* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
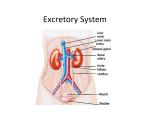
Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 1 of 7 Attention: Transcript contains all lecture powerpoint notes and all additional comments made during class. Notes that were not mentioned are underlined. I. Introduction [S1]: II. General Remarks [S2] III. Body Cavities [S3] a. The abdominal (yellow) and pelvic (green) cavites are continuous with each other and are sometimes referred to collectively as the abdominopelvic cavity. b. The separation (for descriptive purposes) between the two cavities is the oblique plane of the superior pelvic aperture (= pelvic inlet, pelvic brim). This plane passes from the upper border of the pubic symphysis to the upper edge of the sacrum posteriorly—sacral promontory. i. The pelvic and abdominal cavities are continuous at this plane. c. Some parts of the urinary system (kidneys) lie in the abdomen on the posterior abdominal wall, some parts (urinary bladder) lie in the pelvis, and some (ureters) lie in both the abdomen and pelvis. IV. Peritoneal vs. Retroperitoneal Organs [S4] a. Sagittal section: b. The peritoneum is a serous membrane that lines the abdominal and pelvic cavities and secretes serous fluid to keep the surfaces of the organs moist and allows movement without friction. c. There are two parts to the peritoneum: i. Parietal peritoneum - lines the body (abdominal and pelvic) walls, including partially covering the organs that lie on these walls (eg, the superior surface of the urinary bladder is covered parietal peritoneum of the anterior abdominal wall and then moves on to the anterior surface of the rectum and on to the posterior abdominal wall; this is all parietal peritoneum). 1. These organs are referred to as retroperitoneal (partially covered) 2. The entire urinary system (kidneys, ureters, and urinary bladder) is retroperitoneal. ii. Visceral peritoneum - completely surrounds the organs (eg, most of small intestine). 1. These organs are referred to as peritoneal. 2. Peritoneal organs are attached to the posterior abdominal wall by folds of peritoneum termed mesenteries (“a double layer of peritoneum”) V. Kidneys [S5] VI. Function and Posterior Relationships of Kidneys [S6] a. The kidneys are retroperitoneal (peritoneum has been removed). b. The kidneys extend from the T12 to the L3 vertebral level. c. The right kidney is slightly lower than the left b/c the mass of the right lobe of the liver pushes it inferiorly. d. The kidneys are reddish-brown in life and measure ~ 10 cm long, 5 cm wide, and 2.5 cm thick. e. Note the posterior relationships of the kidneys: muscles and nerves of post. abdominal wall. i. upper part of the kidney lies on the diaphragm posteriorly ii. transversus abdominis m. is another abdominal muscle the kidney lies on posteriorly iii. quadratus lumborum m. & psoas major m. are also directly posterior to the kidneys f. Note the relationships of the nerves that pass posteriorly to the kidneys on each side: i. The subcostal n. (branch of 12th spinal nerve) ii. The ilioinguinal & iliohypogastric n. (both are branches of the 1st lumbar nerve) g. All of these are DIRECT POSTERIOR relationships to the kidneys. h. The function of the kidneys is to maintain the body’s fluid and electrolyte balance. i. This is accomplished by the formation of urine, which is excreted into a duct system. VII. Anterior Relationships of Kidneys [S7] a. Review the anterior relationships of the R and L kidneys. b. Note that part of the kidney is covered by peritoneum and other parts are not. c. Note that each kidney is capped superomedially by a suprarenal gland. d. Right Kidney: i. Anterior relationships include the right lobe of the liver, the descending part of the duodenum (2nd part)— the beginning part of the small intestine, the right colic flexure (“the hepatic flexure”)—where the ascending colon makes a bend to become the transverse colon, the jejunum (coils of the small intestine). e. Left Kidney: i. Anterior relationships include the stomach and spleen, the descending colon, coils of jejunum. VIII. Relationships of Kidneys (Transverse Section) [S8] a. Note relationships of kidneys as seen in this transverse section (looking at the body from below). b. The right kidney is very close to the right lobe of the liver. c. The stomach and spleen are major anterior landmarks of the left kidney. Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 2 of 7 d. On both sides, the diaphragm is visible lying posterior to reach kidney. IX. Renal Fascia and Associated Fat [S9] a. There is some disagreement re: the arrangement of the renal fascia around the kidneys. The following description follows Gray’s Anatomy for Students, pp. 321-323. b. There is a lot of fat and fascia surrounding the kidneys. c. The renal fascia consists of two layers (anterior and posterior). i. Laterally, the two layers fuse (this fused layer may connect w/the transversalis fascia—lines the entire inner surface of the abdominal wall and just internal to the tranversus abdominus muscle). ii. Medially, the two layers are not fused; the anterior layer of fascia continues over the vessels in the hilum and fuses w/the CT associated w/the abdominal aorta and IVC; the posterior layer continues over the psoas major m. (one of the muscles that lies behind the kidney) iii. Superiorly (not visible from this view), the two layers fuse and blend w/the fascia that covers the inferior surface of the diaphragm (the layers also enclose the suprarenal gland, although a thin septum usually intervenes between the kidney and suprarenal gland). 1. Note that each kidney is capped superomedially by a suprarenal gland (a.k.a. adrenal gland). iv. Inferiorly, the anterior and posterior layers of renal fascia enclose the ureters and do not fuse completely, but are held together in a loose fashion. (Nevertheless, according to COA, 5th ed., p. 308, the ant. and post. layers of renal fascia are only united loosely, if at all, inferiorly). 1. Thus, pus from a perinephric abscess or blood from an injured kidney may force its way into the pelvis between the two layers of renal fascia. There is nothing to stop it because these two layers don’t fuse firmly below. It is a pathway for blood to travel inferiorly. v. Medially, the posterior layer of fascia fuses with the fascia over the psoas major m. d. The fat immediately surrounding the kidney, but inside the renal fascia, is the perirenal (perinephric) fat. e. The fat immediately surrounding the outside the renal fascia is the pararenal (paranephric) fat. f. The renal fascia, perirenal and pararenal fat, and the tethering provided by the renal vessels and ureter hold the kidneys in a relatively fixed position. However, kidneys do move vertically with respiration and change in body position (normal mobility is ~ 3 cm.) as the diaphragm descends and pushes the kidneys inferiorly. i. Because the renal fascia surrounds the kidney, it must be incised in any surgical approach (anterior or posterior) to the kidney. ii. The fact that the renal fascial layers do not unite firmly inferiorly (don’t provide good support) is one of the reasons transplanted kidneys are placed in the iliac fossa to provide more support to the kidney. iii. Other reasons of the location of the kidney deep in the pelvis are the availability of major blood vessels (e.g. external iliac a. & v.) to which the renal vessels can be anastamosed with and because of the convenient access to the bladder. X. Gross External Structure of Kidney (Ant. View) [S10] a. External gross structure of kidney shown in this slide: i. Kidney surrounded by a fibrous capsule (but has been stripped away in this diagram). ii. Each kidney has sup. and inf. poles, lateral and medial borders, and ant. and post. surfaces. 1. Medial border indented to form the hilum (= hilus) , which is where renal v., a., and pelvis (upper expansion of the ureter) enter or leave kidney (vein most anterior, pelvis most posterior). a. “hilus/hilum” is a general term for any organ referring to the opening where nerves, vessels & lymphatics may enter or leave. iii. The kidney has a smooth outer appearance, unless you have persistent lobation from a fetal condition. XI. Gross Internal Structure of Kidney (Ant. View) [S11] a. Gross internal structure shown in this slide in a sagittal section: b. Kidney consists of an outer rind of cortex (light colored, granular in appearance, and contains renal corpuscles and convoluted tubules), and a deeper, inner medulla (dark, pyramidal shaped masses that contain collecting tubules and are often referred to as renal pyramids). c. Cortex and its associated pyramid constitute a lobe of the kidney. i. Tip of each renal pyramid is termed a renal papilla, and projects into a cup-shaped structure—minor calyx. ii. The collecting tubules that are in the medulla open up on the tip of the papilla as tiny foramina and drain urine formed in the kidney into the minor calices. The minor calices unite to form major calices, which unite to form the renal pelvis. The pelvis then leaves the hilum of the kidney and tapers to become the ureter. iii. The area just internal to the hilum of the kidney that is filled with a lot of fat, major calices and part of the renal pelvis is called the renal sinus. iv. The upper end of the ureter expands into the renal pelvis, which enters the renal sinus (a cavity filled with fat) at the hilum. The pelvis divides into several major calices, each of which divides into several minor calices. d. Cortex also extends between pyramids as renal columns. Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 3 of 7 XII. Renal Arteries and Veins In Situ [S12] a. The renal arteries are paired visceral branches of the abdominal aorta, which arise at the disc between LV1/LV2, which is about the same level that the superior mesenteric artery comes off (an example of an unpaired visceral artery (shown on slide), which goes to the GI tract). b. The R renal artery passes posterior to the IVC. c. The pararenal veins drain into the IVC. i. The L renal v. is longer than the right, and passes in front of the aorta to empty into the IVC. ii. Because of the asymmetry of the position of the vena cava, the L renal v. receives the L suprarenal v. and L gonadal v. (whether testicular or ovarian) as tributaries, whereas these veins on the right side drain directly into the IVC. XIII. Intrarenal Arteries [S13] a. Near the hilum, the renal a. divides into five segmental aa.: i. superior (apical) segmental a. - going to the upper pole ii. inferior segmental a. iii. anterior superior segmental a. iv. anterior inferior segmental a. v. posterior segmental a. 1. Each of these segmental aa. supplies a distinct area of kidney tissue, with no significant anastomoses with other segmental aa. Thus each kidney segment is a surgically resectable unit. XIV. Ureters [S14] XV. Function and Relationship of Ureter [S15] a. The ureter serves as a duct to conduct urine from the kidney to the urinary bladder. b. The upper one-half lies in the abdomen; lower one-half in the pelvis (the pelvic brim area). c. The ureter is a muscular tube with smooth muscle and transports urine by peristaltic action (a few drops at a time, at intervals of (12) 15- 20 seconds) into the urinary bladder. d. The ureter is ~25 cm long. e. The ureter is retroperitoneal throughout its course. f. In the abdomen it descends on and directly in front of the psoas major m., and is crossed anteriorly by the gonadal vessels (testicular or ovarian). g. At the pelvic brim, the ureter crosses the bifurcation of the common iliac artery. It then passes anteriorly on the lateral pelvic wall still in a retroperitoneal position (directly deep to the peritoneum) and turns medially to pierce the posterior wall of bladder wall at the superolateral angles of the trigone. h. The passage or the ureter through the bladder wall is oblique and serves as a valve-like mechanism so that when the bladder musculature contracts it acts as a sphincter, preventing reflux of urine into the ureter. i. Not mentioned here, but mentioned on [S26] XVI. Structures Crossing Ureters in Pelvic Cavity [S16] a. Half of the slide is a female orientation, half is a male orientation. b. Orient: Superior view of the pelvis. Note the urinary bladder directly behind the pubic symphysis & the rectum. i. In the female the uterus is located between the bladder and the rectum. c. Note the more distal aspects of the ureter: i. In males, the terminal part of the ureter is crossed by the vas (ductus) deferens. 1. Note the path the male ureter takes: coming down, crossing the pelvic brim, running along the lateral aspect of the pelvic wall and then bending medially…at this point, just as the ureter is about to pierce the bladder wall posteriorly, it is crossed by the terminal part of the vas (ductus) deferens—the main sperm duct in the male. ii. In females, the terminal part of the ureter is crossed by the uterine a. (a branch of the internal iliac artery) 1. This is a clinically important relationship: when ligating the uterine a. during a hysterectomy (removal of uterus), care must be taken not to damage the underlying ureter! a. Pneumonic: “water under the bridge”—ureter goes under the uterine artery XVII. Sites of Constriction of Ureter [S17] a. The three sites where the ureter is constricted are areas where kidney stones (renal calculi) are apt to lodge. b. The passage of the ureter piercing through the bladder wall is the narrowest site and the most common site i. The other two locations of ureter constriction are where: 1. the ureter meets the renal pelvis (ureteropelvic junction) 2. the ureter crosses the pelvic brim as it crosses the common iliac artery bifurcation c. The pain from a renal calculus can be severe. The pain passes from the “loin to the groin” as the stone gradually moves downward and forward in the ureter. i. The afferent fibers coming from the ureter enter spinal cord segments T11-L2. Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 4 of 7 ii. The pain is referred to cutaneous areas (dermatomes) T11 – L2, the same cord segments that receive visceral afferents from the ureter and often complain of pain along the abdominal wall along the strips of skin (dermatome). iii. T11 dermatome is just below the umbilicus, which is T10. iv. Summary: The kidney stone patient will feel the pain in the dermatome regions T11-L2 because the afferents from the skin (dermatomes T11-L2) are entering the same spinal cord segments the afferents from the ureter are and the CNS interprets the pain as coming from the skin, rather than the ureter itself. v. Renal stones can be treated by lithotripsy (using shock waves to break up a stone into small fragments that can be passed in the urine). XVIII. Arterial Supply to Ureter [S18] a. The ureter is supplied by numerous arteries as it courses through the abdomen and pelvis such as the renal artery, gonadal artery, branches of the aorta, branches from the common iliac artery all in the abdomen region. As well as those branches in the pelvic region off the internal iliac artery or some of its branches. b. Each of these arteries supplies a small segment of the ureter. c. Branches supplying the abdominal half of the ureter approach medially, while those supplying the pelvic half approach laterally. i. Clinical relevance: during surgery, the ureters are avoided and left undisturbed when possible; if necessary, traction of the ureters should be applied gently and only toward the blood supply (i.e. in the abdomen— medially, in the pelvic—laterally) to avoid disruption of the small (delicate) branches. If a part of the ureter becomes necrotic, it can rupture after surgery and leak urine. d. The veins of the ureters correspond with its arteries. XIX. Urinary Bladder [S19] XX. FEMALE: Function and Relationships of Bladder [S20] a. The urinary bladder is a resevoir for urine (it can hold up to ~ 500 cc of urine). b. When empty, it lies in the true (lesser) pelvis, but as it fills it rises above the pubic symphysis into the abdomen. c. The bladder has a thick wall of smooth muscle (the detrusor m.—“to push down or thrust out”). d. Relationships of bladder in female: i. Anteriorly: pubic symphysis & the area just behind the pubic symphysis—retropublic space (not shown) that has loose connective tissue which allows the bladder to fill up and expand and has a venous plexus in this space as well ii. Posteriorly: superior part (upper ½) of vagina iii. Superiorly: peritoneum of the vesicouterine pouch 1. Note: the peritoneum is reflected off the superior surface of the bladder onto the uterus and causes the space of the vesicouterine pouch. 2. The uterus normally hangs over the superior surface of the bladder as shown here. 3. The vesicouterine pouch is part of the peritoneal cavity. iv. Inferiorly: urogenital diaphragm 1. The neck of the bladder (inferior most part of the bladder) is directly above the urogenital diaphragm, which is a muscular structure that stretches between the pubic bones. v. Laterally (on each side):obturator internus m. (above, not shown) & pelvic diaphragm (levator ani m.) below 1. The pelvic diaphragm is a sheet of muscle that stretches along the floor of the pelvis and helps to support the pelvic viscera (including the bladder itself). a. The pelvic diaphragm is actually made up of two muscles, but the most important is the levator ani m. XXI. MALE: Relationships of Bladder [S21] a. Relationships of the bladder in male: i. Anterior: pubic symphysis and retropubic space (note the vesical venous plexus & connective tissue) ii. Posterior: seminal vesicles (one on each side), behind that is the rectum, between the upper part of the posterior surface of the bladder and the rectum is the rectovesical pouch of peritoneum (no uterus present), and the terminal parts of the vasa deferentia (not labelled) iii. Superior: peritoneum iv. Inferior: prostate gland v. Lateral: obturator internus m. (above) (not shown), pelvic diaphragm (levator ani m.) below 1. Similar to the female XXII. MALE: Relationships of Bladder (Post. View) [S22] a. Posterior view of the male bladder. Note the posterior and inferior relationships. The peritoneum has been stripped off the upper surface of the bladder and the detrusor m. of the bladder wall can be seen. b. The ampulla of the ductus deferens and the semimal vesicles (directly posterior to the bladder) are well shown. Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 5 of 7 i. Note how the terminal part of the ductus deferens also lies posterior to the bladder and crosses superior to the terminal part of the ureter. c. Inferiorly, the bladder is related to the base of the prostate gland. i. The ejaculatory duct is formed by the junction of the ductus deferens and the seminal vesicle. 1. The ejaculatory duct will eventually penetrate the prostate gland. XXIII. Relationships of the Distended Bladder [S23] a. The bladder is a pelvic organ in the adult (when the bladder is empty), but when the bladder fills, it rises above the pubic symphysis into the abdomen and becomes an abdominal organ, stripping the peritoneum off the anterior abdominal wall. i. This is clinically relevant because if the bladder needed to be drained it could be done so through the urethra, but also through the anterior abdominal wall and it can be done without penetrating the peritoneum. This is possible because possible infection of the peritoneum is still be avoided. ii. Thus, a catheter can be inserted into the distended bladder w/o entering the peritoneal cavity. b. In some individuals, the fully distended bladder may rise to the level of the umbilicus (T10 level)! XXIV. Bladder of an Infant [S24] a. The bladder of an infant is fusiform in shape and lies entirely in the abdominal cavity (even when empty), above the pubic symphysis. The bladder does not lie entirely within the true (lesser) pelvis until after puberty. XXV. Parts and Surfaces of the Bladder [S25] a. The bladder has four surfaces: superior, two inferolateral on either side, and posterior (= fundus or base of the bladder). If the bladder has a base, then it also has an apex (anterosuperiorly) and the most inferior part of the bladder—the neck (where the inferolateral and posterior surfaces meet inferiorly and marks the beginning of the urethra at the neck of the bladder). XXVI. Interior of the Bladder [S26] a. Coronal section of the bladder looking at the posterior wall of the bladder. b. The mucosa lining the interior of the bladder is wrinkled in most places of the bladder wall because it is loosely attached to the muscular wall. However, in the fundus of the bladder, there is a triangular area of mucosa (the trigone), which is smooth, even when the bladder is empty because the mucosa is tightly bound to the musculature in the region of the trigone. c. The trigone is in the form of an equilateral triangle, the two superolateral angles being the slitlike orifices of the ureters and the inferior angle being the internal urethral orifice. i. As the ureters pierce the bladder wall, they pass obliquely through the bladder wall, which acts as a valvelike mechanism, so when the detrusor muscle contracts forcing urine out it also prevents urine from refluxing back up into the ureter. d. Inferiorly, at the intra-angle of the trigone, is the internal urethral orifice, which is a region of the neck of the bladder where the urethra begins. XXVII. Blood Supply of the Bladder [S27] a. The bladder receives its arterial supply via the superior vesical a. (which supplies the anterosuperior part of the bladder) and the inferior vesical a. (which supplies the fundus and neck of the bladder in the male a.). i. Both the superior vesical a. & inferior vesical a. are direct or indirect branches of the internal iliac a.--CHIEF ARTERY of the PELVIS. ii. In females, the vaginal a. replaces the inferior vesical a. b. Vesical venous plexus surrounds the bladder and lies in the retropubic space and drains into the internal iliac v. XXVIII. Urethra [S28] XXIX. MALE & FEMALE: Function and Course of Urethra [S29] a. In both sexes, the urethra conducts urine from the bladder to the exterior. i. In the male, the urethra also conducts semen—the secretions of the seminal vesicle, prostate gland and the sperm in the vas deferens. b. The course of the urethra differs considerably in the two sexes, primarily because in the male the spongy part of the urethra traverses the penis, whereas in the female the urethra is much shorter and does not traverse the clitoris. c. The fact that the urethra in the female is much shorter (~4cm long) than in the male (~20 cm), and opens into the vestibule of the vagina (space between the labia minora) means that bladder infections are much more common in women. XXX. MALE: Parts and Relationships of the Urethra [S30] a. The urethra in the male has three parts: the prostatic part (3-4 cm) surrounded by the prostate gland, and gently concave forward, the membranous part (~1 cm) surrounded by the sphincter urethrae m., and the spongy part (~15 cm), which is surrounded by the corpus spongiosum (erectile tissue) of the penis. b. The urethra terminates in a vertical slit on the glans of the penis (termed the external urethral meatus). Renal: 1:00 - 2:00 Monday, May 4th, 2009 Dr. Zehren Anatomy of the Urinary System XXXI. MALE: Parts and Relationships of Urethra [S31] a. Coronal section looking at the posterior wall of the prostatic urethra: b. Note that the prostate gland and penis have been split longitudinally. Scribe: Ryan O’Neill Proof: Strud Tutwiler Page 6 of 7 c. The prostatic urethra has several features of note: d. On the posterior wall of the prostatic urethra is a longitudinal ridge, the urethral crest. i. On either side of the crest is a groove (prostatic sinus), which receives the openings of the ducts of the prostate gland. 1. On the crest is a small elevation (seminal colliculus), which has three tiny openings on it. a. The central opening is the prostatic utricle, a blind diverticulum (< 1cm), which projects into the substance of the prostate gland and has no functional significance. i. The utricle is believed to be homologous w/ the uterus and vagina in the female. ii. On either side of the prostatic utricle is the opening of an ejaculatory duct iii. Thus sperm and the secretions of the seminal vesicles and prostate gland all reach the lumen of the prostatic urethra. iv. The prostatic urethra is the widest and most distensible part of the urethra. e. The membranous urethra (shortest segment ~ 1cm) pierces the sphincter urethrae m. (which is a voluntary sphincter of the urethra). i. The membranous urethra then leaves the confines of the sphincter urethrae and enters the bulb of the penis (the proximal end of the corpus spongiosum) and pierces a fibrous structure (perineal membrane) (not labelled) to become the spongy urethra. f. The spongy part (specifically in the part that is within the bulb of the penis) of the urethra traverses the corpus spongiosum of the penis. i. The spongy part of the urethra has a diameter of ~5 mm throughout most of the length of the penis, but in the bulb it is slightly larger and in the glans it again widens as the navicular fossa. g. The external urethral meatus is the narrrowest and least distensible part of the entire urethra (thus an instrument passing thru the meatus should pass thru any of the other parts of the urethra). i. Passage through the external urethral meatus is the most difficult area to place a catheter into. h. The spongy urethra (proximal part) receives the openings of the ducts of the bulbourethral (“Cowper’s) glands (which secrete a mucous-like substance during sexual arousal). These glands are surrounded by the sphincter urethrae m. Their ducts do not empty into the membranous urethra, they empty into the spongy urethra. i. More distally the spongy urethra receives the openings of the ducts of numerous minute, mucous urethral glands. XXXII. MALE: Muscles in the Deep Perineal Space [S32] a. Urogenital diaphragm from an inferior view. Note the pubic symphysis anteriorly. b. The deep perineal space is a space lying superior to the perineal membrane, a fibrous structure spanning between the ischiopubic rami. The perineal membrane has been largely removed in the slide to show the muscles that lie in the deep perineal space, which is the space above the perineal membrane. c. There are two muscles that occupy the deep perineal space. Together, they make up the urogenital diaphragm. i. The sphincter urethrae m. surrounds the membranous urethra and can constrict (voluntarily) the urethra to stop the flow of urine. ii. The other muscle that lies in the deep perineal space is the deep transverse perineal m. d. The sphincter urethrae m. is not confined to a flat plane, but extends superiorly to partially surround the prostate gland ( X see next slide). i. It is a skeletal muscle (voluntary control). e. The bulbourethral glands lie posterolateral to the membranous urethra (their ducts pierce the perineal membrane to enter the spongy urethra, not into the membranous urethra). XXXIII. FEMALE: Relationships of the Urethra [S33] a. The female urethra is much shorter and begins at the neck of the bladder and continues inferiorly to open into the vestibule of the vagina, which is the space the space that receives the vaginal orifice and the urethral orifice. b. It is ~ 4 cm long and its lumen is ~ 5mm in diameter. c. As it passes inferiorly it is surrounded by the sphincter urethrae m., and it pierces the perineal membrane. d. The urethra lies posterior to the pubic symphysis and anterior to the lower one-half of the vagina. i. Thus the urethra can be bruised during childbirth by compression against the pubic symphysis. XXXIV. FEMALE: Muscles in the Deep Perineal Space [S34] a. Inferior view of the urogenital diaphragm in the female. b. As in the male, the deep perineal space contains the sphincter urethrae m. and the deep transverse perineal m. Renal: 1:00 - 2:00 Scribe: Ryan O’Neill Monday, May 4th, 2009 Proof: Strud Tutwiler Dr. Zehren Anatomy of the Urinary System Page 7 of 7 c. However, two additional muscles found in this space (females only) are the compressor urethrae m. and the sphincter urethrovaginalis m. and assist the sphincter urethrae m. All three of these muscles help control the flow of urine in the female. i. Summary: The compressor urethrae m. and sphincter urethrovaginalis m. aid the sphincter urethrae m. in closing the urethra (all are voluntary muscles). d. All the muscles of the deep perineal space are innervated by the perineal branch of the pudendal n. (both sexes). Voluntary innervation of these muscles. XXXV. Lymphatic Drainage of the Urinary System [S35] a. Kidneys: i. The lymphatic drainage is to the lumbar nodes (which are a chain of lymph nodes lying on either side of the abdominal aorta) and then via lumbar lymph trunks to the cisterna chyli (not shown, sac-like structure that will taper superiorly to become the thoracic duct), which lies just below the diaphragm b. Ureters: i. Lymphatic drainage of abdominal part of ureter is to lumbar and common iliac nodes (along the common iliac vessels). ii. Lymphatic drainage of pelvic part of ureter is to internal and external iliac nodes, which are adjacent to their blood vessels c. Bladder: i. Drainage from superior and inferolateral surfaces is to external iliac nodes. ii. Drainage from fundus (base of the bladder) is to both internal and external iliac nodes. iii. Drainage from neck is to sacral and median(l) common iliac nodes. (sacral nodes are located near the 2nd and 3rd sacral foramina). XXXVI. Nerve Supply to the Urinary System [S36] a. There are nerve plexuses that surround various vessels. b. Kidneys: i. Innervated via the renal plexus that surround the renal arteries. 1. Efferent fibers in this plexus are vasomotor (to muscular coats of afferent and efferent arterioles) that will cause constriction of the blood vessels on the kidney (e.g. renal aa. and their branches) and help reduce blood flow to the kidneys which will alter urine formation. a. Nerves appear to influence urine formation only by changing blood supply to kidney. 2. Afferent fibers in this plexus end in spinal cord segments T10-T12 (prob.). c. Ureter: i. The abdominal part of ureter is innervated by the renal and “gonadal” (testicular or ovarian) plexuses. ii. The pelvic part of the ureter is innervated by the inf. hypogastric (“pelvic”) plexus. iii. Afferents from the ureter enter spinal cord segments T11-L2, L1 (prob.). 1. Review referred pain in the ureter discussed earlier. d. Urinary Bladder: i. The bladder is innervated by the vesical plexus, which is an “offshoot” of the inferior hypogastric plexus. 1. “vesical” refers to the bladder in the urinary system ii. Proprioceptive afferents (sensitive to stretch of the bladder wall) in this plexus travel back to spinal cord segments S2 – S4 via the pelvic splanchnic nerves. 1. This will initiate a reflex when the bladder gets full & trigger the emptying reflex via the efferent fibers. 2. Remember: Proprioceptive = stretch receptors iii. Parasympathetic fibers in the plexus reach it via the pelvic splanchnic nerves and cause contraction of the detrusor m. of the bladder wall. This is the emptying reflex. 1. The presynaptic parasympathetic fiber cell bodies lie in the sacral cord segments S2-S4, their axons will leave the cord and travel through the pelvic splanchnic nerves to get to the vesical plexus where they synapse on small ganglion cells in the vesical plexus or even in the wall of the bladder itself. The postsynaptic muscles will travel to the detrusor m. and cause the emptying of the bladder. 2. Both the afferent (stretch) and efferent (to the detrusor m.) fibers travel through the pelvic splanchnic nerves. iv. Sympathetic fibers in the plexus supply blood vessels of the bladder and have little to do with normal voiding according to RTW. v. Afferents for pain travel with sympathetic fibers. e. Urethra (Male): (Note: this info. could be skipped) i. Branches of the pudendal n. and autonomic contributions from the cavernous plexus. XXXVII. End of Lecture [S37] [end 54:00 min]