* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical Considerations During Phase 2 and Phase 3 of - M
Survey
Document related concepts
Polysubstance dependence wikipedia , lookup
Compounding wikipedia , lookup
Neuropharmacology wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug design wikipedia , lookup
Drug interaction wikipedia , lookup
Clinical trial wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Prescription costs wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Transcript
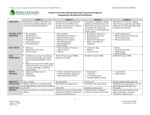
Clinical Pharmacology 2: Clinical Pharmacology Considerations During Phase 2 and Phase 3 of Drug Development Su-Young Choi, Pharm.D., Ph.D Division of Clinical Pharmacology IV Office of Clinical Pharmacology Office of Translational Sciences CDER, FDA The views expressed in this presentation are that of the author and do not reflect the official policy of the FDA. No official endorsement by the FDA is intended nor should be inferred. Objectives • Understand the role of clinical pharmacology throughout drug development • Understand the importance of analysis of exposureresponse (E-R) relationship • Describe the utility of E-R analysis throughout clinical development • Understand barriers to informative E-R evaluation and key steps to the overcome the barriers • Understand the impact of complete and incomplete clinical pharmacology programs on information available to health care providers 2 Phases of Drug Development • Phase 1 – Investigate the safety, tolerability, and pharmacokinetics of the drug – Allow selection of an appropriate dose range for Phase 2-3 • Phase 2 – Provide preliminary data on the safety and effectiveness of the drug – Allow selection of appropriate doses for evaluation in Phase 3 • Phase 3 – Provide pivotal information about effectiveness and safety – Allow evaluation of the overall benefit-risk relationship of the drug 3 Examples of Phase 1-3 Trials • Selected examples of dolutegravir Phase 1-3 trials • Phase 1 trial – Effects of low, moderate, or high fat meals on the pharmacokinetics of dolutegravir in 24 healthy volunteers – Effects of dolutegravir on the pharmacokinetics of ethinylestradiol in 16 healthy female volunteers • Phase 2 trial – 278 HIV patients were randomly assigned to one of the following groups • Dolutegravir 10 mg, 25 mg, 50 mg or standard of care (active control) • Based on the safety and efficacy data collected in this trial, 50 mg was selected for the Phase 3 study • Phase 3 trial – 844 HIV patients were randomly assigned to dolutegravir 50 mg or standard of care (active control) Ann Pharmacother. 2015 Jul;49(7):784-9. Lancet Infect Dis. 2012 Feb;12(2):111-8. N Engl J Med 2013; 369:1807-1818 4 Antimicrob Agents Chemother. 2012 Mar; 56(3): 1627–1629. Pharmacokinetic Assessments during Phase 2-3 Trials • While the primary goal of Phase 2-3 trials is to determine the safety and efficacy of a drug, blood (or target tissue) samples can be collected to determine the concentrations of the drug in Phase 2-3 trials – Typically in a sparse manner in Phase 2-3 trials – The sample collection schedule varies depending on PK characteristics, feasibility, and specific questions that you want to address. – Example • Dolutegravir Phase 3 trial • Dosing regimen: 50 mg once daily for > 48 weeks • Patients provided blood samples for pharmacokinetic analysis at the 4th, 24th, and 48th week of the treatment (at pre-dose or 1-3 hour post dose). 5 Br J Clin Pharmacol. 2015 Sep;80(3):502-14. Clinical Pharmacology Evaluation during Phase 2-3 Trials • Why do we collect drug concentration data during Phase 2-3 trials? – i.e. what valuable information can we obtain, especially information that cannot be obtained from healthy volunteers “To link exposure (drug concentration) to safety and efficacy data” Exposure-response relationship 6 Exposure-Response Relationship Efficacy Response Toxicity A Which is the optimal “target” concentration? A vs. B A vs. C B C Drug concentration Cmin, Cmax, AUC, Css, Log transformed concentrations, etc 7 Probability of AST/ALT elevation Diastolic blood pressure Examples of Exposure-Response Relationships Journal of Clinical Pharmacology, 2008;48:823-836, The AAPS Journal 2004; 6 (4) Article 28, http://regist2.virologyeducation.com/2013/8hepcam/docs/12_Caro.pdf, Clin Pharmacokinet. 2016 May 18. [Epub ahead of print] 8 The Value of E-R Information • Help design well-controlled studies (e.g., from Phase 2 to Phase 3) and select adequate doses for approval – Does treatment effect/adverse event increase with dose/exposures? – A dose may be selected for Phase 3 or approval even if it was not evaluated in previous trials. • Contribute to substantial evidence of effectiveness – Do data indicate a treatment effect? – It may support approval when there are not two adequate and well controlled studies. ICH E4 dose-response information to support drug registration 9 The Value of E-R Information • Allow a better understanding of the clinical trial data – What is the minimal effective concentration? – What is the therapeutic window? – Why do certain groups of people have lower efficacy or increased adverse events? • Is it due to exposure differences? – Adherence – Patient factors (race/ethnicity, sex, hepatic/renal impairment) – Concomitant medications 10 The Value of E-R Information • Support new target populations, use in subpopulations, new doses/dosing regimens, dosage forms and route of administration 11 Example 1 – Dose selection for Phase 3 Dolutegravir --Integrase strand transfer inhibitor (INSTI) indicated for the treatment of HIV-1 infection Treatment-naive INSTI-resistance Patients Treatment-naïve INSTI-resistance Issue No resistance Possible resistance to the study drug May require higher exposures Phase 2 10, 25, and 50 mg QD 50 mg QD or BID Phase 3 50 mg QD 50 mg BID http://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204790Orig1s000ClinPharmR.pdf 12 Example 2 –Different Doses in Women • Zolpidem: approved for the treatment of insomnia • Zolpidem blood levels above 50 ng/mL impairs driving to a degree that increases the risk of a motor vehicle accident • Women appear to be more susceptible to this risk – It is because they eliminate zolpidem from their bodies more slowly than men. • After administering 10 mg zolpidem, about 15% of women and 3% of men had zolpidem concentrations that exceeded 50 ng/mL approximately 8 hours post-dosing. – 15% women who take zolpidem at midnight may have impaired driving during their morning commute! http://www.fda.gov/Drugs/DrugSafety/ucm334033.htm 13 Example 2 –Different Doses in Women • Current dosing recommendations for zoplidem (immediate release) – The recommended initial dose is 5 mg for women and either 5 or 10 mg for men, taken only once per night immediately before bedtime with at least 7-8 hours remaining before the planned time of awakening. Higher exposure (concentration) in women more adverse events (response) in women lower doses used in women http://www.fda.gov/Drugs/DrugSafety/ucm334033.htm 14 Example 3- Interpretation of Drug Interaction Results • Grazoprevir is approved for the treatment of chronic hepatitis C infection • The drug is associated with ALT elevation • The concentrations of grazoprevir are increased when it is co-administered with various drugs as follows. Which ones can be used with grazoprevir and which ones should not be? Interacting drug Changes in grazoprevir AUC Ritonavir 2.0-fold Ketoconazole 3.0-fold Darunavir/ritonavir 7.5-fold Lopinavir/ritonavir 12.9-fold Cyclosporine 15.2-fold The use of these drugs with grazoprevir is contraindicated based on the exposureresponse relationship for safety (ALT elevation) of grazoprevir ZEPATIER™ USPI http://regist2.virology-education.com/2013/8hepcam/docs/12_Caro.pdf 15 http://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/208261Orig1s000ClinPharmR.pd Example 4 – To Support the Approval of New Formulations and New Dosing Regimens • A tablet formulation of drug X was evaluated in Phase 1-3 trials and approved. The current dosing regimen is 300 mg twice daily. • After the approval, the company decided to develop a solution formulation for patients who cannot swallow tablets. • After the approval, the company wanted to change the dosing regimen to 600 mg once daily to improve adherence. 16 The new formulation (solution) ↑ Cmax, ↓ Cmin, ↔ AUC (area under the curve) Concentration Question: Do you expect changes in efficacy/safety of drug X? (i.e. are PK differences clinically relevant?) Time 17 Concentration Time The exposure-response relationship analysis can answer! 18 Barriers to Informative Exposure-Response Evaluation • Data not collected or collected too late – “…the general belief that the company conducted its pharmacokinetic/pharmacodynamic study too late in the game, leading to less than adequate dosing being brought forward in Phase III and for approval” – Pinksheet (9/16/2014) summarizing advisory committee meeting for parathyroid hormone • Study design flaws • Study conduct flaws – lack of validated bioanalytical assay – lack of documentation (dosing times not captured, sampling times not captured) 19 Overcoming the Barrier Good Practice for Exposure-Response Evaluation – Identification of key questions • Details of some analyses can be defined beforehand. – Design and interpretation based on pharmacology and physiological principles • Example: tenofovir for the prevention of HIV transmission – Adherence to the therapy is the key for the efficacy (prevention) – Plasma concentration of tenofovir or emtricitabine: short half life – Active metabolites in immune cells: longer half life a better marker for the adherence Modified from CPT pharmacometrics Syst. Pharmacol (2015) 4, 565-575 20 Good Practice for Exposure-Response Evaluation – Good understanding of the assumptions and limitations – Appropriate choice of analysis methods and datasets • Various statistical models are available • Which clinical trial results should be/should not be used? – Appropriate handling of dropouts and covariates 21 Modified from CPT pharmacometrics Syst. Pharmacol (2015) 4, 565-575 Summary and Conclusion • Without exposure-response information – Dose selection may not be optimal – We cannot interpret the significance of exposure changes • Result: Lack of dosing instructions for certain groups – They are deprived of therapy – Or, they risk suboptimal safety and efficacy 22 RIGHT DRUG RIGHT PATIENT GOAL RIGHT DOSE RIGHT TIME 23