* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download medmicro1-intro normal flora
Lyme disease microbiology wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Gastroenteritis wikipedia , lookup
Marine microorganism wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Infection control wikipedia , lookup
Schistosomiasis wikipedia , lookup
Disinfectant wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
Triclocarban wikipedia , lookup
Globalization and disease wikipedia , lookup
Transmission (medicine) wikipedia , lookup
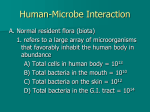
Medical Microbiology SBM 2044 Assoc Prof Dr Othman Abd Samah Tel : 09-5716744 Email : [email protected] Sr. Intan Azura Shahdan Tel : 09-5716400 ext 2816 Email : [email protected] SBM 2044 LECTURE 1 INTRODUCTION TO MODULE Value: 4 credit hours • • • • Methods of assessment Module Aims & Objectives Course structure, Reading, etc. Introduction – Recall some foundations from Principles of Microbiology SBM 2053 SBM 2044: Aims To foster knowledge and understanding of certain microbial pathogens, selected to illustrate: • various kinds of host-pathogen interactions • experimental approaches used to study bacterial/viral pathogens • molecular mechanisms in bacterial pathogenicity • clinical diagnosis and treatment Course Content • Microbes – Man interactions Week 1-3 • Medical Bacteriology Week 4-6 • Medical Virology & Biological Agents of Warfare Week 7-10 • Medical Mycology Week 11-12 • Emerging infectious diseases Week 13 • Introduction to the diagnosis and treatment of infection Week 14 Microbes – Man interactions Lecture 1: • Why is this subject important? • The normal human flora • Factors influencing bacterial-host interactions Lecture 2: • Introduction to bacterial pathogenesis Lecture 3: • Weapons delivery and deployment Today 1. How do we recognise pathogens? Only a tiny proportion of all known microbes cause disease 2. How do we identify a particular microbe as the cause of a particular disease? 3. Which microbes cause disease? 4. How do they do it? 5. How do we stop them? 6. How do we identify a particular microbe as the cause of a patient’s illness? Deaths in children (0 – 4 years) in 1998 Injury Various Noncommunicable Perinatal Nutritional 6% 3% INFECTIOUS DISEASE 8% 20% 63% Data from WHO 1999 Vineeth, 7 months old and identified as HIVpositive, cries at the Community Health Education Society orphanage in Madras, India. The WHO estimates 800,000 children were infected with HIV in 2001 alone, almost all through motherto-child transmission. Premature deaths (0 – 44 years) in 1998 Maternal Perinatal Nutritional 3% 2% 10% INFECTIOUS DISEASE 48% 18% 19% Various noncommunicable Injuries Data from WHO 1999 Human priorities ? Deaths 1945 – 1993 (in millions) Spending 1995 (in billions $) AIDS + Malaria + TB War 15 23 150 AIDS + Malaria + TB 864 Military Malaysian Facts • Population: 24,821,286 (July 2007 est.) • Death rate: 5.05 deaths/1,000 population (2007 est.) • HIV/AIDS (2003 est.) – – adult prevalence rate: 0.4% – people living with HIV/AIDS: 52,000 – HIV/AIDS - deaths: 2,000 • REFERENCE: www.cia.gov/library How do we identify a particular microbe as the cause of a particular disease? • The Koch Henle postulates 1. Isolate the organism from every case 2. Propagate in pure culture in vitro 3. Reproduce disease by injecting the organism into a suitable recipient 4. Re-isolate the organism • OK for major acute diseases like plaque, smallpox, typhoid.. • Pathogens vs. non-pathogens: the Normal Flora – Only a minute fraction of the organisms in the environment cause disease. • Isolation of an organism from a patient does not imply disease. – many different forms of association between microbes and humans – many yet unknown, non-culturable eg. In soil, water, extreme environments – Others colonise other living organisms, virtually all multicellular organisms have their own normal flora, organisms with which they coexist. Factors controlling growth 1. Nutrient availability Essential elements: • Major: C, O, H, N, S, P, K, Mg, Ca, Fe, Na, Cl • Minor: Zn, Mn, Co, Cu All present in vivo, but all not readily available to infecting bacteria – e.g. Fe • Concentration in plasma ca. 20µM • Freely available: 10-18M Pathogens • All heterotrophic (need organic C source) • Many fastidious Factors controlling growth 2. Physical environment Water activity (aw) - not limiting in vivo Osmotic pressure (π) - moderate/high • Too high for some bacteria Oxygen – availability depends on location in vivo • Anaerobic • Aerobic Facultative or Obligate • Microaerophilic Factors controlling growth 2. Physical environment – contd. Temperature: 37ºC – little variation pathogens mesophiles pH: Mostly ca. pH 7.0 in vivo, but can vary • Skin: pH 5.5 • Stomach: pH 2.0 – 5.0 Factors controlling growth 3. Competition – from normal flora Cells occupying your space Approx. number % Total Human 1013 10% Bacteria 1014 90% NORMAL HUMAN FLORA Internal organs/tissues normally sterile External surfaces & accessible ‘internal’ niches colonised by certain bacterial species – include: • Skin • Conjunctiva (eye surface) • Oral cavity • Upper respiratory tract - Nares (nostrils) & nasopharynx • Gastroinsteinal tract • Urogenital tract NORMAL HUMAN FLORA Numbers & composition varies depending on location Site numbers of bacteria Mouth 1010 Skin 1012 Intestines 1014 • May also vary at different sites on same tissue e.g. skin - approx 2 square meters - moist areas more densely populated Complex flora : > 200 species NORMAL HUMAN FLORA Skin – dominated by: • Staphylococcus epidermidis • Micrococcus sp. • Coryneforms (e.g. Propionibacterium acnes) • 20 – 30% individuals: Staphylococcus aureus Conjunctiva • Numbers usually low • Mostly S. epidermidis & certain coryneforms • Occasionally S. aureus, some streptococci, Neisseria sp., Haemophilus sp NORMAL HUMAN FLORA Oral cavity – multiple sp., including: • Oral streptococci (α – haemolytic) - S. salivarius, S. mutans, S. sanguis • Lactobacillus sp, Staphylococcus sp. • Corynebacterium sp. • Many anaerobes – esp. Bacteroides sp. Upper respiratory tract • Nares: S. epidermidis, Corynebacteria, S. aureus (20 – 30% individuals) • Nasopharynx: Mostly α-haemolytic streptococci other Streps., Neisseria sp., NORMAL HUMAN FLORA GI Tract – multiple sp., including for example: • Escherichia coli & other Enterobactericeae • Clostridium perfringens • Enterococcus faecalis • Bacteroides sp. Urogenital tract: • Antherior urethra: S. epidermidis, enteric bacteria • Vagina: various sp., including: Lactobacillus acidophilus Different types of symbiotic associations Commensalism Mutualism Harmless reciprocal benefit Parasitism unilateral benefit Factors controlling growth 4. Host defences – Innate and specific Dynamic, interactions with bacteria – outcome depends on the balance Host defences Bacterial virulence H Multiple factors B Multiple factors Pathogenicity usually a multifactorial process Normal flora - balance in a particular host niche, but not necessarily at other sites Virulence Quantitative – extent of ability to cause disease Completely avirulent Extremely virulent B H No capacity to survive in/on host H B Overwhelm defenses rapidly kills host Opportunistic pathogens Completely avirulent Extremely virulent B H Normal defences No disease H B Compromised defences Disease • Other sites are normally sterile, and the presence of bacteria suggests an infection: – Blood (septicaemia)s – Cerebrospinal fluid (meningitis) – Deep tissues (abscesses) • The digestive tract contains large numbers of organisms – up to 1/3 of faeces can be bacteria: some anaerobes are actually oxygen-sensitive • The vast majority of normal flora organism do not cause disease, but coexist with the host commensals • Much of the normal flora is actually beneficial to the host – they can exclude pathogen, by producing antibiotics, or other bactericidal substances (bacteriocins) • Removal of the normal flora by e.g. antibiotics can make the host much more susceptible to pathogenic organisms which would otherwise not cause disease because the normal flora will prevent them from colonising the host. Homework • Read about the Roles of Normal Flora – Brooks chapter 11 OR – Schaechter chapter 2