* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download mechanisms used by some parasitic protozoa to evade the immune
Survey
Document related concepts
Transcript
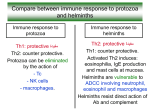
Published by A.P.E. Research and Reviews in Parasitology, 59 (3-4): 71-83 (1999) © 1'999 Asociaci6n de Parasit61ogos Espafioles (A.P.E.) Printed in Barcelona, Spain MECHANISMS USED BY SOME PARASITIC PROTOZOA TO EVADE THE IMMUNE RESPONSE S. ZAMBRANO-VILLAI, D.M. ROSALES-BORJAS2 & L. ORTIZ-ORTIZ3 iCenlro Universitario de Ciencias Exactas e lngenierias, Universidad de Guadalajara, Guadalajara, Jalisco, Mexico 2Hospital Universitario Dr. Miguel Orad, Guanare, Edo. Portuguesa, Venezuela 3Departamento de Inmunologia, Instituto de Investigaciones Biomedicas, UNAM, Apartado PostaL 700228, Ciudad Universitaria, 04510 Mexico D.F., Mexico Received 10 January 1998; accepted 28 July 1999 REFERENCE: ZAMBRANO-VILLA (S.), ROSALES-BORJAS (D.M.) & ORTIZ-ORTIZ (L.), the immune response. Research and Reviews ill Parasitology, 59 (3-4): 71-83. 1999.- Mechanisms used by some parasitic protozoato evade SUMMARY: The present review describes mechanismsto evade the host immune response used by some protozoa that are pathogenicto man. Relatively complex mechanismsare discussed, beyond the encystment shown by some parasites.These allow protozoato penetrateand multiplywithin the cell, vary their surface antigens, eliminate their protein coat to evade the effect of complement and/or antibody,and modulatethe host immune response acting at effector level and causing immunosuppressionthrough induction of suppressor cells which include macrophagesand T lymphocytes. In some cases, immunosuppressionis related to intrinsic properties of parasite products; in others, protozoa use antigenic mimicry involved in the autoimmunitywhich frequently appears in associationwith parasitic diseases. However, among the most interestingmechanismsof evasion is the one by which parasites preferentially induce a particular subset of T helper cells which secrete cytokines, thus modulating the host immune response. KEYWORDS:Immune response,Protozoa, immunosuppression,cytokines, T helper cells, CD4, CD8. INTRODUCTION The host-parasite relationship maintains an equilibrium as long as there is harmony between the two components. It ends when one of them senses danger of survival or damage, and that is when the host tries to eliminate the parasite, and the parasite struggles to survive, attempting to escape the host's defense mechanisms. This contest will result in either elimination of the parasite or infection of the host, leading to various possible pathologies and sometimes to the host's death. The host's defense mechanisms include everything from the primary barriers to the most elaborate devices, which involve a large variety of cells and molecules capable of specific recognition and elimination of many invasive agents. These cells and molecules are organized and act together dynamically (SHER & SCOTT, 1993). In spite of the high amount of antigens presented by the parasite to the host, and the host's vast immune and inflammatory response, parasites manage to survive within the host for lengthy periods. This may be due to genetic factors (WAKELIN & BLACKWELL, 1993) or to alternative causes such as the host's incapacity to respond effectively, due to an immune response diminished by environmental or physiological factors (GoDFREY-FAUSSETT et al., 1993). Protozoa are responsible for several human diseases, among them malaria, sleeping sickness, Chagas disease, amebiasis, giardiasis, toxoplasmosis and leishmaniasis. The host immune response and its effectiveness largely depend on the type of parasite and its site. Some parasites present extracellular stages where the humoral immune response is effective, while others present intrace- llular stages where they are protected from this response, even though the infected cell may be attacked by mechanisms of cell-mediated immunity (SHER & SCOTT, 1993). In spite of this, parasites manage to survive by various mechanisms, some of which have been compiled in the present review. MALARIA Malaria affects more than 250 million people, and causes death in 1%. The infection is caused by Plasmodium vivax, P. malariae, P. ovale and P. falciparum. The first three cause the classic symptoms of malaria, i.e., fever and malaise with intermittent paroxysms. On the other hand, P.falciparum is known for its virulence and prevalence (RrLEY, HVIID & THEANDER, 1994). In this parasitemia, Plasmodium has shown to be resistant to drugs, besides the resistance to DDT exhibited by the vector, the Anopheles mosquito. The infection involves a complex life-cycle with intra- and extracellular stages. In endemic regions the immune response to the parasite is poor, particularly in children, who become more susceptible and exhibit a more severe pathology. Adults present a lower infection prevalence and less severe symptoms, suggesting protection (CHRISTOPHERS, 1924). The poor immune response may be due to changes presented by the parasite's surface as it passes through its various stages, from sporozoite to merozoite and gametocyte, and to the intracellular phase inside the liver or erythrocyte. We have to consider that the most susceptible stage of the parasite is the sporozoite and that its duration is very short, not even an hour, before it infects the liver cells. This is a 72 very short period for the immune system to mount a response to eliminate the parasite, and even if this should occur, the protozoan is capable of evading the effect of an antibody by eliminating its protein cover, the circumsporozoite, a 45kDa antigen (KUBY, 1997). Each phase of the cellular cycle is associated with the expression of stage- and species-specific proteins, many of which are inserted into the parasite membrane surface and seem to be the target of the naturally acquired immune response (DAY & MARSH, 1991). Stage-specific proteins tend to be highly polymorphic and antigenically variable (MCCUTCHANet al., 1988). In contrast, some internal antigens are less variable and seem to be at least partially conserved among Plasmodium species. Some of these are liberated by infected erythrocytes in large quantities during the rupture of the schizont and seem to be involved in triggering the cascade of cytokines which produce most of the symptomatology and pathology of the infection (KWIATKOWSKI, 1991; TAVERNE et al., 1990). Evidence suggests that acute malaria infection induces a temporary reduction of the immune response. An association with increased susceptibility to infections has been observed during this phase. It is not known if these effects are due to the parasitemia or to the generalized physiopathological effects of the disease (RrLEY, HVIm & THEANDER,1994). During acute infection with P. jalciparum, circulating T-Iymphocytes are reduced in number (WYLER, 1976; GREENWOOD,ODULOJU& STRATTON,1977; MERINOet al., 1986) accompanied by a decrease in the lymphoproIiferative response and in the cytokines of peripheral blood mononuclear cells (PBMC) when stimulated by malarial antigens (HO et al., 1986; THEANDER et al., 1986; RILEY et al., 1988). It has been suggested that the loss of response of the PBMC in patients with malaria may be due to the activation of CD8+ suppressor cells (LELCHUK, SPROTT & PLAYFAIR, 1981; THEANDERet al., 1986), although the role of antigen specific suppressor cells during acute malaria is controversial (WHITTLE et al., 1990; Ho et al., 1986). The decrease in PBMC response to malarial antigens during acute infection may also be due to generalized physiologic effects of the febrile disease. Thus, the depression observed in vitro of the proliferative response to malaria soluble exoantigens can be partially reverted by the addition of indomethacin to cell cultures, indicating that prostaglandins secreted by activated macrophages may be responsible for the effect (RILEY et al., 1989b). Furthermore, acute phase proteins, which are liberated in serum during infection, can bind to the surface of lymphoid cells. This may inhibit lymphocyte proliferation (CHERESH,HAYNES& DTSTASTO,1984), and thus may also be responsible of the suppression observed in vitro against malarial and other antigens (THEANDERet al., 1987; RILEYet al., 1988). It has also been reported that some malarial antigens can induce suppression directly. Thus, a low molecularweight glycoprotein from P. berghei, which in vivo sup- S. ZAMBRANO-VILLA, D.M. ROSALES-BORJAS & L. ORTIZ-ORTIZ presses the primary humoral immune response to thymus-dependent antigens (SROUR, SEGRE & SEGRE, 1988) and a schizont extract from P. jalciparum which in vitro suppresses the Iymphoproliferative response of a malarial and other soluble antigens (RILEY et al., 1989a) have been isolated. The mechanisms responsible for suppression are not well known, although it has been suggested that hemozoin accumulation derived from the parasite in macrophages may inhibit their accessory function (MORAKOTE& JUSTUS, 1988). AFRICAN TRYPANOSOMIASIS Another disease in which the parasite uses interesting mechanisms to evade the immune response of the host is the sleeping sickness produced in humans by two subspecies of African trypanosomes, Trypanosoma brucei gambiense and T. brucei rhodesiense, and in cattle by T. brucei brucei, T. vivax, T. evansi and T. congolense. These trypanosomes live in the blood of the host and show no intracellular stages, which makes them a target for antibody-mediated destruction. The protozoan remains in circulation where it divides each 4 to 6 hours. The infection presents various stages, during the initial or systemic stage the parasite divides in the blood and progresses to a neurologic stage in which it infects the central nervous system, producing megaloencephalitis with eventual loss of conscience (VICKERMAN, 1985). During the initial stage, the parasite grows indefinitely in waves, as a result of the humoral immune response which eliminates, with the first wave, most parasites by opsonization in liver macrophages, more than by complement-mediated lysis (URQUHART& HOLMES, 1987). However, those which survive due to a modification of their glycoproteic coat, a phenomenon known as antigenic variation (GRAY & LUCKINS, 1976), start a new surge which is once more suppressed by the formation of antibodies against the new antigens present on the surface of the parasite. However, a small number of parasites survive and change their superficial coat again, starting a new surge, and so on. This glycoproteic coat, called variant surface glycoprotein (VSG) (VICKERMAN, 1978), is generated by rather infrequent genetic processes in which the organism carries a large repertoire of VSG genes, each one coding for a VSG with different primary sequence, particularly at the N termini, and sequence similarities near the C termini (MATTHYSSENSet al., 1981; RICE-FIGHT, CHEN & DONELSON, 1981). An interesting aspect is that the parasite only expresses a single VSG gene at anyone time. The activation of the VSG gene results in its duplication and transposition to an active site of transcriptional expression on the telomeric end of specific chromosomes. The activation of the new gene displaces the previous gene from the telomeric site of expression. Even though several VSG genes can potentially express themselves, this is limited by unknown control mechanisms which allow only one site 73 Immune evasion mechanisms by protozoa of expression at a time (BORST & CROSS, 1982; LAURENTet al., 1983; MYLER et al., 1984; VAN DER PLOEG, 1987). In consequence, this repeated antigenic change of VSG in the trypanosome allows it to evade the humoral immune response, resulting in successive surges of parasitemia. This phenomenon makes it difficult to develop a vaccine against the disease. Since the pathogenesis is linked to the incapacity of the untreated patient to eliminate the parasite, attempts have been made to determine how the parasite interacts with the immune system and alters the cytokine balance and that of other mediators, thus allowing the pathology to develop. During development of the parasitemia several populations of Band T lymphocytes are altered (URQUHARTet al., 1973; PEARSONet al., 1978; SACKS & ASKONAS, 1980; GASBARREet aI., 1981). During infection, Band T lymphocytes proliferate and respond against a series of antigens unrelated to the parasite (HUDSONet al., 1976; ASKONASet al., 1979), but surprisingly, the capacity to induce T cell-dependent cell responses decreases, with progressive alteration of the helper, suppressor and cytotoxic T-cell functions (GOODWINet aI., 1972; PEARSONet al., 1979; CHAROENVIT, CAMPBELL& TOKUDA, 1981), until the disease continues with the sole function of the T -independent B cells, which generally increase (HOUBA, BROWN & ALLISON, 1969; MURRAY et al., 1974; ASKONASet al., 1979). In consequence, the parasite induces paradoxical changes characterized by polyclonal expansion associated to immunosuppression (lAYAWARDENA& W AKSMAN, 1977; DIFFLEY, 1983). The T cell-dependent immune response against the persistent trypanosoma antigens is depressed, although the T -independent B cell response to the VSG surface epitopes (REINITZ& MANSFIELD,1990; SILEGHEMet al., 1994) can very likely control subsequent parasitemias. It has also been observed that the parasite activates the macrophages, initiating a series of events which result in immunosuppression. The macrophage thus activated causes a change in the pattern of cytokines produced by activated T cells, regulating an increase in interferon(IFN) "I and a decrease of expression of the IL-2 receptor, which causes an impaired proliferative responsiveness (SILEGHEMet al., 1994). These results indicate that the parasite molecules which trigger the cascade are not suppressor factors but factors which activate the macrophage. These alterations may be partially responsible for the altered immune response and other aspects of pathogenesis. AMERICAN TRYPANOSOMIASIS Chagas disease is produced by another Trypanosoma cruzi. This parasite affects million people in the American continent, causes has no cure and it is a main factor death. The disease is transmitted to man trypanosoma, more than 20 the disease it of premature via the insect vector's feces. The parasite has a life-cycle with intraand extracellular phases. In the blood stream it is found as flagellated trypomastigotes and intracellularly as amastigotes. The amastigote divides by binary fission forming parasite nests or pseudocysts, particularly in cardiac muscle fibres. The disease is frequently lethal in children and infants, but in adults the initial infection often turns into a chronic disease, sometimes after a long interval, causing an illness characterized by megacardia with megacolon, megaesophagus and degeneration of the central and peripheral nervous system. A mystery in this disease are the pathologic alterations which vary from subclinical to lethal in a period which can be short or long. Another characteristic is that the infection is generally associated with suppression of the immune response (BRENER, 1980). In a study performed on mice infected with trypomastigotes which were immunized 5 days later with donkey erythrocytes, the response to the red blood cells, both by IgM and by IgG, was significantly reduced (CLINTONet aI., 1975). A similar effect was observed with other T-dependent and T-independent antigens (RAMOS et al., 1978). The observed immunosuppression became more evident later on as the parasitemia advanced in blood and tissues. Surprisingly, phagocytic activity of the immunosuppressed animals was increased, which suggested that suppression at least was not due to a blocking of the mononuclear phagocytic system, as has been observed in leishmaniasis (CLINTONet aI., 1969) and in African trypanosomiasis (GOODWINet al., 1972). On the other hand, a similar phenomenon was noticed in experimental infections with another protozoan, Plasmodium vinckei (Cox, BTLBEY& NICOL, 1964), in which increased activity of the mononuclear phagocytic system is associated with important immunosuppression (SALAMAN, WEDDERBURN& BRUCE-CHWATI, 1969; BARKER, 1971; GREENWOOD,PLAYFAIR& TORRIGIANT,1971). With respect to the management of antigen by peritoneal cells of animals infected by T. cruzi, they did not differ in their capacity to bind antigen nor in the immunogenicity of the antigen associated with cells, compared to observations in normal animal cells (RAMOS et al., 1978). In support of this, it was found that animals infected with T. cruzi developed nonspecific resistance to challenge with an unrelated intracellular microorganism Listeria monocytogenes, associated with an increased mononuclear phagocytic activity. This antibacterial response of animals infected with T. cruzi has been reported in infections by other protozoa (MAUEL & BEHIN, 1974). As with other microorganisms, T. cruzi and other protozoa induce polyclonal B lymphocyte activation, which is characterized by the spontaneous appearance of antibodies, predominantly of the IgM class, against antigens not related with the parasite (ORTIZ-ORTIZet al., 1980). Polyclonal activation may be responsible for the immunoglobulin alterations reported for Chagas disease (SCHMUNISet aI., 1978). However, it is not known whether this phenomenon participates in the human infection with this protozoan. 74 The nonspecific stimulation of antibody-forming cells to soluble proteins such as human globulin and to syngeneic erythrocytes is particularly interesting, considering the potential for autoimmune diseases after parasitic infection. If B cells specific for autoantigens are stimulated either by infectious organisms or by the host's inflammatory response to the parasite, the resulting autoantibodies may potentially induce autoimmune disease (ORTIZ-ORTIZet al., 1980). The antigenic similarity of the parasite with the host (molecular mimicry) may be a further mechanism used by the parasite to evade the immune response of the host and also be responsible for autoimmunity in Chagas disease. Autoantibodies have been reported against cardiac tissue (endocardium, vascular and interstitial tissue), Schwann cells, laminin, striated muscle and neurons. By crossed absorption studies, it has been demonstrated that these autoantibodies define epitopes shared by the host and the parasite. The autoimmune basis for the chronic pathology has been experimentally demonstrated by adoptive transfer studies (non-adherent spleen cells) in mice, demonstrating that the host and the parasite share antigens, which may be the reason for T cell-mediated autoimmunity (HALL, 1994). Immunosuppression observed during experimental infection by T. cruzi has been confirmed by various authors, who have contributed to its better understanding. Thus, RAMOSet al. (1978) found that the lymphoproliferative response induced with Con A in spleen cells of BALB/c mice was suppressed by T cells obtained from mice infected with T. cruzi. The spleen cells from infected mice also showed alterations in IL-2 production when stimulated with Con A which was not restored by addition of IL-l, and addition of exogenous IL-2 did not correct lymphoproliferative suppression (HAREL-BELLANet al., 1983, 1985). However, addition of exogenous IL-2 in a murine model of experimental infection did restore suppression of the response to sheep erythrocytes determined in the spleen by the production of antibody-forming cells (TARLETON& KUHN, 1984). Suppressor cells have been characterized as spleen-adherent Tny-ILyt-z (TARLETON,1988a, b). The suppressor effect has been reverted by incubation in culture medium, suggesting that it could have been caused directly by the parasite on the lymphocytes (KIERSZENBAUNet al., 1989). In a recent study of patients with chronic chagastic miocarditis, an association has been reported between the increase in T CD8+ cells and the presence of T. crusi antigen, while the number of T CD4+ cells did not vary significantly, which indicates that the T CD8+ cells are responsible for immune activation in this disease. The correlation between T. cruri antigens and T CD8+ cell increase strongly suggests a direct influence of the parasite on the development of miocarditis (HIGUCHI et al., 1997). Besides, T. cruzi extend their permanence in the vertebrate blood stream through the expression of surface S. ZAMBRANO- VILLA, D.M. ROSALES-BORJAS & L. ORTlZ-ORTlZ molecules with anti-complementary properties (T-DAF, gp58/68 and gp160) which confer them resistance to seric complement-dependent lysis (FISHER et al., 1988; JOINERet al., 1988; NORRIS, HART & SO, 1989), surface molecule turnover through the endocytic pathway, of great use to the parasite for eliminating membranebound antibodies (TEXEIRA& SANTANA,1989), and the liberation of immune membrane complexes by means of phospholipase which degrades anchoring glycoproteins (ALMElDA et al., 1994). Recently, it has been reported that the IgM bound to the membrane on the trypomastigote surface limits the binding of IgG to the parasite and alters the elimination of the parasite induced by IgG in strains Y and CL, thus favoring its transmission to the hematophagous vector host (GARCIAet al., 1997). AMEBIASIS The intestinal protozoan Entamoeba hystolytica is the causal agent of amebiasis, a disease of world-wide distribution. Endemicity and mortality rates are very high in Africa, South America, India and Mexico (W ALSH, 1986). In Mexico, where seroprevalence was found to be 8,41 % in representative samples from the 32 examined entities (CABALLERO-SALCEDO et al., 1994), the disease is endemic with areas of high predominance not related to climatic conditions. Exposure to infectious contact with amebas occurs at all ages, with high frequency at school age. Poor sanitary conditions, low educational level and bad hygienic habits contribute to the spread of the disease. The human host is infected by parasite cysts which then turn into trophozoites and colonize the lumen of the colon, where they multiply and live as commensals. However, when trophozoites lyse the colon epithelial cells and penetrate the intestinal mucosa, they can cause massive and fatal destruction of the host tissues. The most relevant characteristic of this parasite is its extensive cytolytic capacity, which can be considered as its main pathogenic function. It has been reported that after cell-cell contact, the ameba liberates a protein into the intercellular space which inserts itself into the membrane, forming an ion channel similar to that observed in cytotoxic lymphocytes (TSCHOPP & NABHOLZ, 1990). This event is initiated by intimate contact between the parasite and the target cell which is established mainly through a lectin-like molecule (PETRI et al., 1987). In a few minutes, important changes can be noticed in the target cell, such as swelling and surface alterations which finally cause the membrane to lose its functions and the cell to die. The pore-producing factor is known as amebapore. Isoforms have been reported which constitute a family with a similar sequence to that of a polypeptide found in NK and cytotoxic T cells. Other candidates have been reported as mediators of cytolysis (RAVDIN, 1989), whose biological and functional significance is currently under study. Amebic granules contain a battery 01 aggressive components such as hydroly- Immune evasion mechanisms by protozoa tic enzymes, among them an A2 acidic phospholipase with a phospholipase hydrolyzing activity on artificial membranes which is augmented in the presence of amebapore (LEIPPE, 1997). Additionally, potent cysteine proteases have been found whose secretion may contribute to the damage of host cells and tissues. In fact, it has been observed that before intestinal invasion, these cysteine proteases degrade the extracellular matrix and host mucoproteins, dislodge the epithelial cells and degrade the basal epithelial membrane; besides, they can interfere with the immune response by degrading IgA and IgG. They also activate the alternative complement pathway and elude the inflammatory response by inactivating C3a and C5a (QUE & REED, 1997). When the ameba is exposed to seric complement alone or in the presence of specific antibodies, it is destroyed by the activation of the alternative and of the classic antibody-dependent pathways. The activation exerted by the ameba on the alternative complement pathway has been known for a few years (ORTIZ-ORTIZet al., 1978). However, the sensibility of the ameba to this activation is still being discussed. Thus, while some authors prove its sensibility (HAMELMANNet al., 1993), others disprove it (REED, SARGEAUNT& BRAUD, 1983; REED et al., 1986). Recently, in a study performed on 21 patients from which E. histolytica was isolated and its presence characterized by the techniques of polymerase chain reaction and hexokinase isoenzyme typing, it was found that 90% of trophozoites were lysed by the alternative complement pathway after 30 min in the presence of human serum, regardless of whether it came from symptomatic or asymptomatic subjects (W ALDERICH,WEBER & KNOBLOCH, 1997). However, the ameba somehow escapes the lytic complement effect when it invades the host's tissues (CALDERON& Tov AR, 1986; MOGYOROS,CALEF & GITLER, 1986; HAMELMANNet al., 1993). It has not been discarded that the ameba may acquire resistance to this humoral factor in vivo and that it is sensitive to the effects of the alternative pathway only during the phase within the intestine; when the ameba colonizes the intestinal epithelium it does not need to be protected from the complement effects. On the other hand, when it invades the host and is exposed to the complement effects it needs to be protected and that is when it adapts to the presence of the seric factor (W ALDERICH,WEBER & KNOBLOCH, 1997). It has been proposed that the main mechanism of resistance of E. histolytica to lysis by complement may be through the acquisition of regulating molecules (GUTIERREZ-KoBEH, CABRERA & PEREZMONTFORT,1997), as the human erythrocyte restriction factor is incorporated to the membranes of sheep erythrocytes, protecting them from reactive lysis by C5b-9 (ZALMAN,WOOD & MULLER-EBERHARD,1987). On the other hand, the antibody also activates the complement when it combines with the ameba and in doing so, it destroys the trophozoite. Here, once more, the ameba evades the effect of the antibody through a mechanism which allows it to polarize the antibodies depo- 75 sited on the surface towards the uroid region where they are spontaneously eliminated by the ameba as supramolecular aggregates or caps, membrane compounds, without causing the parasite any harm. It is possible that the polarization of surface antigens interferes, avoiding the lytic effect mediated by the complement (CALDERON& AVILA,1986). Tissue invasion by the ameba has been associated with suppression of the cell-mediated response, which can facilitate its extra-intestinal survival and the production of the hepatic abscess. Most studies suggest that cell-mediated immunity is the most viable deposit of acquired protective immunity (ORTIZ-ORTIZ, 1994). The arguments that support this are: the cellular anergy which accompanies the initial invasion by E. histolytica (ORTIZ-ORTIZet al., 1975); the elevated incidence of invasive amebiasis in animals or humans who have received treatments which suppress T cells or splenectomy (GHADTRIAN& MEEROVTTCH,1981a, b; TRTSSL,1982); the protective effect of T cell stimulants (GHADTRIAN, MEEROVITCH& HARTMANN,1980); the appearance and persistence of delayed-type hypersensitivity (DTH) to amebic antigens after recovery from amebic liver abscess (KRETSCHMERet al., 1972; ORTIZ-ORTIZ et al., 1973a, b); the adoptive transfer of immunity by sensitized T lymphocytes and the amebolytic effect of cytotoxic T lymphocytes stimulated with antigen and activated macrophages (ORTIZ-ORTIZ, 1994). The parasite seems to exert different modulatory effects on macrophages and T cells, which surely allow its survival within the host. In a model of intestinal amebiasis in mice it has been found that infection induces a cyclic depression of DNA synthesis when spleen cells are stimulated with T or B lymphocyte mitogens or with antigen. In the supernatant of these cells stimulated with concanavalin A (Con A), a similar response is observed in the production of interleukin (IL)-2. This effect is eluded when spleen cells are treated with phorbol myristate acetate and ionomycin, indicating a defect at the level of the transduction signal. These cell alterations may facilitate the invasion of the host by the protozoan (GHOSH, CASTELLANOS-BARBA & ORTIZ-ORTIZ,1995). In support of the role of cellular immunity in amebiasis it has been reported that human macrophages stimulated in vitro with IFN-)' present an amebicidal effect which is dependent on contact. IFN-)' with lipopolysaccharide (LPS), tumor necrosis factor (TNF)-a and colony stimulating factor 1, present potent amebicidal activity which seems to involve oxidative and non-oxidative mechanisms (CAMPBELL& CHADEE, 1997). The requirement for macrophage activation suggests that the response of a Th l-type T -cell secreting IFN-)', IL-2 and TNF-I3, would be necessary for effective immunity against amebae. The cytotoxic capacity of macrophages is reduced during the acute phase of hepatic amebiasis. In a study performed with an experimental model of hepatic abscesses in the hamster, we found that the capacity of the mono- 76 nuclear phagocytic system of animals infected with amebae to eliminate an intracellular microorganism, specifically Candida albicans, was significantly altered. Evidently, this alteration very likely favors the survival of trophozoites in the liver (CAPIN, GONZALEZ-MENDOZA & ORTIZ-ORTIZ, 1980). It has been suggested that suppression of macrophage activity during amebiasis is mainly a local event mediated by direct exposure to the ameba and its products (DENIS & CHADEE, 1988). These events can influence the presentation of the antigen by the macrophage to T cells, thus diminishing cell-mediated immunity and cytokine secretion, some of which are necessary to activate the macrophage. In this sense, it has been reported that treatment of mouse macrophages with amebic antigens reduces in vitro the expression of la molecules induced by IFN-')' (DENIS & CHADEE, 1988; WANG & CHADEE, 1995). This effect has been partially considered to be due to prostaglandin E2 (PGE2), since it is blocked by cyclooxygenase inhibitors (indomethacin) which revert the amebic suppressor effect of la in the macrophage. In this sense, it has been reported that PGE2 may be produced by the ameba (BELLEY & CHAOEE, 1995) and may also elevate cAMP levels, triggering the phosphokinase A (PKA) pathway which inhibits the expression of la molecules of the macrophage surface (FIGUEREIDO,1990). Furthermore, the ameba also elevates the levels of cAMP in human macrophages through a monocyte locomotion inhibitory factor (RIco et al., 1995). The role of cytokines produced during amebic infection has been studied and TNF-a plays a relevant role. If increased it promotes macrophage amebecidal activity, while reduced levels may favor the development of amebic granulomas. Amebic stimulation of macrophage PGE2 production participates in suppressing TNF-a production (CAMPBELL& CHAOEE, 1997). Spleen cells from mice inoculated with a surface protein of 220 kDa have been found not to proliferate in vitro when stimulated by this protein, although they do induce IL-4 and IL-lO secretion (TALAMAS-RoHANAet al., 1995). Moreover, during the initial phases of experimental hepatic abscesses in gerbils, IL-4 is produced (CAMPBELL& CHADEE, 1997). These cytokines may suppress macrophage function, while the 220 kDa protein suppresses T-cell mitogenesis. Likewise, in addition to the production of Th2 cytokines, amebic infection is associated with suppression of IFN-')', a cytokine produced by Th I, which activates macrophages (SALATA et al., 1990). All these factors may participate in suppressing cellmediated immunity during the amebic hepatic abscess. PGE2 production during invasive amebiasis may regulate T cells since it inhibits their proliferation (BELLEY& CHADEE,1995) and the production of the Th 1 cytokines, IL-2 and IFN-')' (BETZ & FOX, 1991). It may be said that during amebic invasion, the parasite manipulates the functions of T cells and macrophages with the purpose of increasing the survival of the parasite within the liver S. ZAMBRANO-VILLA, D.M. ROSALES-BORJAS & L. ORTIZ-ORTIZ granuloma. Furthermore, amebas are capable of downregulating the expression of la molecules in the macrophage, possibly inhibiting their antigen-presenting cell activity and the activation of T cells. GIARDIASIS Giardia lamblia is one of the most common enteropathogenic protozoa. Infection with this parasite may cause acute or chronic diarrhea, characterized by intestinal malabsorption, and in children with chronic disease it may be associated to retardation in growth and development. However, the clinical spectrum may be very diverse, from the asymptomatic carrier to persistent diarrhea with malabsorption (WOLFE, 1984). In spite of extensive investigation in animal models and during human infection, little is known about the immunologic factors which determine the elimination of the acute disease and the development of protective immunity. The Giardia trophozoite colonizes the proximal small intestine and is responsible for diarrhea and malabsorption, while the cyst is the form of transmission since it is capable of leaving the host and surviving in an adequate environment (FARTHING,1994). Patients with the symptomatic disease present anti-Giardia antibodies of the classes IgM, IgG and IgA. Since trophozoites do not appear to invade tissues, the mucous surfaces remain stimulated by Giardia antigens during the entire life-span of the parasite. In this case, immunity to Giardia is closely associated to the type of immune response generated by the mucous-associated lymphoid tissue (FAUBERT, 1996). In this respect, evidence to date suggests that slgA in the intestinal lumen is likely to be involved in parasite clearance (FARTHING,1989). A protective effect of anti-trophozoite antibodies might result from inhibition of trophozoite attachment to intestinal epithelial cells (INGE, EOSON & FARTHING, 1988), as occurs in amebiasis (CARREROet al., 1994) or from opsonization of trophozoites for phagocytosis (KAPLAN& ALTMANSHOFER,1985). However, clearance of murine infection is also T-cell dependent (PETRO et al., 1992). Epidemiological evidence suggests that the presence of slgA antibodies may contribute to the protection against giardiasis in infants fed with maternal milk (ANDREWS & HEwLETT,1981). Invasion of the intestinal epithelium by the parasite is a rare event although diverse mechanisms are found in the mucosa to prevent it, for example, cytotoxic intraepithelial Iymphocytes, antibody mediated cytotoxicity (ADCC) and the complement system (DEGUCHI et al., 1987). The role of cellular immunity seems to be relevant in the infections caused by this flagellated protozoan. Experimentally, nude mice (nu/nu) present a prolonged infection which can be eradicated by reconstitution with normal syngeneic Iymphocytes (ROBERTS-THOMSON& MITCHELL, 1978). CD4 cells seem to be important for the elimination of the parasite during 77 Immune evasion mechanisms by protozoa infection, since they may be involved in the switch of IgM to the production of IgA in B cells. Not much is known about the ability of Giardia to evade the host's resistance mechanisms. However, attention has been directed to a group of cysteine-rich surface proteins which exhibit antigenic variation in Giardia isolates. The phenomenon of antigenic variation has been well established and it occurs both in vitro and in vivo (ADAM et al., 1988; NASH et al., 1988, 1990; GOTTSTEINet al., 1990). The frequency of surface antigen modifications has been determined, and depending on the particular Giardia isolate, they occur in one out of every 6 to 13 generations. The biological significance of this antigenic variation remains unknown, although it was originally thought that it could constitute a mechanism of evasion of immunologic effectors of the host, as happens with saliva trypanosomes. Not more than one cyclic modification has been demonstrated for surface antigens in the human infection and in other animals. However, it has recently been shown that Giardia isolates possess unique anti genic variants which differ in susceptibility to digestive proteases of the host, trypsin and a-chymotrypsin; thus, certain surface antigens seem to protect the parasite from enzymatic attack (NASH, MERRITT& CONRAD, 1991). TOXOPLASMOSIS Toxoplasmosis is caused by Toxoplasma gondii, an obligatory intracellular parasite of world-wide distribution which causes infection in most mammals. In man, seroprevalence is very high although the disease is rare (GARCIA& BRUCKNER,1993). After infection, the parasite remains inactive indefinitely in the central nervous system and other host tissues. The human infection is usually mild or asymptomatic, although in immunologically compromised patients the disease can be lethal (LEVY, BREDESEN & ROSENBLUM, 1985). The tachyzoite is very prolific; it infects almost all nucleated cells and generates the formation of parasitophorous vacuoles which do not fuse with intracellular organelles, thus preventing their destruction (MAUEL, 1996). The tachyzoite divides by binary fusion, forming an intracellular pseudocyst which distorts the host cell and finally destroys it. The tachyzoites liberated in this process invade adjacent cells. One important characteristic of this protozoan is that it induces a potent immune response in the host which is absolutely necessary for the host's survival and, therefore, for parasite survival, as it limits its multiplication and dissemination. The rise in host immunity is associated to the parasite's transformation to a latent state, thus escaping elimination by forming inactive cystic structures (DARCY & SANTORO,1994). The host controls the parasite mainly through IFN-l' from T and NK cells. Infection is characterized by a response with a characteristic pattern of cytokines from Th type 1 cells (Thl), i.e., cytokines which produce a strong cellular immunity (elevated IFN-l'/ decreased IL-4) (SHER & COFFMAN,1992). T. gondii seems to possess a superantigen which stimulates non-immune T cells to produce IFN-l'. It is likely that IL-12 and the superantigen induce a highly polarized response to Thl cells, characteristic of the T. gondii infection (DENKERS, 1996a). The superantigen is different from the peptidic antigens of T cells in that it binds to the external part of the class 11, lA and lE molecules of the MHC. Moreover, the interaction occurs regardless of the haplotype and with no requirement of intracellular processing. The combination of the superantigen and the class 11 molecules of the MHC interacts with the T cell receptor which expresses the variable 13 chain (VI3). Thus, numerous families of CD4+ and CD8+ T cells which express the appropriate VI3 chain are activated, instead of the clonotypic response which the conventional antigen activates (HERMAN,1991). During the early stages of infection, elevated levels of IFN-l' are required to control tachyzoite proliferation and the T. gondii superantigen may contribute to the production of IFN-l' by massive activation of T Vb5+ cells. Interestingly, in vitro studies indicate that the Vb5+ cell which expands is predominantly CD8+, a producer of IFN-l' (ROMAGNANI,1997). During chronic infection, tachyzoite replication is minimal and the requirement for IFN-l' decreases. The host may use down-regulatory mechanisms to evade the important immunogenicity of this parasite. The induction of V135 non-responsiveness may be an example of that mechanism (DENKERS,1996b). LEISHMANIASIS Approximately 12 million people are infected and 350 million at risk of being infected with leishmaniasis. Disease variations of this illness have been described (MoDABBER,1987). Leishmania is a protozoan which lives exclusively in mononuclear phagocytes. However, it lacks a specialized mechanism to penetrate cells and it therefore depends on the phagocytic potential of the host cell to be infected (MAUEL, 1996). When the host macrophage internalizes the Leishmania, the phagosome which arises rapidly fuses with the lysosomes forming a phagolysosome which contains cathepsins and dipeptidyl peptidases I and 11(PRINA et al., 1990). The Leishmania amastigotes seem to be adapted to life inside the acid medium of the phagolysosome, since they are metabolically more active in acid than in neutral pH. It is not known how this protozoan resists the degrading action of this and other enzymes. The phagolysosome appears to be the final site in which the parasite survives and multiplies. Two surface molecules of Leishmania have been implicated in the inhibition of the macrophage degrading processes: a gp63 surface protease (BORDIER,1987) and a lipophosphoglycan (LPG) (TuRCO & DESCOTEAUX, 1992). Nevertheless, the mechanisms used by these mo- 78 lecules remain largely unknown. Apparently, LPG protects the parasite from the lytic effect mediated by complement (PUENTESet al., 1990). Besides, during the initial stages of macrophage infection LPG promotes the intracellular survival of promastigotes. This molecule is liberated by promastigotes and is known as excreted factor, which possibly protects them against initial intralysosomal degradation (HANDMAN& GREENBLATT,1977). LPG also contributes to the infection potential of these protozoa by direct scavenging of oxygen intermediates or by an indirect effect on the respiratory burst through modulation of host cell signaling pathways. LPG belongs to a class of bacterial glycolipids which are quite effective at capturing hydroxyl radicals and superoxide anions, possibly due to their structure, formed by repeating oxidizable phosphorylated disaccharide units (MAUEL, 1996). L. donovani promastigotes, which do not contain much catalase, seem to be less resistant to damage mediated by oxidants, and to intracellular death, than amastigotes, which have a much larger amount of catalase and superoxide dismutase. Furthermore, Leishmania contains an antioxidant composed of two molecules of glutathione conjugated with spermidine, which have a similar function to glutathione in other cells (FAIRLAMB et al., 1985). Survival of Leishmania seems to depend on its capacity to avoid the respiratory burst of the host. Macrophage protein kinase C (PKC) activity is altered by intracellular Leishmania. The respiratory burst depression in human monocytes infected with L. donovani is accompanied by a decrease in protein phosphorylation, which correlates with a weak translocation of PKC to the membrane (OLIVIER,BROWNSEY& REINER, 1992). This suggests that Leishmania interferes with the transduction signal in macrophages, particularly with PKC-dependent pathways, where LPG (DESCOTEAUX& TURCO, 1993) and gp63 (SORENSEN,HEY & KHARAZMI, 1994) have been implicated. It is also necessary to mention that other mechanisms, beside these molecules, also contribute to parasite protection. In this sense, the parasite may promote its survival by preventing host cell death, which is accomplished by inhibiting apoptosis, possibly by stimulation of the granulocyte-macrophage colony stimulating factor (GMCSF), and production of TNF-a (MOORE & MATLASHEWSKI,1994). Other interesting effects which favor survival of this protozoan are: a notorius suppression of the expression of class I and 11 molecules of the MHC, through macrophage stimulation by IFN-')' (RElNER, NG & Mc MASTER, 1987); a release of PGE2 (RElNER & MALELMUD,1985) and transforming growth factor 13 (BARRALet al., 1993) which inhibit the immune response; downregulation of TNF-a receptor expression in LPG-treated macrophages (DESCOTEAUXet al., 1991) by inhibiting macrophage activation by TNF-a (CORRADIN,BUCHMULLER-RoUILLER & MAUEL, 1991); and inhibition of neutrophil and monocyte chemotaxis (FRANKENBURGet al., 1990). S. ZAMBRANO-V1LLA, D.M. ROSALES-BORJAS & L. ORTlZ-ORTlZ The role of Thlffh2 cells has been reported to be protective against infection with L. major. The capacity of specific T CD4+ cells to transfer the resistance or exacerbation of the disease to immunodeficient or sublethally irradiated naive hosts correlates with the production of cytokines derived from Thl or Th2 cells (SCOTT et al., 1988; HOLADAYet al., 1991). At the beginning of Leishmania infection in resistant (C57BL/6) or susceptible mice (BALB/c) a strong mixed response is observed in the CD4+ cell population, which consists in IL-2, IL-4 and IL-13, with a maximum on day 4. However, the resistant strain rapidly down regulates IL-4 transcription, while BALB/c mice continue to express IL-4 levels consistent with Th2. It has been observed that IL-4 gene knockout BALB/c mice, despite lacking IL-4, remain susceptible to infection with L. major. On the other hand, observations in resistant mice revealed that infected macrophages produce IL-12 and NK cells produce IFN-')', and both are responsible for the protective Thl response in this type of mice (ROMAGNANI,1997). The susceptible strain, however, could change its phenotype after administration of anti -IL-4 or IL-12 during the first weeks of infection (COFFMANet al., 1991; CHATELEIN, V ARKILA& COFFMAN, 1992; SYPEK et al., 1993). It is currently known that the only factors involved in the process of subset differentiation of CD4+ T cells in vivo are IL-4 and IFN-')'. However, this evidence derives from the study of some models of infectious diseases and it is not known how general the roles of these two cytokines are (COFFMANet al., 1991). Many questions still need to be answered with regard to the participation of the Thl and Th2 subunits in leishmaniasis. However, results obtained at present and their application to treatment of the disease in humans are promising. CONCLUSIONS The protozoa here reviewed possess mechanisms which allow them to evade the effect of the host immune response in various ways. Some protozoa do so by changes or mutations of surface proteins, others by mechanisms which somehow allow them to survive the effect of intracellular enzymes of the phagocytic cell, or else, of the noxious effect of the antibody or complement by a mechanism of «denuding» in which membrane and antibody are oriented towards one extreme of the cell and subsequently eliminated. Others possess the ability to inactivate or acquire resistance to the effects of complement. However, most seem to have an effect on the regulation of T lymphocytes and its cytokines, since an inappropriate response at this level may be of vital importance to the survival of the host, and therefore, of the parasite. REFERENCES ADAM(R.D.), AQGARWAL (A.), LAL(A.A.), DE LACRUZ(V.F.), MCCUTCHAN (T.) & NAsH(T.E.), 1988.- Antigenicvariationof Immune evasion mechanisms by protozoa protein in Giardia lamblia. Journal of Experimental Medicine, 167: 109-118. a cysteine-rich ALMEIDA (I.e.), FERGUSON (M.A.I.), SHENKMAN (S.) & l'RAVASsos (L.R.), 1994.- GPI-anchored glycoconjugates from Trypaare recognized by lytic anti-a-ganosoma cruri trypomastigotes lactosyl antibodies from patients with chronic Chagas' disease. Brazilian Journal of Medical and Biological Research, 27: 443447. ANDREWS (1.S.) & HEWLETI (E.L.), 1981.- Protection against infection with Giardia muris by milk containing antibody to Giardia. Journal of Infectious Diseases, 143: 242-246. ASKONAS (B.A.), CORSlNI (A.e.), CLAYTON (C.E.) & OGrLVIE (B.M.), 1979.- Functional depletion of T- and B-memory cells and other lymphoid cell subpopulations during trypanosomiasis. Immunology, 36: 313-321. BARKER (L.R.), 1971.- Experimental malaria: effects upon the immune response to different antigens. Journal of Infectious Diseases, 123: 99-10 1. BARRAL (A.), BARRAL-NETTO (M.), YOUNG (E.e.), BROWNELL (e.E.), TwARDZIK (D.R.) & REED (S.G.), 1993.- Transforming growth factor-b as a virulence mechanism for Leishmania brazi- liensis. Proceedings of the National Academy of Sciences USA, 90: 3442-3446. BELLEY (A.) & CHADEE (K.), 1995.- Eicosanoid production by paParasitology rasites: from pathogenesis to immunomodulation? Today, 11: 327-334. BETZ (M.) & Fox (B.S.), 1991.- Prostaglandin E2 inhibits production of Thl Iymphokines but not of Th2 Iymphokines. Journal of Immunology, 146: 108-113. BORDlER (C.), 1987.- The promastigote surface proteases of Leishmania. Parasitology Today, 3: 151-156. BORST (P.) & CROSS (G.A.M.), 1982.- Molecular basis for Trypanosoma antigenic variation. Cell, 29: 291-303. BRENER (Z.), 1980.- Immunity to Trypanosoma cruzi. Advances in Parasitology, 18: 247-292. CABALLERO-SALCEDO (A.), VIVEROS-ROGEL (M.), SALVATIERRA (B.), TAPIA-CONYER (R.), SEPULVEDA-AMoR (1.), GUTIERREZ (G.) & ORTlZ-ORTlZ (L), 1994.- Seroepidemiology of amebiasis in Mexico. American Journal of Tropical Medicine and Hygiene, 50: 412-419. caps in CALDERON (J.) & AVILA (E.E.), 1986.- Antibody-induced Entamoeba histolytica: isolation and electrophoretic analysis. Journal of Infectious Diseases, 153: 927-932. CALDERON (J.) & TOVAR (R.), 1986.- Loss of susceptibility to complement lysis in Entamoeba histolytica HMI by treatment with human serum. Immunology, 58: 467-471. CAMPBELL (D.) & CHADEE (K.), 1997.- Survival strategies of Entamoeba histolytica: modulation of cell-mediated immune responses. Parasitology Today, 13: 184-190. CAPIN (R.), GONZALEZ-MENDOZA (A.) & ORTIZ-ORTIZ (L.), 1980.Disminuci6n de la actividad del sistema facogftico mononuclear en hamsters infectados con Entamoeba histolytica. Archivos de la lnvestigacion Medica (Mexico), 11: 235-240. CARRERO (I.e.), DlAZ (M.Y.), VIVEROS (M.), ESPlNOZA (B.), ACOSTA (E.) & ORTlZ-ORTlZ (L.), 1994.- Human secretory immunoglobulin A anti-Entamoeba histolytica antibodies inhibit adherence of amebae to MOCK cells. Infection and Immunity, 62: 764-767. CHAROENVIT (Y.), CAMPBELL (G.H.) & TOKUDA (S.), 1981.- Suppression of parasite antigen-specific lymphoid blastogenesis in Journal of Immunology, 127: 2350African trypanosomiasis. 2354. CHATELElN (R.), VARKILA (K.) & COFFMAN (R.L.), 1992.- IL-4 induces a Th2 response to Leishmania major-infected mice. Journal of Immunology, 148: 1182-1187. CHERESH (D.A.), HAYNES (H.) & DISTASIO (I.A.), 1984.- Interaction of an acute phase reactant, alpha-acid glycoprotein (oros- 79 mucoid), with the lymphoid cell surface. A model for nonspecific immune suppression. Immunology, 51: 541-548. CHRlSTOPHERS (S.R.), 1924.- The mechanism of immunity against malaria in communities living under hyper-endemic conditions. Indian Journal of Medical Research, 12: 273-294. CUNTON (B.A.), STAUBER (L.A.) & PALCZUK (N.C.), 1969.Leishmania donovani: antibody response to chicken ovalbumin by infected golden hamsters. Experimental Parasitology, 25: 171-180. CUNTON (B.A.), ORTlZ-ORTlZ (L.), GARClA (W.), MARTlNEZ (T.) & CAPlN (R.), 1975.- Trypanosoma cruzl: early immune responses in infected mice. Experimental Parasitology, 37: 417-425. COFFMAN (R.L.), CHATELAlN (R.), LEAL (L.M.e.C.) & V ARKILA (K.), 1991.- Leishmania major infection in mice: a model sysResetem for the study of CD4+ T-cell subset differentiation. arch in Immunology, 142: 36-40. CORRADlN (S.B.), BUCHMULLER-RoUILLER (Y.) & MAUEL (l), 1991.- Phagocytosis enhances murine macrophage activation by interferon-g and tumor necrosis factor-a. European Journal of Immunology, 21: 2553-2558. Cox (F.E.G.), BILBEY (D.L.1.) & NICOL (T.), 1964.- Reticulo-endothelial activity in mice infected with Plasmodium vinckei. Journal of Protozoology, 11: 229-236. DARCY (F.) & SANTORO (F.), 1994.- Toxoplasmosis. In: Parasitic Infections and the Immune System (F. Kierszenbaum edit.), Academic Press, New York: 163-20 I. DA Y (K.) & MARSH (K.), 1991.- Naturally acquired immunity to Plasmodium falciparum. Parasitology Today, 7: 68-71. DEGUCHI (M.), GlLLlN (F.D.) & GIGU (I.), 1987.- Mechanisms of killing of Giardia Lamblia trophozoites by complement. Journal of Clinical Investigation, 79: 1296-1302. DENIS (M.) & CHADEE (K.), 1988.-ln vitro and in vivo studies of macrophage function in amebiasis. Infection and Immunity, 56: 3126-3131. DENKERS (E.Y.), 1996a.- A Toxoplasma gondii superantigen: biological effects and implications for the host-parasite interaction. Parasitology Today, 12: 362-366. DENKERS (E. Y.), 1996b.- Toxoplasma gondii induces specific nonresponsiveness in Iymphocytes bearing the Vj35 chain of the mouse T cell receptor. Journal of Immunology, 156: 10891094. DESCOTEAUX (A.) & TURCO (S.1.), 1993.- The lipophosphoglycan of Leishmania and macrophage protein kinase C. Parasitology Today, 9: 468-471. DESCOTEAUX (A.), TuRCO (S.J.), SACKS (D.L.) & MATLASHEWSKI selecti(G.), 1991.- Leishmania donovani lipophosphoglycan vely inhibits signal transduction in macrophages. Journal of Immunology, 146: 2747-2753. DIFFLEY (P.), 1983.- Trypanosomal surface coat variant antigen causes polyclonal Iymphocyte activation. Journal of Immunology, 131: 1983-1986. FAIRLAMB (A. H.), BLACKBURN (P.), ULRlCH (P.), CHAlT (B.T.) & CERAMI (A), 1985.- Trypanothione: a novel bis(glutathionyl)spermidine cofactor for glutathione reductase in trypanosomatids. Science, 227: 1485-1487. FARTHING (MJ.G.), 1989.- Host-parasite interactions in human giardiasis. Quarterly Journal of Medicine, 70: 191-204. FARTHING (M.J.G.), 1994.- Giardiasis as a disease. In: Giardia: From Molecules to Disease (R.e.A. Thompson, J.A. Reynoldson & AJ. Lymbery edit.), Cab International, London: 15-37. FAUBERT (G.M.), 1996.- The immune response to Giardia. Parasitology Today, 12: 140-145. FIGUElREDO (F.) , 1990.- Activation of the cAMP cascade inhibits an early event involved in murine macrophage la expression. Journal of Biological Chemistry, 265: 12317-12323. FiSHER (E.), OUAlSSI (M.A.), VELVE (P.), CORNETTE (1.) & KAZATCHKINE(M.D.), 1988.- gp 58/68, a parasite component that 80 contributes to the escape of the trypomastigote form of T. cruri from damage by the human alternative complement pathway. Immunology, 65: 299-303. FRANKENBURG(S.), LElBOVICI (V.), MANSBACH (N.), TURCO (S.1.) & ROSEN (G.), 1990.- Effect of glycolipids of Leishmania parasites on human monocyte activity. Inhibition by lipophosphoglycan. Journal of Immunology, 145: 4284-4289. GARCIA (L.S.) & BRUCKNER (D.A.), edit., 1993.- Diagnostic Medical Parasitology. American Society for Microbiology, Washington, D.C.: 92-112. GARCIA (I.E.), D'IMPERlO (M.R.L.), MARlNHO (C.R.F.), KIPNIS (T.L.), FURTADO (G.c.) & ALVAREZ (J.M.), 1997.- Role of membrane-bound IgM in Trypanosoma cruri evasion from immune clearance. Journal of Parasitology, 83: 230-233. GASBARRE (L.C.), HUG (K.) & LOUIS (J.), 1981.- Murine T Iymphocyte specificity for African trypanosomes. H. Suppression of the T Iymphocyte proliferative response to Trypanosoma brucei by systemic trypanosome infection. Clinical and Experimental Immunology, 45: 165-172. GHADIRIAN (E.) & MEEROVITCH (E.), 1981 a.- Effect of splenectomy on the size of the amoebic liver abscess and metastatic foci in hamsters. Infection and Immunity, 31: 571-573. GHADIRIAN (E.) & MEEROVITCH (E.), 1981b.- Effect of immunosuppression on the size and metastasis of amoebic liver abscess in hamsters. Parasite Immunology, 3: 329-338. GHADIRIAN (E.), MEEROVITCH (E.) & HARTMANN (D.F.), 1980.Protection against amebic liver abscess in hamsters by means of immunization with amebic antigen and some of its fractions. American Journal of Tropical Medicine and Hygiene, 29: 779-784. GHOSH (P.K.), CAsTELLANos-BARBA (C.) & ORTIZ-ORTIZ (L.), 1995.- Intestinal amebiasis: cyclic suppression of the immune response. Parasitology Research, 81: 475-480. GODFREy-FAUSSETT (P.), WRlGHT (S.G.), McDoNALD (V.), NINA (1.), CHIODINI (P.L) & McADAM (K.P.M.1.), 1993.- Parasites in the immunocompromised host. In: Immunology and Molecular Biology of Parasitic Infections (K.S. Warren edit.), Blackwell, London: 100-125. GOODWIN (L.G.), GREEN (D.G.), GUY (M.W.) & VOLLER (A.), 1972.- Immunosuppression during African trypanosomiasis. British Journal of Experimental Pathology, 53: 40-43. GOTTSTElN(B.), HARRIMAN (G.R.), CONRAD (G.T.) & NAsH (T.E.), 1990.- Antigenic variation in Giardia lamblia: cellular and humoral immune response in a mouse model. Parasite Immunology, 12: 659-673. GRAY (A.R.) & LUCKlNS (A.G.), 1976.- Antigenic variation in salivarian trypanosomes. In: Biology of the Kinetoplastida (W.H.R Lumsden & D.A. Evans edit.), Academic Press, London, Vol. 1: 493-452. GREENWOOD(B.M.), PLAYFAIR(J.H.L.) & TORRIGIANI(G.), 1971.Immunosuppression in murine malaria. I. General characteristics. Clinical and Experimental Immunology, 8: 467-478. GREENWOOD(B.M.), ODULOJU (AAJ.) & STRATTON (D.), 1977.Lymphocyte changes in acute malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene, 71: 408-410. GUTIERREZ-KoBEH (L.), CABRERA (N.) & PEREZ-MoNTFORT (R.), 1997.- A mechanism of acquired resistance to complement-mediated lysis by Entamoeba histolytica. Journal of Parasitology, 83: 234-241. HALL (R.), 1994.- Molecular mimicry. Advances in Parasitology, 34: 81-132. HAMELMANN(C.), FOERSTER (B.), BURCHARD (G.D.), SHETTY (N.) & HORSTMANN (R.D.), 1993.- Induction of complement resistance in cloned pathogenic Entamoeba histolytica. Parasite Immunology, 15: 223-228. HANDMAN (E.) & GREENBLATT (C.L.), 1977.- Promotion of leishmanial infection in non-permissive host-macrophages by con- S. ZAMBRANO- VILLA, D.M. ROSALES-BORJAS & L. ORTIZ-ORTIZ ditioned medium. Zeitschriftfiir Parasitenkunde, 53: 143-147. HAREL-BELLAN (A.), JOSKOWICZ (M.), FRADELlZI (D.) & EISEN (H.), 1983.- Modification of T-cell proliferation and interleukin 2 production in mice infected with Trypanosoma cruzi. Proceedings of the National Academy of Sciences USA, 80: 3466-3469. HAREL-BELLAN (A.), JOSKOWICZ (M.), FRADELlZI (D.) & ElsEN (H.), 1985.- T Iymphocyte function during experimental Chagas' disease: production of and response to interleukin 2. European Journal of Immunology, 15: 438-442. HERMAN (A.), 1991.- Superantigens: mechanisms ofT-cell stimulation and role in immune responses. Annual Review of Immunology, 9: 745-772. HIGUCHI (M.L.), MARTINS (M.R.), DEMARCHI (V.A.), BENVENUTI (L.A.), SAMPAIO (P.G.), BELLOTTI (G.) & PlLEGGI (F.), 1997.Association of an increase in CD8+ cells with the presence of Trypanosoma cruzi antigens in chronic, human, chagasic myocarditis. American Journal of Tropical Medicine and Hygiene, 56: 485-489. Ho (M.), WEBSTER (H.K.), LOOAREESUWAN(S.), SUPANARANOND (W.), PHlLLlPS (R.E.), CHANTHAVANICH (P.) & WARREOO (D.A.), 1986.- Antigen-specific immunosuppression in human malaria due to Plasmodium falciparum. Journal of Infectious Diseases, 153: 763-771. HOLADAY (BJ.), SADICK (M.D.), WANG (Z.-E.), REINER (S.L.), HEINZEL (F.P.), PARSLOW (T.G.) & LOCKSLEY (R.M.), 1991.Reconstitution of Leishmania immunity in severe combined immunodeficient mice using Thl- and Th2-like cell lines. Journal of Immunology, 147: 1653-1658. HOUBA (V.), BROWN (K.N.) & ALLlsON (A.C.), 1969.- Heterophile antibodies. M-antiglobulins and immunoglobulins in experimental trypanosomiasis. Clinical and Experimental Immunology,4: 113-119. HUDSON (K.M.), BYNER (C.), FREEMAN (J.) & TERRY (RJ.), 1976.- Immunodepression, high IgM levels and evasion of the Nature (London), immune response in murine trypanosomiasis. 264: 256-258. INGE (P.M.G.), EDSON (C.M.) & FARTHING (MJ.G.), 1988.- Attachment of Giardia lamblia to rat intestinal epithelial cells. Gut, 29: 795-801. JAYAWARDENA (A.N.) & WAKSMAN (B.H.), 1977.- Suppressor Nature (London), 265: cells in experimental trypanosomiasis. 539-541. JOINER (K.A.), DA SILVA (W.D.), RIMOLDI (M.T.), HAMMER (C.H.), SHER (A.) & KIPNIS (T.L.), 1988.- Biochemical characterization of a factor produced by trypomastigotes of T. cruzi which accelerates the decay of complement C3 convertases. Journal of Biological Chemistry, 263: 11327-11335. KAPLAN (B.) & ALTMANSHOFER(D.), 1985.- Giardia muris adherence to intestinal epithelium: the role of specific anti-Giardia antibodies. Microecological Therapy, 15: 133-140. KIERSZENBAUM (F.), SZTEIN (M.B.) & BELTZ (L.A.), 1989.- Decreased human IL-2 receptor expression due to a protozoan pathogen. Immunology Today, 10: 129-131. KRETSCHMER (R.R), SEPULVEDA (B.), ALMAZAN (A.) & GAMBOA (F.), 1972.- Intradermal reactions to an antigen (histolyticin) obtained from axenically cultivated E. histolytica. Tropical and Geographical Medicine, 24: 275-281. KUBY (J.), 1997.- Immunology. W.H. Freeman, New York: 474476. KWIATKOWSKI (D.), 1991.- Cytokines and anti-disease immunity to malaria. Research in Immunology, 142: 611-738. LAURENT (M.), PAYS (E.), MAGNUS (E.), MEIRVENNE (V.), MATTHYSSENS (G.), WILLlAMS (RO.) & STEINERT (M.), 1983.DNA rearrangements linked to expression of a predominant surface antigen gene of trypanosomes. Nature (London), 302: 263-266. . Immune evasion mechanisms by protozoa LEIPPE (M.), 1997.- Amoebapores. Parasitology Today, 13: 178183. LELCHUK (R.), SPROTI (V.M.A.) & PLAYFAIR (J.H.L.), 1981.- Differential involvement of nonspecific suppressor T cells in two lethal murine malaria infections. Clinical and Experimental Immunology, 45: 433-438. LEVY (R.M.), BREDESEN (D.E.) & ROSENBLUM (M.L.), 1985.Neurological manifestations of the acquired immunodeficiency syndrome (AIDS): experience at UCSF and review of the literature. Journal of Neurosurgery, 62: 475-495. MATIHYSSENS (G.), MICHIELS (F.), HAMERS (R.), PAYS (E.) & STEINERT (M.), 1981.- Two variant surface glycoproteins of Trypanosoma brucei have a conserved C-terminus. Nature (London), 293: 230-233. MAUEL (J.), 1996.- Intracellular survival of protozoan parasites with special reference to Leishmania spp., Toxoplasma gondii and Trypanosoma cruzi. Advances in Parasitology, 38: 1-51. and humoral imMAuEL (J.) & BEHIN (R.), 1974.- Cell-mediated munity to protozoan infections. Transplantation Reviews, 19: 121-146. MCCUTCHAN (T.F.), DE LA CRUZ (V.F.), GOOD (M.F.) & WELLEMS (T.E.), 1988.- Antigenic diversity in Plasmodium falciparum. Progress in Allergy, 41: 173-192. MERINO (F.), LAYRlSSE (Z.), GODOY (G.) & VOLCAN (G.), 1986.Immunoregulatory alterations in Plasmodium falciparum and Plasmodium vivax infections. Tropical Medicine and Parasitology, 37: 241-244. Mo DABBER (F.), 1987.- The leishmaniases. In: Tropical Disease Research, a Global Partnership, Eight Programme Report, TDR (J. Maurice & A.M. Pearce, edit.), World Health Organization, Geneva: 99-112. MOGYOROS (M.), CALEF (E.) & GITLER (C.), 1986.- Virulence of Entamoeba histolytica correlates with the capacity to develop complement resistance. Israel Journal of Medical Science, 22: 915-917. MOORE (KJ.) & MATLASHEWSKI (G.), 1994.- Intracellular infecapoptosis. tion by Leishmania donovani inhibits macrophage Journal of Immunology, 152: 2930-2937. MORAKOTE (N.) & JUSTUS (D.E.), 1988. Immunosuppression in malaria: effect of hemozoin produced by Plasmodium berghei. International Archives of Allergy and Applied Immunology, 86: 28-34. MURRAY (P.K.), JENNINGS (F.w.), MURRAY (M.) & URQUHART (G.M.), 1974.- The nature of immunosuppression in Trypanosoma brucei infections in mice. H. The role of the T and B Iymphocytes. Immunology, 27: 825-840. MYLER (P.), NELsoN (R.G.), AGABIAN (N.) & STUART (K.), 1984.Two mechanisms of expression of a predominant variant antigen gene of Trypanosoma brucei. Nature (London), 309: 282-284. NAsH (T.E.), AGGARWAL (A.), ADAM (R.D.), CONRAD (J.T.) & MERRlTI (J.W. JR.), 1988.- Antigenic variation in Giardia lamblia. Journal of Immunology, 141: 636-641. NASH (T.E.), HERRlNGTON (D. A.), LEVINE (M.M.), CONRAD (J.T.) & MERRlTI (J.WJr.), 1990.- Antigenic variation of Giardia lamblia in experimental human infections. Journal of Immunology, 144: 4362-4369. NASH (T.E.), MERRlTI (J.wJr.) & CONRAD (J.T.), 1991.- Isolate and epitope variability in susceptibility of Giardia lamblia to intestinal proteases. Infection and Immunity, 59: 1334-1340. NORRls (K.A.), HARTH (G.) & So (M.), 1989.- Purification of a Trypanosoma cruzi membrane protein which elicits lytic antibodies. Infection and Immunity, 57: 2372-2377. OUVIER (M.), BROWNSEY (R.W.) & REINER (N.E.), 1992.- Defective stimulus-response coupling in humans monocytes infected with Leishmania donovani is associated with altered activation and translocation of protein kinase C. Proceedings of the National Academy of Sciences USA, 89: 7481-7485. 81 ORTtz-ORTIZ (L.), 1994.- Amebiasis. In: Parasitic Infections and edit.), Academic Press, the Immune System (F. Kierszenbaum New York: 145-162. ORTtz-ORTIZ (L.), GARMlLLA (C.), T ANIMOTO-WEKI (M.) & ZAMACONA (G.R.), 1973a.- Hipersensibilidad celular en amibiasis: I. Reacciones en hamsters inoculados con E. histolytica. Archivos de Investigaci6n Medica (Mexico), 4: 141-146. ORT1Z-ORTIZ (L.), GARMILLA (C.), ZAMACONA (G.R.) & SEPULVEDA (B.), 1973b.- Hipersensibilidad celular en amibiasis: 11. Estudio en pacientes con absceso hepatico amibiano agudo. Archivos de Investigaci6n Medica (Mexico), 4: 191-196. ORTlZ-ORTlZ (L.), ZAMACONA (G.), SEPULVEDA (B.) & CAPIN (N.R.), 1975.- Cell-mediated immunity in patients with amebic abscess of the liver. Clinical Immunology and Immunopatho- logy,4: 127-134. ORTIZ-ORTIZ (L.), CAPlN (R.), CAPlN (N.R.), SEPULVEDA (B.) & ZAMACONA (G.), 1978.- Activation of the alternative pathway of complement by Entamoeba histolytica. Clinical and Experimental Immunology, 34: 10-18. ORTtz-ORTlZ (L.), PARKS (D.E.), RODRlGUEZ (M.) & WElGLE (W.O.), 1980.- Polyclonal B Iymphocyte activation during Trypanosoma cruzi infection. Journal of Immunology, 124: 121-126. ORTlZ-ORTIZ (L.), CAPIN (R.), CAPlN (N.R.), SEPULVEDA (B.) & ZAMACONA (G.), 1978.- Activation of the alternative pathway of complement by Entamoeba histolytica. Clinical and Experimental Immunology, 34: 10-18. PEARSON (T.W.), ROELANTS (G.E.), LUNDlN (L.B.) & MAYOR-WITHEY (K.S.), 1978.- Immune depression in trypanosome-infected mice. I. Depressed T Iymphocyte responses. European Journal of Immunology, 8:723-727. PEARSON(T.W.), ROELANTS (G.E.), PINDER (M.), LUNDIN (L.B.) & MAYOR-WITHEY (K.S.), 1979.- Immune depression in trypanosome-infected mice. Ill. Suppressor cells. European Journal of Immunology, 9: 200-204. PETRI (W.A.), SMITH (R.D.), SCHLESINGER(P.H.), MURPHY (C.F.) & RA VDIN (J .1.), 1987.- Isolation of the galactose-binding lectin that mediates the in vitro adherence of Entamoeba histolytica. Journal of Clinical Investigation, 80: 1238-1244. PETRO (T.M.), WATSON (R.R.), FEELY (D.E.) & DARBAN (H.), 1992.- Suppression of resistance to Giardia muris and cytokine production in a murine model of acquired immune deficiency syndrome. Regional Immunology, 4: 409-414. PRlNA (E.), ANTOINE (J.C.), W1EDERANDERS(B.) & KIRSCHKE(H.), 1990.- Localization and activity of various lysosomal proteases in Leishmania amazonensis-infected macrophages. Infection and Immunity, 58: 1730-1737. PUENTES (S.M.), DA SILVA (R.P.), SACKS (D.L.), HAMMER (C.H.) & JOINER (K.A.), 1990.- Serum resistance of metacyclic stage Leishmania major promastigotes is due to the release of C5b-9. Journal of Immunology, 145: 4311-4316. QUE (X.) & REED (S.L.), 1997.- The role of extracellular cysteine proteinases in pathogenesis of Entamoeba histolytica invasion. Parasitology Today, 13: 190-194. RAMos (C.), LAMOYI (E.), FEOLl (M.), RODRIGUEZ (M.), PEREZ (M.) & ORTtz-ORTtz (L.), 1978.- Trypanosoma cruzi: Immunosuppressed response to different antigens induced in the infected mouse. Experimental Parasitology, 45: 190-199. RAvDlN (J.I.), 1989.- Entamoeba histolytica: from adherence to enteropathy. Journal of Infectious Diseases, 159: 420-429. REED (S.L.), SARGEAUNT (P.G.) & BRAUDE (A.I.), 1983.- Resistance to lysis by human serum of pathogenic Entamoeba his- tolytica. Transactions of the Royal Society of Tropical Medicine and Hygiene, 77: 248-253. REED (S.L.), CURD (J.G.), GIGLI (I.), GlLLIN (F.D.) & BRAUDE (A.I.), 1986.- Activation of complement by pathogenic and Entamoeba histolytica. Journal of Immunology, nonpathogenic 136: 2265-2270. S. ZAMBRANO- VILLA, D.M. ROSALES-BORJAS & L. ORTIZ-ORTIZ 82 REINER (N.E.) & MALELMUD (Cl.), 1985.- Arachidonic acid metabolism by murine peritoneal macrophages infected with Leishalteramania donovani: in vitro evidence for parasite-induced tions in cyclooxygenase and lipooxygenase pathways. Journal of Immunology, 134: 556-563. REINER (N.E.), NG (W.) & McMASTER (W.R.), 1987.- Parasite accessory cell interactions in murine leishmaniasis. II. Leishmania donovani suppresses macrophage expression of class I and class II major histocompatibility complex gene products. Journal of Immunology, 138: 1926-1932. REINITZ (D.M.) & MANSFIELD (1.M.), 1990.- T-cell-independent and Tvcell-dependent B-cell responses to exposed variant surface glycoprotein epitopes in trypanosome-infected mice. Infection and Immunity, 58: 2337-2342. RICE-FIGHT (A.C), CHEN (K.K.) & DONELSON (1.E.), 1981.- Sequence homologies near the C-termini of the variable surface glycoproteins of Trypanosoma brucei. Nature (London), 294: 53-57. RICO (G.), DIAz GUERRA (0.) & KRETSCHMER (R.R.), 1995.- Cyclic nucleotide changes induced in human leukocytes by a product of axenic ally grown Entamoeba histolytica that inhibits human monocyte locomotion. Parasitology Research, 81 : 158-162. RlLEY (E.M.), HVIID (L.) & THEANDER (T.G.), 1994.- Malaria. In: Parasitic Infections and the Immune System (F. Kierszenbaum edit.), Academic Press, San Diego: 119-143. RrLEY (E.M.), ANDERSSON (G.), OTOO (L.N.), lEPSEN (S.) & GREE WOOD (B.M.), 1988.- Cellular and humoral responses to Plasmodium falciparum antigens in Gambian children during and after an attack of acute falciparum malaria. Clinical and Ex- perimentallmmunology,73: 17-22. RJLEY (E.M.), JOBE (0.), BLACKMAN (M), WHITfLE (H.C) & GREE WOOD(B.M.), 1989a.- Plasmodiumfalciparuin schizont sonicates suppress the Iymphoproliferative response to rnitogens and antigens in malaria-immune adults. Infection and Immunity, 57: 3181-3188. RlLEY (E.M.), MAcLENNAN (C.), KWIATKOWSKI (D.) & GREENWOOD(B.M.), 1989b.- Suppression of in vitro lyrnphoproliferative responses in acute malaria patients can be partially reversed by indomethacin. Parasite Immunology, 11 : 509-517. ROBERTs-THOMSON (I.C) & MITCHEL (G.F.), 1978.- Giardiasis in mice. I. Prolonged infections in certain mouse strains and hypothymic (nude) mice. Gastroenterology, 75: 42-46. ROMAGNANI(S.), 1997.- Molecular Biology Intelligence Unit. The Thl/Th2 Paradigm in Disease. Springer, New York: 63-108. SACKS (DL) & ASKONAS (B.A.), 1980.- Trypanosome-induced suppression of antiparasite responses during experimental African trypanosomiasis. European Journal of Immunology, 10: 971-974. SALAMAN (M.H.), WEDDERBURN (N.) & BRUCE-CHWATT (L.l.), 1969.- The immunodepressive effect of a murine Plasmodium and its interaction with murine oncogenic virus. Journal of General Microbiology, 59: 383-391. SALATA (R.A.), MARTJNEZ-PALOMO (A.), CANALES (L.), MURRAY (H.W.), TREVINO (N) & RA VDlN (1.1.), 1990.- Suppression of TIymphocyte responses to Entamoeba histolytica antigen by immune serum. Infection and Immunity, 58: 3941-3946. SCHMuFns (G.A.), SZARFMAN (A.), COARASA (L.) & V AINSTOK (C), 1978.- Immunoglobulin concentration in treated human acute Chagas' disease. American Journal of Tropical Medicine and Hygiene, 27: 473-477. SCOTT (P.), NATOVITZ (P.), COFFMAN (R.L.), PEARCE (E.) & SHER (A.), 1988.- Immunoregulation of cutaneous leishmaniasis. T cell lines that transfer protective immunity or exacerbation belong to different T helper subsets and respond to distinct parasite antigens. Journal of Experimental Medicine, 168: 16751684. SHER (A.) & COFFMAN (R.L.), 1992.- Regulation of immunity to parasites by T cells and T cell-derived cytokines. Annual Review of Immunology, 10: 385-410. SHER (A.) & SCOTT (P.A.), 1993.- Mechanisms of acquired immunity against parasites. In: Immunology and Molecular Biology of Parasitic Infections (K.S. Warren, edit.), Blackwell, London: 35-51. SlLEGHEM, (M.), FLYNN (1.N.), DARJI (A.), BAETSELIER (P. DE) & NAESSENS (J.), 1994.- African trypanosomiasis. In: Parasitic Infections and the Immune System (F. Kierszenbaum edit.), Academic Press, New York: 1-51. SORENSEN (A.L.), HEY (A.S.) & KHARAZMI (A.), 1994.- Leishmania major surface protease Gp63 interferes with the function of human monocytes and neutrophils in vitro. Acta Pathologica, Microbiologica et Immunologica Scandinavica, 102: 265-27l. SROUR (E.), SEGRE (M.) & SEGRE (D.), 1988.- Impairment of T helper function by a Plasmodium berghei-derived immunosuppressive factor. Journal of Protozoology, 35: 441-446. SYPEK (J.P.), CHUNG (CL.), MAYOR (S.E.), SUBRAMANYAM(l.M.), GOLDMAN (S.1.), SrEBURTH (D.S.), WOLF (S.F.) & SCHAUB (R.G.), 1993.- Resolution of cutaneous leishmaniasis: interleukin 12 initiates a protective T helper type I immune response. Journal of Experimental Medicine, 177: 1797-1802. TALAMAs-RoHANA (P.), SCHLlE-GUZMAN (M.A.), HERNANDEz-RAMJRES (V.I.) & ROSALES-ENCINA (l.L.), 1995.- T-cell suppression and selective in vivo activation ofTh2 subpopulation by the Entamoeba histolytica 220-kilodalton lectin. Infection and Immunity, 63: 3953-3958. TARLETON (R.L.), 1988a.- Trypanosoma cruzi-induced suppression of IL-2 production. I. Evidence for the presence of IL-2 producing cells. Journal of Immunology, 140: 2763-2768. TARLETON (R.L.), 1988b.- Trypanosoma cruzi-induced suppression of IL-2 production. H. Evidence for a role for suppressor cells. Journal of Immunology, 140: 2769-2773. TARLETON (R.L.) & KUHN (R.E.), 1984.- Restoration of in vitro immune responses of spleen cells from mice infected with Trypanosoma cruzi by supematants containing interleukin 2. Journal of Immunology, 133: 1570-1575. TAVERNE (1.), BATE (C.A.W.), KWIATKOWSKI (D.), lAKOBSEN (P.H.) & PLAYFAIR (1.H.L.), 1990.- Two soluble antigens of Plasmodiumfalciparum induce TNF release from macrophages. Infection and Immunity, 58: 2923-2928. TEXEIRA (R.L.) & SANTANA (J.M.), 1989.- Trypanosoma cruzi: endocytosis and degradation of specific antibodies by parasite forms. American Journal of Tropical Medicine and Hygiene, 40: 165. THEANDER (T.G.), BYGBJERG (I.C), ANDERSEN (BJ.) JEPSEN (S.), KHARAZMI (A.) & ODUM (N.), 1986.- Suppression of parasite specific response in Plasmodium falciparum malaria. A longitudinal study of blood mononuclear cell proliferation and subset composition. Scandinavian Journal of Immunology, 24: 73-81. THEANDER (T.G.), SVENSON (M.), BYGBJERG (I.C), KHARAZMI (A.), JEPSEN (S.), ANDERSEN (B.1.) & LARSEN (P.B.), 1987.- Inhibition of human Iymphocyte proliferative response by serum from Plasmodium falciparum infected patients. Acta Pathologica, Microbiologica et lmmunologica Scandinavica, C95: 257263. TRISSL (D.), 1982.- Immunology of Entamoeba histolytica in human and animal hosts. Reviews of Infectious Diseases, 4: 11541184. TSCHOPP (1.) & NABHOLZ (M.), 1990.- Perform-mediated target cell lysis by cytolytic T Iymphocytes. Annual Review of Immunology, 8: 279-302. TURCO (SJ.) & DESCOTEAUX (A.), 1992.- The lipophosphoglycan of Leishmania parasites. Annual Review of Microbiology, 46: 65-94. URQUHART (G.M.) & HOLMES (P.H.), 1987.- African trypanoso- Immune evasion mechanisms by protozoa miasis. In: Immune Responses in Parasitic Infections, Immunology, Immunopathology and Immunoprophylaxis, Vol. 3 (E.J.L. Soulsby edit.), CRC Press, Boca Raton, Florida: 1-22. URQUHART (G.M.), MURRAY (M.), MURRAY (P.K.), JENNINGS in Trypano(F.W.) & BATE (E.), 1973.- Immunosuppression soma brucei infections in rats and mice. Transactions of the Royal Society of Tropical Medicine and Hygiene, 67: 528-535. VAN DER PLOEG (L.H.T.), 1987.- Control of variant surface antiCell, 51: 159-161. gen switching in trypanosomes. VICKERMAN, (K.), 1978.- Antigenic variation in trypanosomes. Nature (London), 273: 613-617. VICKERMAN (K.), 1985.- Developmental cycles and biology of British Medical Bulletin, 41: 10 15pathogenic trypanosomes. 1114. WAKELIN (D.) & BLACKWELL (1.M.), 1993.- Genetic variations in immunity to parasitic infections. In: Immunology and Molecular Biology of Parasitic Infections (K.S. Warren edit.), Blackwell, London: 3-22. WALDERICH (B.), WEBER (A.) & KNOBLOCH (J.), 1997.- Sensitivity of Entamoeba histolytica and Entamoeba dispar patient Parasite Immunology, 19: 265isolates to human complement. 271. 83 WALSH (1.), 1986.- Amebiasis in the world. Archivos de Investigacion Medica (Mexico), 17: 385-389. WANG (W.) & CHADEE (K.), 1995.- Entamoeba histolytica suppresses gamma interferon-induced macrophage class II major histocompatibility complex la molecule and I-Ab mRNA expression by a prostaglandin E2-dependent mechanism. Infection and Immunity, 63: 1089-1094. WHITTLE (H.C.), BROWN (1.), MARSH (K.), BLACKMAN (M), JOBE (0.) & SHENTON(F.), 1990.- The effects of Plasmodium falciparum malaria on immune control of B lymphocytes in Gambian children. Clinical and Experimental Immunology, 80: 213-218 WOLFE (M.A.), 1984.- Symptomatology, diagnosis, and treatment. In: Giardia and Giardiasis (S.L. Erlandsen & E.A. Meyer edit.), Plenum, New York: 147-16l. WYLER (DJ.), 1976. Peripheral lymphocyte subpopulations in human falciparum malaria. Clinical and Experimental Immunology, 23: 471-476. ZALMAN (L.S.), WOOD (L.M.) & MULLER-EBERHARD (HJ.), 1987.-Inhibition of antibody-dependent lymphocyte cytotoxicity by homologous restriction factor incorporated into target cell membranes. Journal of Experimental Medicine, 166: 947955.