* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 11 Glaucoma Primary Open Angle Glaucoma
Contact lens wikipedia , lookup
Vision therapy wikipedia , lookup
Keratoconus wikipedia , lookup
Visual impairment wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Macular degeneration wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Corneal transplantation wikipedia , lookup
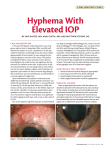
Chapter 11. Glaucoma Concept: Those suffer from pathologic high IOP which is sufficient to cause excavation of optic disc, optic atropy and characteristic loss of visual field are called glaucoma. IOP is a major risk factor, but not always, especially for open angle glaucoma, normal tension glaucoma. Vascular or ischemic factors Neuroprotection Primary angle closure glaucoma Etiology: blockage or permennant synechia of trabecular meshwork by peripheral iris. narrow angle, small eye, shallow anterior chamber Acute angle-closure glaucoma Etiology: still unknown often induced by fatigue, anxiety, anger small or crowded eye: short axis of the globe small cornea shallow anterior chamber narrow angle, thick lens Clinical manifestation Staging: 1. Preclinical stage 2. Premonitory stage 3. Acute attack 4. Remission stage 5. Chronic stage 6. Absolute stage Diagnosis and differential diagnosis Acute attack :nausea, vomitting,headache; Congestion Edematous cornea Reduced vision High IOP Shallow chamber Pupil dilated feckle 1. Acute conjunctivitis 2. Acute iridocyclitis Treatment 1. IOP controled with 20% mannitol, 1% pilocarpine 0.25% timolo, diamox, etc 2. Peripheral iridectomy laser iridotomy 3. Trabeculectomy Chronic angle-closure glaucoma Etiology: still unknown shallow chamber narrowed angle goniochia Clinical manifestation IOP increase progressively Excavtion of optic cup Visual field loss seidal scotoma nasal step arcute scotoma circuit scotoma tubular vision Treatment 1. Medical treatment 0.25% pilocarpine 0.5% timolo diamox mannitol if necessary 2. Peripheral iridectomy or trabeculectomy according to gonioscopy Primary Open Angle Glaucoma Etiology: still unknown Characteristics: high IOP angle open pathologic findings on trabecular meshwork and Schlemm’s cannal Clinical findings Symptoms: usually no symptoms usually found at late stage few blurred vision, pain of the eye IOP: fluctuated at early stage high at late stage 24-hour IOP curve is important for abnormal findings Clinical findings Anterior Segment of Eye: usually no abnormal findings Fundus Examination: key tips 1. optic cup enlarged and deepened 2. narrowing of neuroretinal rim 3. larger C/D ratio 4. unsymmetric C/D ratio 5. hemorrhage on or near optic disc 6. loss of optic nerve fiber Clinical findings visual function: loss of visual field 1. paracentral scotoma 2. arcuate scotoma 3. quadrant field loss 4. tubular visual field Diagnosis IOP: 24-hour IOP curve important Optic cup changes: Visual field loss: any patient with either 2 of the 3 signs mentioned above plus an open angle, diagnosis can be made. Treatment Medical: target IOP: various, individual beta-blockers or alpha-excitors diamox( carbonic anhydrase inhibitor) latanoprost Laser : trabeculoplasty Filtering surgery trabeculectomy nonpenetrating trabecular surgery reversed trabeculectomy Congenical glaucoma Infantile glaucoma Juvenile glaucoma abnormalities of angle Surgery trabeculotomy goniotomy Chapter 12. Uveal Diseases Anatomy: 1. iris 2. ciliary body 3. choroid Characteristics: abundant in blood vessels abundant in pigment Uveitis Etiology & Mechanism 1. Infection: bacteria, virus, fungus etc 2. Auto-immune factors: antigens 3. Oxidation damage 4. Arachidonic acid 5. Immuno-inheritance: HLA antigen Anterior Uveitis Including: 1.iritis: iris only 2. Iridocyclitis: iris + ciliary body 3. Cyclitis: ciliary body only Classification: 1. Acute: HLA-B27 (+) 2. Chronic: Fuchs 3. Both acute and chronic Clinical Manifestation Symptoms: pain photophobia tearing blurred vision Signs: 1. ciliary or mixed congestion congestion near limbus due to dilation of episcleral vessels notice: keratitis and PACG 2. KP( keratic precipitate) indicating endothelial damage and inflammatory cell or pigment existing dust KP: non-sarcoid uveitis neutrocyte, lymphocyte, plasma middle sized KP: Fuchs syndrome, HSK mutton KP: sarcoid uveitis mono-nuclear macrophage 3. Aqueous flare: damage of blood-aqueous barrier, protein entering into anterior chamber; no meaning of active inflammation 4. Aqueous cells: indicating the severity of inflammation inflammatory cells like white-greyish dust going up near iris, coming down near cornea causing KP formation and hypopyon 5. Iris changes: posterior synechia: iris to lens anterior synechia: iris to cornea iris nodules: Koeppe Bussaca irido-sarcoma 6. Pupil changes: small pupil irregular pupil seclusion of pupil occlusion of pupil 7. Lens changes: pigment on lens cataract 8. Vitreous changes: inflammatory cell Complications 1. Cataract: aqueous changing leading to abnormal metabolism of lens and longterm use of steroids 2. Glaucoma: obstruction of trabecular meshwork, anterior iris synechia, occusion or seclusion of pupil 3. Low IOP & atrophy: atrophy of ciliary body leading to less secretion of aqueous Differential Diagnosis 1. Acute conjunctivitis 2. Acute angle closure glaucoma 3. Ocular tumour 4. Panuveitis Treatment 1. Cycloplegia: pain of the eye homatropine is ideal, better, lasting 18~36 hours atropine lasting longer,no recommendaed 1). prevent and treat posterior synechia 2). relieve ciliary and sphincter spasm 2. Steroid eye drops: predineson is the best owing to good penetration into anterior chamber sub-conjunctival injection should not be used in anterior uveitis 3. Nsaid eye drops: prostaglandin,etc. 4. Systemic use of steroids: 5. Etiologic treatment: 6. Treatment for complications Sympathetic Ophthalmia Etiology: auto-antigen exposure after penetrating wound or operation, resulting in auto-immune response. Clinical manifestation: severe uveitis Treatment: large dose of steroids other anti-immunologic drugs Prognosis: used to be very poor much better right now