presentation – typical pain, fever, malaise, leukocytosis, elevated sed rate – large pericardial/pleural effusions common – Tamponade is rare if Dressler’s after MI, but more commonly seen in Dressler’s post-operatively Dressler’s Syndrome • NSAID’s • Corticosteroids • Recurrences common Constrictive Pericarditis Constriction occurs when fibrous thickening and loss of elasticity of the pericardium results in interference of diastolic filling usually following inflammation Cardiac trauma, open heart surgery, intrapericardial hemorrhage, fungal or bacterial pericarditis, and uremic pericarditis are the most common causes of constrictive pericarditis (in the past, tuberculosis was also included) Constrictive Pericarditis - symptoms • Symptoms develop gradually and mimic those of restrictive cardiomyopathy (CHF, exercise dyspnea, decreased exercise tolerance) • chest pain, orthopnea, and paroxysmal nocturnal dyspnea are uncommon Physical Exam • • • • • • Pedal edema hepatomegaly ascites JVD Kussmaul’s sign(^jvp w/insp) pericardial knock (early diastolic sound) heard at the apex • usually - no friction rub Diagnosis • ECG - may show low voltage QRS complexes and inverted T waves • Chest x-ray - 50% of cases show pericardial calcification • Doppler echocardiography • Cardiac CT, MRI • Consider other diseases - acute pericarditis, myocarditis, exacerbation of chronic ventricular dysfunction, or systemic process (eg sepsis) Treatment • General supportive care - initial treatment • Symptomatic patients - pericardiectomy • Gentle diuresis • Treatment with appropriate antibiotics if agent is Id’d Endocarditis • Infective endocarditis is defined as an infection of the endocardial surface of the heart, which may include one or more heart valves, the mural endocardium, or a septal defect • Endocarditis can be broken down into the following categories: Native valve (acute and subacute) endocarditis Prosthetic valve (early and late) endocarditis Endocarditis related to intravenous drug use Native valve endocarditis (acute and subacute) • Native valve acute endocarditis usually has an aggressive course. Virulent organisms, such as Staphylococcus aureus and group B streptococci, are typically the causative agents of this type of endocarditis. • Subacute endocarditis usually has a more indolent course than the acute form. Alpha-hemolytic streptococci or enterococci, usually in the setting of underlying structural valve disease, typically are the causative agents of this type of endocarditis. Prosthetic valve endocarditis (early and late) • Early prosthetic valve endocarditis occurs within 60 days of valve implantation. Staphylococci, gramnegative bacilli, and Candida species are the common infecting organisms. Prosthetic valve endocarditis (early and late) • Late prosthetic valve endocarditis occurs 60 days or more after valve implantation. Staphylococcus epidermidis, alpha-hemolytic streptococci, and enterococci are the common causative organisms. Endocarditis related to intravenous drug use • Endocarditis in intravenous drug abusers commonly involves the tricuspid valve. S aureus is the most common causative organism • Infective endocarditis generally occurs as a consequence of nonbacterial thrombotic endocarditis, which results from turbulence or trauma to the endothelial surface of the heart. Endocarditis • Increased mortality rates are associated with increased age, infection involving the aortic valve, development of congestive heart failure, central nervous system (CNS) complications, and underlying disease • Affects men more than women (2:1 ratio) • Affects all age groups - however, 50% of cases in adults over age 50 Endocarditis • Most common symptoms - fever (90% of cases) and chills • Anorexia, weight loss, malaise, headache, myalgias, night sweats, shortness of breath, cough, or joint pains are common complaints • Dyspnea, cough, and chest pain are common complaints of intravenous drug users who have infective endocarditis Endocarditis • Primary cardiac disease may present with signs of congestive heart failure due to valvular insufficiency • Heart murmurs are heard in approximately 85% of patients Endocarditis One or more classic signs of infective endocarditis are found in as many as 50% of patients. They include the following: Petechiae - Common but nonspecific finding Splinter hemorrhages - Dark red linear lesions in the nailbeds Osler nodes - Tender subcutaneous nodules usually found on the distal pads of the digits Janeway lesions - Nontender maculae on the palms and soles Roth spots - Retinal hemorrhages with small, clear centers; rare and observed in only 5% of patients. splinter hemorrhages and purpuric papules on the foot of a 10 year old boy with acute bacterial endocarditis Splinter hemorrhages(Panel A) are normally seen under the fingernails. They are usually linear and red for the first two to three days and brownish thereafter. Panel B shows conjunctival petechiae. Osler's nodes (Panel C)are tender, subcutaneous nodules, often in the pulp of the digits or the thenar eminence. Janeway's lesions (Panel D) are nontender, erythematous, hemorrhagic, or pustular lesions, often on the palms or soles Endocarditis • baseline studies, such as a complete blood count (CBC), electrolytes, creatinine, BUN, glucose, and coagulation panel • Blood cultures: Two sets of cultures have >90% sensitivity when bacteremia is present. Three sets of cultures improve sensitivity and may be useful when antibiotics have been administered previously Endocarditis Echocardiogram Transthoracic echocardiography has a sensitivity of approximately 60%. Transesophageal echocardiography has a sensitivity of more than 90% for valvular lesions Endocarditis • Empiric antibiotic therapy is chosen based on the most likely infecting organisms. Native valve disease usually is treated with penicillin G and gentamicin for synergistic treatment of streptococci Endocarditis • Patients with a history of IV drug use may be treated with nafcillin and gentamicin to cover for methicillinsensitive staphylococci. Endocarditis • Infection of a prosthetic valve may include methicillin-resistant Staphylococcus aureus; thus, vancomycin and gentamicin may be used, despite the risk of renal insufficiency Endocarditis • Rifampin also may be helpful in patients with prosthetic valves or other foreign bodies; however, it should be used in addition to vancomycin or gentamicin. Endocarditis prophylaxis against infective endocarditis in patients at higher risk. Patients at higher risk include those with the following conditions: Presence of prosthetic heart valve History of endocarditis History of rheumatic heart disease Congenital heart disease with a high-pressure gradient lesion Mitral valve prolapse with a heart murmur Endocarditis prophylaxis in patients before they undergo procedures that may cause transient bacteremia, such as the following: Ear, nose, and throat (ENT) procedures associated with bleeding, including dental manipulations and nasal packing Incision and drainage of an abscess Anoscopy and Foley catheter placement when a urinary tract infection is present or suspected Myocarditis Myocarditis • Inflammation of the myocardium • May be the result of systemic disorder or infectious agent ...usually follows an upper resp infection • Pericarditis frequently accompanies myocarditis • Drug induced, cytotoxic agents,also, cocaine Myocarditis • Bacterial cases include; – Corynebacterium diphtheriae, Neisseria meningitides, Mycoplasma pneumoniae, and B-hemolytic streptococci • Viral etiologies include; – coxsackie B, echovirus, influenza, parainfluenza, Epstein-Barr, and HIV Myocarditis -clinical features • Systemic signs/symptoms (fever, tachycardia, myalgias, headache, and rigors) • chest pain due to coexisting pericarditis • pericardial friction rub in cases of concomitant pericarditis • In severe cases - symptoms of progressive heart failure (CHF, pulmonary rales, pedal edema, etc.) Diagnosis • Nonspecific ECG changes, atrioventricular block, prolonged QRS duration, or ST segment elevation (in cases of accompanying pericarditis) • normal chest x-ray • cardiac enzymes may be elevated • Differential diagnosis includes cardiac ischemia or infarction, valvular disease and sepsis Treatment • Supportive care • If bacterial cause suspected, antibiotics are appropriate • Myocardial biopsy may reveal inflammatory pattern • Many cases spontaneously resolve others progress to dilated cardiomyopathy Questions ?