* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Effect of Baseline and Changes in Systolic Blood Pressure Over
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
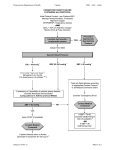
Effect of Baseline and Changes in Systolic Blood Pressure Over Time on the Effectiveness of Valsartan in the Valsartan Heart Failure Trial Inder S. Anand, MD, DPhil, FRCP; Thomas S. Rector, PhD; Michael Kuskowski, PhD; Sabu Thomas, MD; N. J. Holwerda, MD; Jay N. Cohn, MD Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Background—Low systolic blood pressure (SBP) is a risk factor for adverse outcomes in patients with heart failure (HF). Valsartan improved morbidity rates in the Valsartan Heart Failure Trial (Val-HeFT) despite a reduction in SBP. The aim of the present study was to investigate the relationship between the SBP-lowering effects of valsartan and its cardiovascular protective effects in this population. Methods and Results—Baseline measurements and changes in SBP at 4 months were related to mortality and morbidity rates. The effects of valsartan on these end points were compared in quartiles of baseline SBP with multivariable Cox proportional hazards regression models that included a test for interaction between the effects of valsartan treatment and baseline SBP and examined the effects of changes in SBP on the valsartan effect. The mean⫾SD baseline SBP in all patients (n⫽5010) was 124⫾18 mm Hg. Patients in the lowest quartile of SBP (SBP ⱕ110 mm Hg; mean SBP 102 mm Hg; n⫽940) had more severe HF and a significantly increased adjusted risk of death (hazard ratio [HR], 1.21; 95% confidence interval [CI], 1.03 to 1.43; P⫽0.02), first morbid event (HR, 1.25; 95% CI, 1.10 to 1.40; P⫽0.001), and hospitalization for HF (HR, 1.45; 95% CI, 1.22 to 1.73; P⬍0.001) than did patients in the upper 3 quartiles of baseline SBP (mean SBP 130 mm Hg; n⫽3260). Valsartan reduced SBP in patients in the upper 3 quartiles but not in patients in the lowest quartile who had a baseline SBP ⬍110 mm Hg. Valsartan was associated with decreases in the risks of first morbid event (HR, 0.74; 95% CI, 0.60 to 0.91; P⫽0.005) and hospitalization for HF (HR, 0.60; 95% CI, 0.45 to 0.79; P⬍0.001) in the lowest quartile that were not significantly different than the valsartan effects in the other 3 quartiles combined (first morbid event HR, 0.90; 95% CI, 0.79 to 1.02; P⫽0.10; and HF hospitalization HR, 0.77; 95% CI, 0.64 to 0.93; P⫽0.006; nonsignificant interactions). The decrease in SBP from baseline to 4 months was an independent risk factor for subsequent events. When changes in SBP were added to the regression model, the effects of valsartan in the lowest quartile and in the other 3 quartiles combined did not change substantially. Conclusion—Baseline SBP and a decrease in SBP over time were risk factors for adverse events in HF. Valsartan reduced SBP but not in the high-risk group of patients who had a baseline SBP ⬍110 mm Hg. The beneficial effects of valsartan did not vary significantly with baseline SBP, and decreases in SBP did not counteract the beneficial effects on HF morbidity rates. (Circ Heart Fail. 2008;1:34-42.) Key Words: heart failure 䡲 blood pressure 䡲 clinical trial 䡲 valsartan 䡲 outcomes H of hypertension, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and a combination of hydralazine and isosorbide, are also effective in reducing mortality and morbidity rates in patients with HF.12–17 Whether the beneficial effects of these medications on morbidity and mortality rates in patients with HF are modified by initially low or drops in blood pressure is an important clinical issue. igh blood pressure increases the risk of death in the general population,1,2 and hypertension is the most important population-attributable risk factor for the development of heart failure (HF).3,4 The benefits of treating hypertension on risks of major cardiovascular events are well established in the absence of systolic HF, and effective lowering of blood pressure is associated with an ⬇50% reduction in the incidence of HF.5,6 Once HF develops, however, lower blood pressure becomes a risk factor for increased mortality and morbidity rates both in acute decompensated7,8 and chronic HF.9 –11 The risk associated with elevated blood pressure in patients with systolic dysfunction has not been established. Vasodilators used in the treatment Clinical Perspective p 42 The present study is a secondary analysis of the Valsartan Heart Failure Trial (Val-HeFT) database to study the effects of baseline blood pressure and changes in blood pressure over Received August 31, 2007; accepted January 18, 2008. From the VA Medical Center, Minneapolis, Minn (I.S.A., T.S.R.); the University of Minnesota, Minneapolis, Minn (I.S.A., T.S.R., J.N.C., S.T.); Geriatric Research Education and Clinical Center, VA Medical Center, Minneapolis, Minn (M.K.); and St Elisabeth Hospital, Tilburg, the Netherlands (N.J.H.). The views expressed in this article are those of the authors and do not necessary represent the views of the Department of Veterans Affairs. Correspondence to Inder S. Anand, MD, FRCP, DPhil (Oxon), VA Medical Center, Cardiology 111-C, One Veterans Dr, Minneapolis, MN 55417. E-mail [email protected] © 2008 American Heart Association, Inc. Circ Heart Fail is available at http://circheartfailure.ahajournals.org DOI: 10.1161/CIRCHEARTFAILURE.107.736975 34 Anand et al Effect of Blood Pressure on Heart Failure Outcomes time on the effectiveness of treatment with valsartan on morbidity and mortality in patients with moderate to severe HF. First, we sought to confirm that both lower baseline systolic blood pressure (SBP) and a decrease in SBP over time were independently associated with an increased risk of morbidity and mortality. The interaction between the effects of valsartan and baseline SBP was then examined, controlling for several other known prognostic variables. Finally, to determine whether adjusting for any potentially deleterious drops in SBP during treatment would enhance the apparent beneficial effects of valsartan, we examined how controlling for changes in SBP affected the beneficial effects of valsartan. Methods Study Design and Patient Selection Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Val-HeFT was a randomized, placebo-controlled, double-blind, multicenter trial in 5010 men and women with symptomatic HF that evaluated the efficacy of the angiotensin receptor blocker valsartan. Details of the study design and protocol have been presented previously.17 Briefly, patients over 18 years of age who were in stable New York Heart Association class II-IV HF for at least 3 months and who had a left ventricular (LV) ejection fraction ⬍40% and LV internal dimension in diastole/body surface area ⬎2.9 cm/m2 on echocardiography were eligible. All patients had to be receiving stable pharmacological treatment for HF that could include angiotensin-converting enzyme inhibitors, -blockers, digoxin, diuretics, hydralazine, and/or nitrates. Exclusion criteria included a persistent mean standing SBP ⬍90 mm Hg and serum creatinine ⬎2.0 mg/dL. Eligible patients were stratified according to baseline -blocker therapy and were randomly allocated to receive either oral valsartan or placebo. Treatment with valsartan was initiated at 40 mg twice daily and the dose was doubled every 2 weeks to reach the target dose of 160 mg twice daily, provided SBP was ⱖ90 mm Hg, there were no signs or symptoms of hypotension, and increases in serum creatinine levels did not exceed 50% of the baseline value. Blood pressure was measured at each visit with a sphygmomanometer after 5 minutes of rest in the sitting position. The study had 2 primary end points: death and the first morbid event, which was defined as either death, sudden death with resuscitation, hospitalization for HF, or administration of intravenous inotropic or vasodilatory drugs for ⱖ4 hours without hospitalization. Hospitalization for HF was a secondary end point. Data Analysis Baseline variables grouped by quartiles of baseline SBP were compared with ANOVA for continuous variables and 2 tests for categorical variables. Time to events in various groups were described with Kaplan-Meier curves. Cox proportional-hazards regression models were used to assess the association between time to death from any cause and baseline SBP, changes in SBP during the first 4 months of follow-up, and treatment with valsartan. Baseline SBP values were grouped into quartiles to examine whether baseline SBP was linearly related to the mortality and hospitalization hazards and to examine the effects of valsartan on SBP. The quartile analysis suggested that the relationships between baseline SBP and hazards were not linear, as most of the increased risk was seen in the lowest quartile (quartile 1 [Q1]: SBP ⱕ110 mm Hg). Rather than trying to model a continuous nonlinear relationship, all further analyses were simply carried out comparing Q1 with the other 3 quartiles (Q2, Q3, and Q4) combined. Analyses were repeated using time to first morbid event and first hospitalization for HF as the dependent variable. All of the regression models included baseline age, New York Heart Association class, ischemic etiology, history of hypertension, diabetes, body mass index, pulse, LV ejection fraction, serum sodium, creatinine, uric acid, brain natriuretic peptide, aldosterone, plasma renin activity, hemoglobin, and use of angiotensin- 35 converting enzyme inhibitors, diuretics, digoxin, and -blockers as covariates. When change in blood pressure over the first 4 months was included in the models, all subjects with fatal (n⫽154) or nonfatal events (n⫽332) that occurred during the first 4 months of follow-up were excluded. The changes in SBP from baseline to month 4, month 12, and end of study in the 2 treatment groups were compared at each time point with a 2-sample t test rather than ANOVA to minimize loss of information over time due to deaths and censored follow-up. SPSS statistical software (version 15; SPSS Inc, Chicago, Ill) was used for all analyses. A probability value ⬍0.05 was considered significant without adjustment for making multiple comparisons. The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agree to the manuscript as written. Results Patient Characteristics The baseline blood pressure (mean⫾standard deviation) in the overall population was 124⫾18 mm Hg systolic and 76⫾11 mm Hg diastolic (n⫽5010). Comparison of SBP quartiles in Table 1 indicates that lower SBP was associated with younger age, lower body mass index, lower LV ejection fraction, greater LV internal dimension in diastole, higher levels of aldosterone and plasma renin activity, and lower hemoglobin levels. Lower SBP was also associated with worse New York Heart Association class and Minnesota Living with Heart Failure Questionnaire (MLHF) scores, along with more prevalent use of diuretics, digoxin, and spironolactone. The mean SBP of 149 mm Hg among the large number of patients in Q4 (SBP ⬎135 mm Hg) is remarkable for patients with documented systolic dysfunction who were often treated with medications that lower blood pressure. Baseline Systolic Blood Pressure Related to Morbidity and Mortality Unadjusted time to death, first morbid event, and hospitalization for HF within quartiles of baseline SBP are shown in Figure 1. The risks of all events were similar in the upper 3 quartiles of SBP and increased only in the Q1, suggesting that baseline SBP was not linearly related to the risk (hazard) of death or hospitalization for HF. We did not fit nonlinear models to this relationship. The Cox multivariable model for baseline SBP quartiles is shown in Table 2. With Q3 (patients with normal SBP) as the reference group, only patients in the Q1 were found to have an increased risk of first morbid event and hospitalization for HF, with a trend for an increase risk for death. The upper quartile that contained many patients with elevated SBP was not associated with increased risk. Given these findings, the upper 3 quartiles were collapsed into 1 group for further analyses comparing Q1 with Q2, Q3, and Q4 combined. Patients with baseline SBP in the lowest quartile (Q1: ⱕ110 mm Hg) had a significantly increased adjusted risk of death (hazard ratio [HR], 1.21; 95% confidence interval [CI], 1.03 to 1.43; P⫽0.02), first morbid event (HR, 1.25; 95% CI, 1.10 to 1.40; P⫽0.001), and hospitalization for HF (HR, 1.45; 95% CI, 1.22 to 1.73; P⬍0.001) compared with patients in the upper 3 quartiles (Table 2). Thus, a low baseline SBP was an independent risk factor for morbidity and mortality in this patient population. 36 Circ Heart Fail Table 1. May 2008 Baseline Characteristics by Quartile of SBP Quartile 1 Quartile 2 Quartile 3 Quartile 4 No. 1156 1304 1323 1227 Quartiles 2, 3, and 4 Combined 3854 Age, y† 60⫾12 62⫾11 64⫾11 66⫾10 64⫾11§ Female 19 19 20 22 20 White 88 91 91 92 91§ Ischemic etiology 56 58 58 56 58 Nonischemic etiology 44 42 42 44 42 Diabetes 23 23 28 28 26‡ Atrial fibrillation 14 14 13 15 14 Mean SBP, mm Hg† 102⫾6 115⫾4 128⫾4 149⫾12 130⫾16§ Mean DBP, mm Hg† 67⫾8 73⫾8 77⫾9 84⫾10 78⫾10§ Heart rate, bpm 74⫾13 74⫾12 73⫾13 73⫾13 73⫾13 44 39 34 36 36§ 36⫾23 33⫾23 30⫾22 30⫾23 31⫾23§ History of PND 11 9 8 8 8† Elevated JVP 14 13 14 14 13 Peripheral edema 16 18 17 19 18 79⫾15 79⫾15 80⫾16 79⫾15 79⫾15 26.4⫾4.6 26.8⫾4.4 27.2⫾4.5 27.2⫾4.4 27⫾4§ NYHA III/IV† Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 MLHFQ† Weight, kg BMI, kg/m2† eGFR 57⫾17 58⫾16 58⫾15 58⫾15 58⫾15§ Serum albumin, g/dL 4.2⫾0.4 4.2⫾0.3 4.2⫾0.3 4.2⫾0.3 4.2⫾0.3 S3 presence† LVEF§ LVIDd/BSA§ 29 28 24 23 25§ 25⫾8 26⫾7 27⫾7 28⫾7 27⫾7§ 3.76⫾0.6 3.67⫾0.5 3.62⫾0.5 3.57⫾0.5 3.60⫾0.5§ Background therapy ACE inhibitors 94 94 91 92 92‡ -Blockers 38 34 33 35 34 Diuretics† 89 86 83 84 84 Digoxin* 74 68 65 64 65§ Aspirin 40 39 41 42 41 Statins 33 33 32 29 32 Spironolactone† 7 5 4 3 13.6⫾1.5 13.7⫾1.4 13.8⫾1.5 13.8⫾1.4 13.8⫾1.4§ lnCRP 1.6⫾0.9 1.6⫾0.9 1.6⫾0.8 1.5⫾0.8 1.6⫾0.8 lnNorepinephrine 6.0⫾0.6 6.0⫾0.6 5.9⫾0.6 6.0⫾0.5 5.9⫾0.6 lnBNP 4.6⫾1.4 4.5⫾1.3 4.3⫾1.4 4.5⫾1.3 4.4⫾1.4§ lnaldosterone* 4.8⫾0.9 4.7⫾0.9 4.6⫾0.8 4.5⫾0.8 4.6⫾0.8§ lnPRA* 2.5⫾1.4 1.9⫾1.5 1.4⫾1.5 0.7⫾1.5 4.4⫾1.6§ Hemoglobin, g/dL* 4§ Values are expressed as mean⫾SD or %. DBP indicates diastolic blood pressure; NYHA, New York Heart Association functional class; MLHFQ, Minnesota Living with Heart Failure Questionnaire; PND, paroxysmal nocturnal dyspnea; JVP, jugular venous pressure; BMI, body mass index; eGFR, estimated glomular filtration rate; LVEF, left ventricular ejection fraction; LVIDd, left ventricle internal dimension in diastole; BSA, body surface area; ACE, angiotensin-converting enzyme; CRP, C-reactive protein; BNP, brain natriuretic peptide; and PRA, plasma renin activity. *P⬍0.05, †Pⱕ0.001 for differences between quartiles. ‡P⬍0.05, §P⬍0.01 between Q1 and Q2, Q3, and Q4 combined. Effect of Baseline Systolic Blood Pressure on Effectiveness of Valsartan In the overall population, valsartan use was not associated with a reduction in the risk of death but it did cause a 13.3% reduction in risk of first morbid event (HR, 0.87; 95% CI, 0.77 to 0.97) and a 27.5% reduction in risk for first hospitalization for worsening HF (HR, 0.73; 95% CI, 0.64 to 0.84).17 When the effects of valsartan were estimated separately in patients with baseline SBP in Q1 and in those with baseline SBP the upper 3 SBP quartiles combined, use of valsartan was associated with a 26% decrease in risk of first morbid event in the Q1 patients (HR, 0.74; 95% CI, 0.60 to 0.91; P⫽0.005), compared with a 10% decrease in the combined Q2, Q3, and Q4 group (HR, 0.90; 95% CI, 0.79 to 1.02; Anand et al 100 Effect of Blood Pressure on Heart Failure Outcomes Effect of Valsartan on Systolic Blood Pressure Time to Death % Survival 90 80 SBP <110 mmHg SBP >110 <121 mmHg SBP >121 <135 mmHg SBP >135 mmHg 70 60 0 10 20 30 40 Months Since Randomization Time to First Morbid Event 90 80 70 Overall, treatment with valsartan caused a significant placebo corrected decrease in SBP (mean, [95% CI]) of ⫺4.0 (⫺3.1 to ⫺4.6), ⫺3.9 (⫺2.9 to ⫺4.9), and ⫺3.4 (⫺2.4 to ⫺4.3) mm Hg at 4 months, 12 months, and the end point, respectively (P⬍0.001 at all time points). The change in SBP at 4 months with valsartan by quartiles of baseline SBP is shown in Table 4. Treatment with valsartan did not lower SBP in Q1 (ⱕ110 mm Hg). In fact, the mean SBP increased in both the placebo and valsartan groups as one might expect with regression to the mean. However, the increase in SBP in Q1 was significantly greater in the placebo group (P⬍0.001). In contrast to the lowest baseline SBP quartile, SBP fell in the other 3 combined quartiles in both treatment groups at 4 months, with a significantly greater decrease in the valsartan group. Because the use of valsartan in patients with extremely low SBP may be a concern to the clinicians, we also compared the response to valsartan with the response to placebo in 317 patients whose baseline SBP was ⱕ100 mm Hg (valsartan group mean SBP 95⫾3 mm Hg, n⫽170; placebo group mean SBP 95⫾3 mm Hg, n⫽147). In this group as well, SBP increased in both the valsartan (5⫾13 mm Hg) and placebo (8⫾12 mm Hg) groups, and the increase was significantly greater in the placebo group (Table 4). Safety Profile of Valsartan in Patients With Low Versus High Baseline SBP 60 0 10 20 30 40 30 40 Months Since Randomization Time to Hospitalization 100 % Hospitalizations for Heart Failure Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 % Event Free Survival 100 37 90 80 70 60 0 10 20 Overall, the mean change from baseline to 4 months was greater in the valsartan group than in the placebo group for blood urea nitrogen (1.4⫾3.6 versus 0.7⫾2.2 mmol/dL P⬍0.001), serum creatinine (0.9⫾2.2 versus 0.2⫾1.3 mmol/ dL, P⬍0.001), and serum potassium (0.13⫾0.65 versus decrease of 0.06⫾0.6 mmol/dL, P⬍0.001). However, the effect of valsartan on these parameters was similar in low (Q1) and high (Q2, Q3, and Q4) SBP groups (blood urea nitrogen 1.6⫾4.4 versus 1.4⫾3.3 mmol/L; creatinine 0.12⫾0.28 versus 0.10⫾0.24 mmol/dL; and potassium 0.7⫾0.6 versus 0.12⫾0.7 mmol/L; all P⫽not significant). More patients discontinued the randomized treatment because of hypotension in Q1 (2.9% in valsartan group versus 1.4% in placebo group; P⬍0.001) than in the other quartiles combined (0.7% in valsartan group versus 0.2% in placebo group; P⬍0.001). Months Since Randomization Figure. Kaplan-Meier curves for time to death, first morbid event, and hospitalization for HF by quartile of baseline systolic blood pressure. P⫽0.10). The test for interaction between the effects of valsartan treatment and baseline SBP was not significant, however, as shown in Table 3. Similarly, valsartan caused a 40% decrease in risk of first hospitalization for HF in Q1 patients (HR, 0.60; 95% CI, 0.45 to 0.79, P⬍0.001) and a 23% decrease in patients in the upper 3 quartiles (HR, 0.77; 95% CI, 0.64 to 0.93; P⫽0.006), with interaction that was again not significant. Changes in Systolic Blood Pressure Related to Morbidity and Mortality When the change in SBP over the first 4 months was analyzed as a continuous variable in a multivariable Cox regression model ignoring treatment, a 1-mm Hg increase in SBP was associated with a significant decrease in the risk of death, first morbid event, and hospitalizations for HF in the entire population (Table 5). The interaction between the baseline SBP quartile groups and the change in SBP was not significant for any end point, suggesting that the beneficial effect associated with an increase in SBP over time was not different in the 2 groups defined by baseline SBP (Table 5). Thus, both low baseline SBP and a decrease in SBP over time were associated with an increase in subsequent HF morbidity. 38 Circ Heart Fail May 2008 Table 2. Adjusted Hazard Ratios (95% Confidence Interval) for Mortality, First Morbid Event, and Hospitalizations for HF in Patients Grouped by Baseline SBP Mean Baseline SBP, Mean⫾SD 102⫾5 No. of Patients Mortality, HR (95% CI) First Morbid Event, HR (95% CI) Hospitalization for HF, HR (95% CI) 940 1.12 (0.98 to 1.47) 1.24 (1.05 to 1.45) 1.44 (1.16 to 1.79) 0.08 0.01 0.001 0.97 (0.83 to 1.14) 1.01 (0.81 to 1.26) SBP Quartiles Q1: ⱕ110 mm Hg P Q2: ⬎110 mm Hg and ⱕ121 mm Hg 115⫾4 1110 1.01 (0.82 to 1.23) 0.96 0.71 0.91 128⫾4 1116 Reference group Reference group Reference group 149⫾11 1034 0.94 (0.76 to 1.16) 0.99 (0.84 to 1.17) 0.95 (0.71 to 1.20) 0.58 0.90 0.67 1.21 (1.03 to 1.43) 1.25 (1.10 to ⫺1.4) 1.45 (1.22 to 1.73) 0.02 0.001 ⬍0.001 Reference group Reference group Reference group P Q3: ⬎121 mm Hg and ⱕ135 mm Hg P Q4: ⬎135 mm Hg P Q1 versus Q2, Q3, and Q4 combined Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Q1 102⫾6 940 P Q2, Q3, and Q4 combined 130⫾16 3260 Covariates used in the Cox regression model: age, New York Heart Association class, origin, history of hypertension, diabetes, body mass index, pulse, LV ejection fraction, serum sodium, creatinine, uric acid, brain natriuretic peptide, aldosterone, plasma renin activity, hemoglobin, and use of an angiotensin-converting enzyme inhibitor, diuretics, digoxin, or -blockers. No. in each groups is for those with all covariates. P values are against the reference groups. HR indicates hazard ratio. Effects of Valsartan Treatment Adjusted for Change in Systolic Blood Pressure Because valsartan caused a significant decrease in SBP in baseline Q2, Q3, and Q4 and a smaller increase in SBP in Q1 compared with placebo throughout the study, and because a decrease in SBP was associated with worse outcomes regardless of baseline SBP, we examined whether controlling for the change in SBP after 4 months would alter the apparent effectiveness of valsartan from 4 months to the end of follow-up. When the change in SBP was added to the regression model, the beneficial effects of valsartan on first morbid event and hospitalizations for HF tended to increase in Q1, and to a lesser extent in Q2, Q3, and Q4 (Table 6); however, the blood pressure–lowering effect of valsartan did not deeply undermine its beneficial effects. Furthermore, there was no significant interaction between treatment and change in blood pressure on any of the outcomes, suggesting that the effect of valsartan was not greatly modified by changes in SBP. Discussion The present analysis of Val-HeFT data confirms that low SBP is independently associated with an increase in the risk of mortality and morbidity in patients with moderate to severe chronic HF.7,9 –11 The increased risk did not appear to be linear across all levels of baseline SBP and was observed mainly in patients with a SBP in the lowest quartile (⬍110 mm Hg). A decrease in SBP over time was also found to increase the subsequent risk of adverse outcomes. It is noteworthy that approximately 25% of patients in the present study, all of whom had documented LV systolic dysfunction and were being treated with a diuretic (84%), an Table 3. Effect of Valsartan Versus Placebo on Mortality, First Morbid Event, and Hospitalizations for HF in Patients Grouped by Baseline SBP Mean Baseline SBP, mm Hg Mean⫾SD Q1 P First Morbid Event, HR (95% CI) Hospitalization for HF, HR (95% CI) 0.74 (0.60 to 0.91) 0.60 (0.45 to 0.79) Placebo Valsartan Placebo Valsartan 102⫾5 101⫾6 474 466 0.82 (0.63 to 1.06) 0.13 0.005 ⬍0.001 131⫾16 130⫾15 1657 1623 1.04 (0.88 to 1.23) 0.90 (0.79 to 1.02) 0.77 (0.64 to 0.93) P Q2, Q3, and Q4 combined Mortality, HR (95% CI) No. of Patients 0.64 0.10 0.006 䡠䡠䡠 䡠䡠䡠 䡠䡠䡠 0.15 0.29 0.36 䡠䡠䡠 䡠䡠䡠 䡠䡠䡠 䡠䡠䡠 The Hs (95% CIs) have been adjusted for all covariates. Covariates used in the Cox regression model: age, New York Heart Association class, origin, history of hypertension, diabetes, body mass index, pulse, LV ejection fraction, serum sodium, creatinine, uric acid, brain natriuretic peptide, aldosterone, plasma renin activity, hemoglobin, and use of an angiotensin-converting enzyme inhibitor, diuretics, digoxin, or -blockers. No. in each groups is for those with all covariates. HR indicates hazard ratio. Interaction P 䡠䡠䡠 Anand et al Table 4. Effect of Blood Pressure on Heart Failure Outcomes 39 Effects of Valsartan on SBP at 4 Months by Quartile of Baseline SBP No. of Patients Mean Baseline SBP Mean Change in SBP Placebo-Corrected Change ⫺4.9 (⫺6.4 to ⫺3.5) † Quartiles of Baseline Systolic Blood Pressure Q1: ⱕ110 mm Hg Valsartan 509 101⫾5 1.2⫾12 Placebo 539 102⫾5 6.1⫾12 Valsartan 629 115⫾4 ⫺2.1⫾14 Placebo 574 115⫾4 1.2⫾13 Q2: ⬎110 mm Hg and ⱕ121 mm Hg ⫺3.2 (⫺4.8 to ⫺1.7) † Q3: ⬎121 mm Hg and ⱕ135 mm Hg Valsartan 617 128⫾4 ⫺7.2⫾15 Placebo 616 127⫾4 ⫺2.1⫾14 ⫺5.1 (⫺6.7 to ⫺3.5) † Q4: ⬎135 mm Hg Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Valsartan 543 149⫾12 ⫺12.5⫾18 Placebo 601 149⫾11 ⫺9.1⫾16 ⫺3.4 (⫺5.4 to ⫺1.4) † Q1 versus Q2⫹Q3⫹Q4 Q1 Valsartan 509 101⫾5 1.2⫾12.3 Placebo 539 102⫾5 6.1⫾11.8 ⫺4.9 (⫺6.4 to ⫺3.5† Q2⫹Q3⫹Q4 Valsartan 1789 130⫾16 ⫺7.0⫾16.2 Placebo 1791 131⫾16 ⫺3.4⫾14.9 Valsartan 170 95⫾3 4.7⫾13 Placebo 147 95⫾3 8.0⫾12.3 ⫺3.6 (⫺4.6 to ⫺2.6) † SBP ⱕ 100 mm Hg ⫺3.4 (⫺6.2 to ⫺0.5)* Values are expressed as n, mean⫾SD. *P⬍0.05, †P⬍0.01 for change in SBP comparing valsartan to placebo groups. angiotensin-converting enzyme inhibitor (92%), and sometimes a -blocker (35%), still had SBP ⬎135 mm Hg (mean 149 mm Hg). The reason for the high SBP is not obvious. These patients tended to be older, to have better LV function, and to have slightly less medication use than others in the study. Interestingly, these patients did not have a significantly increased risk of adverse events. In the African American Heart Failure Trial (A-HeFT), approximately 25% patients with systolic dysfunction had similarly elevated blood pressure at baseline.12 Similar findings of elevated SBP have also been reported recently in patients admitted with acute HF from the Organized Program To Initiate life-saving treatment in hospitalized patients with Heart Failure (OPTIMIZE-HF) registry. In this registry, the majority of patients with elevated SBP had preserved LV function. Although the pathophysiology of systolic hypertension might be different in patients with preserved LV systolic function, if elevated SBP is common among patients with chronic HF and LV systolic dysfunction and the elevated SBP is not associated with increased risk of adverse events (although the risk of stroke Table 5. Effect of Change in SBP From Baseline to 4 Months on the Adjusted HRs (95% CIs) for Mortality, First Morbid Event, and Hospitalizations for HF Analyzed as a Continuous Variable in Patients Grouped by Quartile No. of Patients Mortality, HR (95% CI) First Morbid Event, HR (95% CI) Hospitalization for HF, HR (95% CI) 3897 0.993 (0.988 to 0.999) 0.992 (0.987 to 0.996) 0.989 (0.983 to 0.995) 0.024 ⬍0.001 ⬍0.001 853 1.0 (0.986 to 1.01) 0.994 (0.983 to 1.004) 0.986 (0.972 to 0.999) 0.90 0.23 0.035 3044 0.992 (0.986 to 0.998) 0.991 (0.986 to 0.996) 0.989 (0.983 to 0.996) P 0.014 0.001 0.001 Interaction P 0.35 0.50 0.88 Continuous variable P Q1 versus Q2 ⫹Q3⫹Q4 Q1 P Q2 ⫹Q3⫹Q4 Covariates used in the Cox regression model: baseline SBP, age, New York Heart Association class, origin, history of hypertension, diabetes, body mass index, pulse, LV ejection fraction, serum sodium, creatinine, uric acid, brain natriuretic peptide, aldosterone, plasma renin activity, hemoglobin, and use of an angiotensin-converting enzyme inhibitor, diuretics, digoxin, or -blockers. No. in each groups is for those with all covariates. HR indicates hazard ratio. 40 Circ Heart Fail May 2008 Table 6. Effect of Controlling for Changes in SBP on the Effect of Valsartan on Mortality, First Morbid Event, and Hospitalizations for HF Placebo Versus Valsartan, Mean Difference in SBP, mm Hg Mortality* First Morbid Event* Hospitalization for HF* 0.82 (0.63 to 1.06) 0.74 (0.60 to 0.91) 0.60 (0.45 to 0.79) Baseline SBP Q1 (n⫽853) Without change in SBP in model P With change in SBP in model ⫺4.9 P 0.13 0.005 ⬍0.001 0.75 (0.54 to 1.03) 0.63 (0.49 to 0.82) 0.52 (0.37 to 0.73) 0.08 0.001 ⬍0.001 1.07 (0.87 to 1.29) 0.88 (0.76 to 1.02) 0.75 (0.62 to 0.91) 0.48 0.08 0.003 1.05 (0.86 to 1.28) 0.83 (0.71 to 0.97) 0.69 (0.56 to 0.84) 0.65 0.015 ⬍0.001 Baseline SBP Q2⫹Q3⫹Q4 (n⫽3044) Without change in SBP in model P With change in SBP in model ⫺3.6 Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 P *HR (95% CI) from Cox regression model; see Data Analysis section for a list of covariates. Groups include only those who had a value for all covariates. could not be assessed), one wonders whether the high SBP should or could be decreased. This important question needs to be addressed by further research. Although the beneficial effects of valsartan in reducing the number of morbid events over time and of hospitalizations for HF tended to be relatively higher in the patients with the baseline SBP ⬍110 mm Hg (Q1) as compared with those with SBP above 110 mm Hg, statistical test for interaction between treatment and baseline SBP did not detect a significant difference in effect in the 2 subgroups. Interestingly, valsartan did not actually decrease SBP in patients with the lowest pretreatment values, including those in Q1 with a SBP ⬍110 mm Hg or even the subgroup with a SBP ⱕ100 mm Hg, even though valsartan was associated with a smaller increase in SBP as compared with placebo. In contrast, valsartan did cause a significant decrease in SBP in patients with higher baseline SBP that could have potentially counteracted its beneficial effects on morbidity rates. However, the present analysis did not indicate that the benefits of valsartan depended on baseline SBP or changes in SBP during the first 4 months of treatment, suggesting dissociation between the effects of valsartan on SBP and clinical outcomes. It should be emphasized, however, that these conclusions are based on the lack of significance for interaction. Although interaction tests can be useful exploratory tools, the lack of statistical significance for interaction tests may be partially due to their relatively low power. Thus, any inference based on interaction test results should be made with caution. The observation that blood pressure did not actually decrease in the group with low initial SBP suggests that the addition of valsartan was usually well tolerated by patients with moderate to severe chronic HF. Low SBP blood pressure should not preclude a trial of these agents that appear to benefit all patients. Is there a threshold SBP below which the use of an angiotensin receptor blocker is associated with deleterious outcomes? Although the present study was not designed to address this question, we did find that even in the small subgroup of 317 patients with a SBP between 90 and 100 mm Hg, valsartan appeared to have been well tolerated, on average, without frequent deleterious drops in blood pressure. Because patients with low initial SBP are at a greater risk of HF morbidity and mortality, and because a trend for greater risk reduction in morbidity was seen with valsartan for the low SBP patients (even though the risk reduction for HF hospitalization was significant for both low and high SBP patients), patients with low SBP could be expected to be more likely to benefit from this treatment. Moreover, the increases in serum creatinine, blood urea nitrogen, and potassium were no different in patients in baseline SBP Q1 or than those in Q2, Q3, and Q4, suggesting that introduction of valsartan even in patients with low SBP may not precipitate major adverse effects. However, a patient’s baseline SBP had to be ⬎90 mm Hg to be eligible for this clinical trial or for an increase in the dose of the study medication. Thus, these data cannot address the use or benefits of valsartan in patients with HF and a SBP less than this level. If low baseline SBP and a decrease in SBP over time are associated with worse outcomes, how can we explain the apparent dissociation between the blood pressure–lowering effects of valsartan and clinical outcomes? The fact that valsartan did not lower blood pressure in patients with a low baseline SBP could be explained by an improvement in the hemodynamics, although these were not measured in the present study. In patients with chronic HF, a low stroke volume threatens the arterial blood pressure and leads to a baroreceptor-mediated activation of several vasoconstrictive neurohormones that help to preserve blood pressure by increasing arterial impedance.19 The increase in impedance is, however, deleterious to the failing heart and further reduces the stroke volume, worsening hypotension. Vasodilators such as sodium nitroprusside reverse the functional abnormalities acutely by improving stroke volume and may increase blood pressure.10,20,21 Thus, the vasodilatory effects of valsartan might have lowered arterial impedance in patients with the Anand et al Effect of Blood Pressure on Heart Failure Outcomes Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 lowest SBP who would be expected to have the highest impedance, thereby increasing the cardiac output and maintaining blood pressure. Over the long term, valsartan use was associated with an improvement in LV ejection fraction22 and a decrease in the levels of several neurohormones, including brain natriuretic peptide, norepinephrine, and aldosterone.23,24 Thus, the dual effects of lowering impedance (BP-lowering effect) and improving LV structural remodeling might have contributed to the beneficial effects of valsartan on hemodynamics and subsequently to reduced morbidity and mortality. In conclusion, the present secondary analysis of data from a randomized controlled clinical trial suggests that patients with low systolic blood pressure can benefit from valsartan therapy without an inordinate risk of deleterious hypotension. Patients with low SBP are at least as likely as and perhaps more likely to benefit from valsartan therapy as those with normal or high pretreatment blood pressures. Patients with low blood pressure are at the highest risk and, therefore, have the greatest need for aggressive therapy. Judicious use of valsartan in such patients is more likely to produce benefit than use in those with higher blood pressures, although patients with low or high SBP appear to benefit. However, the data were not sufficient to determine whether these findings are generalizable to patients with SBP well below 100 mm Hg. Regardless, blood pressure reduction does not seem to greatly counteract the favorable effects of valsartan on hospitalization for HF and morbidity and cannot be used as a surrogate for efficacy. Many patients in the present analysis had HF, systolic dysfunction, and prescriptions for antihypertensive medications but still had elevated SBP; however, they were not at increased risk of adverse events. Because reductions in SBP tended to be associated with increased risk, further research is needed to determine whether the SBP should be reduced in patients with these characteristics and how this might be achieved, if desirable. Finally, it is important to emphasize that findings of the present study do not apply to patients with acute decompensated HF. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Sources of Funding Novartis Pharmaceutical provided a grant for the study. Resources of the Minneapolis VA Medical Center supported this analysis in part. Dr Rector was supported by VA Clinical Science and Health Services Research & Development Grants 04S-CRCOE-001 and HFP-98-001. 15. 16. Disclosures Drs Anand, Holwerda, and Cohn received research grants and honoraria from Novartis. The other authors report no conflicts. 17. References 18. 1. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies (published correction appears in Lancet. 2003;361:1060). Lancet. 2002;360:1903–1913. 2. World Health Organization. World Health Report 2002; Reducing Risk, Promoting Healthy Life. Geneva, Switzerland: World Health Organization; 2002. 3. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; 19. 20. 21. 41 National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206 –1252. Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ, Levy D; Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068 –3072. Dahlöf B, Lindholm LH, Hansson L, Scherstén B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338:1281–1285. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–3264. Fonarow GC, Adams KF Jr, Abraham WT, Yancy CW, Boscardin WJ; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293:572–580. Lee DS, Austin PC, Rouleau JL, Liu PP, Naimark D, Tu JV. Predicting mortality among patients hospitalized for heart failure: derivation and validation of a clinical model. JAMA. 2003;290:2581–2587. Aaronson KD, Schwartz JS, Chen TM, Wong KL, Goin JE, Mancini DM. Development and prospective validation of a clinical index to predict survival in ambulatory patients referred for cardiac transplant evaluation. Circulation. 1997;95:2660 –2667. Anand IS, Tam SW, Rector TS, Taylor AL, Sabolinski ML, Archambault WT, Adams KF, Olukotun AY, Worcel M, Cohn JN. Influence of blood pressure on the effectiveness of a fixed-dose combination of isosorbide dinitrate and hydralazine in the African-American Heart Failure Trial. J Am Coll Cardiol. 2007;49:32–39. Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, Anand I, Maggioni A, Burton P, Sullivan MD, Pitt B, Poole-Wilson PA, Mann DL, Packer M. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006;113:1424 –1433. Taylor AL, Ziesche S, Yancy C, Carson P, D’Agostino R Jr, Ferdinand K, Taylor M, Adams K, Sabolinski M, Worcel M, Cohn JN; AfricanAmerican Heart Failure Trial Investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure (published correction appears in N Engl J Med. 2005;352:1276). N Engl J Med. 2004;351: 2049 –2057. Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, Yusuf S, Pocock S; CHARM Investigators and Committees. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362:759 –766. The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure: results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987; 316:1429 –1435. The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302. Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, Dunkman WB, Jacobs W, Francis GS, Flohr KH, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure: results of a Veterans Administration Cooperative Study. N Engl J Med. 1986;314:1547–1552. Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345: 1667–1675. Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, Stough WG, Yancy CW, Young JB, Fonarow GC; OPTIMIZE-HF Investigators and Coordinators. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–2226. Anand IS, Ferrari R, Kalra GS, Wahi PL, Poole-Wilson PA, Harris PC. Edema of cardiac origin: studies of body water and sodium, renal function, hemodynamic indexes, and plasma hormones in untreated congestive cardiac failure. Circulation. 1989;80:299 –305. Cohn JN, Franciosa JA. Vasodilator therapy of cardiac failure (second of two parts). N Engl J Med. 1977;297:254 –258. Cohn JN, Franciosa JA. Vasodilator therapy of cardiac failure: (first of two parts). N Engl J Med. 1977;297:27–31. 42 Circ Heart Fail May 2008 22. Wong M, Staszewsky L, Latini R, Barlera S, Volpi A, Chiang YT, Benza RL, Gottlieb SO, Kleemann TD, Rosconi F, Vandervoort PM, Cohn JN; Val-HeFT Heart Failure Trial Investigators. Valsartan benefits left ventricular structure and function in heart failure: Val-HeFT echocardiographic study. J Am Coll Cardiol. 2002;40:970 –975. 23. Cohn JN, Anand IS, Latini R, Masson S, Chiang YT, Glazer R; Valsartan Heart Failure Trial Investigators. Sustained reduction of aldosterone in response to the angiotensin receptor blocker valsartan in patients with chronic heart failure: results from the Valsartan Heart Failure Trial. Circulation. 2003;108:1306 –1309. 24. Latini R, Masson S, Anand I, Judd D, Maggioni AP, Chiang YT, Bevilacqua M, Salio M, Cardano P, Dunselman PH, Holwerda NJ, Tognoni G, Cohn JN; Valsartan Heart Failure Trial Investigators. Effects of valsartan on circulating brain natriuretic peptide and norepinephrine in symptomatic chronic heart failure: the Valsartan Heart Failure Trial (Val-HeFT). Circulation. 2002;106:2454 –2458. CLINICAL PERSPECTIVE Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Lowering high blood pressure greatly reduces the incidence of heart failure. In the presence of heart failure with systolic dysfunction, however, low blood pressure and drops in blood pressure are associated with increased risk of hospitalization and death. Many effective medications that are used for heart failure, including those that decrease angiotensin II, reduce blood pressure, which could reduce their beneficial effects. Concerns about hypotensive effects often limit use of these medications. The present secondary analysis of data from the Valsartan Heart Failure trial indicates that neither a low pretreatment systolic blood pressure (SBP) nor changes in SBP reduced the beneficial effects of valsartan. As expected, valsartan did reduce SBP in patients in the upper 3 quartiles of SBP but not those in the lowest quartile who had a baseline SBP between 90 and 110 mm Hg. Valsartan reduced the risk of hospitalization for heart failure and the first morbid event in the lowest SBP quartile and the other 3 quartiles. Adjustments for the changes in SBP on therapy did not substantially reduce these beneficial effects. Judicious use of valsartan should be considered for patients who present with low SBP and have the highest risk of hospitalization and death. Effect of Baseline and Changes in Systolic Blood Pressure Over Time on the Effectiveness of Valsartan in the Valsartan Heart Failure Trial Inder S. Anand, Thomas S. Rector, Michael Kuskowski, Sabu Thomas, N.J. Holwerda and Jay N. Cohn Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 10, 2017 Circ Heart Fail. 2008;1:34-42 doi: 10.1161/CIRCHEARTFAILURE.107.736975 Circulation: Heart Failure is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2008 American Heart Association, Inc. All rights reserved. Print ISSN: 1941-3289. Online ISSN: 1941-3297 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circheartfailure.ahajournals.org/content/1/1/34 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation: Heart Failure can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation: Heart Failure is online at: http://circheartfailure.ahajournals.org//subscriptions/