* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Reflex Hemodynamic Responses Initiated from the Thoracic Aorta
Electrocardiography wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Aortic stenosis wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
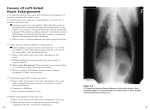
Reflex Hemodynamic Responses Initiated from the Thoracic Aorta By Franco Lioy, Alberto Malliani, Massimo Pagani, Giorgio Recordati, and Peter J. Schwartz ABSTRACT In anesthetized vagotomized cats with both carotid arteries occluded, stretch of the walls of the thoracic aorta performed without obstructing aortic blood flow induced reflex increases in arterial blood pressure (systolic: 136 ± 4 [SE] to 170 ± 7 mm Hg), heart rate (230 ± 10 to 236 ± 1 1 beats/min), and maximum rate of rise of left ventricular pressure (dP/dt max) (2,337 ± 256 to 3,155 ± 302 mm Hg/sec). In cats with spinal transection (C ( ), similar increases were observed. These responses were abolished by infiltrating the walls of the thoracic aorta with xylocaine. In adrenalectomized cats with intact central nervous systems, reflex responses were reduced but were still statistically significant. Phenoxybenzamine abolished the pressor response but not the increases in heart rate and dP/dt max. Propranolol drastically reduced the increases in heart rate and dP/dt max but not the pressor response. It is concluded that stretch of the thoracic aorta induced an increase in sympathetic activity affecting the heart, the peripheral vessels, and, probably, the adrenal glands through a spinal reflex. Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 KEY WORDS dP/dt max spinal cardiovascular reflexes adrenal glands vagotomy • Experimental evidence for spinal reflex mechanisms contributing to the neural control of circulation has been progressively growing (1-8). A definitive resolution of this debated question (9, 10) would result from identifying the cardiovascular receptors projecting to the spinal cord, the stimuli capable of affecting the receptors, the afferent and efferent nervous pathways, and the cardiovascular functions which represent the target of the reflexes. So far it has been proven that: (1) some cardiacsympathetic sensory endings are sensitive to specific hemodynamic events (6, 11), (2) natural hemodynamic stimuli in spinal vagotomized preparations reflexly modify the electrical discharge of sympathetic efferent fibers (6, 7), and (3) electrical or chemical stimulation of afferent cardiac sympathetic fibers produces reflex cardiovascular responses (12-14). It remains to be demonstrated that cardiovascular reflex responses can be induced by mechanical stimuli in spinal preparations. In our previous work on cardiocardiac reflexes (5, 6, 13-15), we could not find a mechanical stimulus that acted on the heart without directly affecting From the Istituto Ricerche Cardiovascolari, Universitii di Milano, Centro Ricerche Cardiovascolari CNR, 20122 Milano, Italy. Dr. Lioy was a Research Scholar, Canadian Heart Foundation, and CNR Visiting Professor, on leave from the Department of Physiology, University of British Columbia, Vancouver 8, B.C., Canada. Please address reprint requests to Dr. A. Malliani, Istituto Ricerche Cardiovascolari, Via F. Sforza 35, 20122 Milano, Italy. Received August 6, 1973. Accepted for publication October 25, 1973. 78 heart rate arterial blood pressure phenoxybenzamine propranolol carotid occlusion cats cardiac function. However, a recent observation that numerous sympathetic sensory endings can be functionally identified in the walls of the thoracic aorta (unpublished observations) seems to offer a possible solution to this problem. Therefore, we decided to stimulate these vascular endings mechanically to ascertain whether such a stimulus would produce reflex hemodynamic responses. This procedure demonstrated that a stretch of the thoracic aorta which did not interfere with aortic blood flow induced significant increases in arterial blood pressure, heart rate, and maximum rate of rise of left ventricular pressure (dP/dt max) in spinal vagotomized cats or vagotomized cats with intact central nervous systems. Methods Nineteen cats were anesthetized with chloralose and urethane (60 and 250 mg/kg, respectively, ip). In two cats sodium pentobarbital (35 mg/kg, ip) was used. The cervical vagi were cut, and then a carotid artery and a femoral artery were cannulated with short, wide-bore polyethylene catheters. After injection of a paralyzing dose of gallamine triethiodide, positive-pressure respiration was initiated using a Harvard respirator connected to a tracheal cannula. The respirator was adjusted to maintain arterial gases and pH (measured on an Astrup model RM 1304 blood acid-base analyzer) within physiological limits. The guidelines of the American Physiological Society regarding anesthetized, curarized animals were observed. In five cats the spinal cord was sectioned at Cx. In another five cats hydrocortisone (20 nig, iv) was administered, and the adrenal glands were removed through an abdominal midline laparotomy. Additional hydrocortisone (30 mg/hour) was then administered during the experiment by slow intravenous infusion. Circulation Research, Vol. XXXIV, January 1974 79 HEMODYNAMIC RESPONSES TO AORTIC STRETCH X c p ^» 4) j c^ CC CC +1 +1 2390 "^- 2691 «** in 3155 itricul : max 1_ « CO -H — d in c ss 00 o *« (N CN in -H •H •H o r- oo CM c O in © o c? d ss in n CM o <M — S •H _ o a """ c o o O 3 E (0 +1 CO — +1 oo ci in Ol in p q o d d 0) o o +1 CM .2 c _ ir> CO '•5 \s d oo "™ 1 Ol _ Ui _j CD +1 •H (N o ai jntricu )lic pr< nHg) a r- \s CO <N ati (0 o o 3 CO -H OO 0.01 Sti CB 01 X 2 CO Ol CO 0.05 ats/m CO 2 +i 0.005 tio c +1 (Si — +1 z +1 in CO oi CO TT <£> CD +1 M 4 •H +1 n CD Ol CC 1 cai Z3 •H CO 2 •y. in ue CO tt U a. ulectoi ion cord I CNS Groui •„ a. en O z c c a. ZJ > c = - •H V. >% rvou oo o :arot b z wer trial 6 z CO cj 1 tori -2 1 the vagi cut in i paired t-t Vi ro M in -* t~ (0 cv o a o ^, val ues .01 •A -5" centn ° J '6 CC occl nine d usi a E •H "c — 'c < •sP comn racic < o X G! ^s 0.01 i tid artery itoli c pressure 'i m -H o 131 o o 144 ± '•5 o o 113 CO n M i ^ 170 ± 0.001 O "5 to 136 CO 0) Stimulaltion oli E Con trol 1 Ca o u 105 V) +1 o o in 1— .001 1 Q. o 0.001 iS .00! o 0) >, 1UJj Circulation Research, VoL XXXIV. January 1974 a Ul) Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 All cats were placed on their right side, and the left hemithorax was widely opened from the fourth to the tenth rib. A special cannula was used to stretch the walls of the thoracic aorta without obstructing aortic blood flow. It consisted of a stainless steel tube surrounded by a thin rubber cylinder which could be inflated via another small metal tube mounted perpendicular to the tube close to one end of the cannula. The cat was heparinized (3 mg/kg), and, after clamping the aorta caudal to the left subclavian artery, the vessel was completely divided and the cannula inserted. Cannulas of different dimensions (5-7 cm long, 3-5 mm, i.d.) were selected according to the cat's size so that they fit snugly into the vessel. The two cut ends of the aorta were ligated around the lower end of the cannula, the side tube passing out between them. The cannulation procedure took between 1.5 and 2 minutes. The pressure drop across the cannula measured by comparing the carotid and femoral arterial mean pressures was between 5 and 15 mm Hg. When the balloon was inflated the aortic walls were stretched between the seventh and the tenth intercostal arteries. The pericardium was opened, and a short (7 cm) no. 7 cardiac catheter was introduced into the left ventricle via the left auricle and mitral valve. Recorded Variables.—Arterial pressures were measured with Statham P23De strain gauges. The cathetermanometer systems had a flat ( ± 5 % ) frequency response of 30 Hz as calculated by their responses to step increases in pressure (16). Left ventricular pressure was measured with a Statham P23De strain gauge connected to a specially built, high-frequency d-c operational bridge amplifier that was linear (-3 db) up to 15 kHz. The measured flat (±5%) frequency response of the left ventricular catheter-manometer system was 60 Hz, and the phase lag was linear up to 110 Hz. The left ventricular pressure signal was fed into an analog differentiator which was linear up to 160 Hz. An amplified record of left ventricular end-diastolic pressure was obtained using a Grass 7DAC driver amplifier. We also recorded the electrocardiogram (ECG), using a Grass 7P511 preamplifier, the heart rate, using a Grass 7P4C tachograph, and the respiratory movements, transduced by a crystal capsule connected to the side arm of the tracheal cannula. These variables and the blood pressures were registered on a multichannel inkwriting Grass P7 polygraph and simultaneously fed into a Hewlett-Packard 3907C tape recorder. Five of these variables could also be photographed by a Grass C4 camera from a Tektronix 565 oscilloscope. Data were collected only from cats that had a systolic blood pressure (carotid artery) above 100 mm Hg. Heart rate was measured from the ECG for each group of ten cardiac cycles during one control period (30-60 seconds) and during 30-60 seconds of stimulation (stretch of the aortic walls). As a check on the validity of the measurements of left ventricular dP/dt max, carotid and left ventricular pressures along with dP/dt were displayed at fast speed on the oscilloscope to establish that dP/dt max was always reached during the isovolumic phase of ventricular contraction. The control values and the maximum changes induced in each variable by stretch of the aortic walls were averaged for each cat, and the resulting values o Stim ula c _o 5 l - en VZ 80 LIOY, MALUANI, PAGANI, RECORDATI, SCHWARTZ Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 were used to compute the means ± SE presented in the tables. Results Cats with Intact Central Nervous Systems.—In eight vagotomized cats with both their common carotid arteries occluded, stretch of the walls of the thoracic aorta induced marked increases in systolic, diastolic, and pulse arterial pressures, left ventricular systolic pressure, and dP/dt max. Heart rate increased only a few beats per minute, and left ventricular end-diastolic pressure increased by less than 1 mm Hg. All these changes were statistically significant (Table 1). Figure 1A shows one of these experiments: blood pressures, left ventricular dP/ dt max, and heart rate rose soon after inflation of the balloon and remained elevated throughout the period of stimulation. These hemodynamic effects were not due to obstruction of the thoracic aortic blood flow caused by the experimental maneuver, since a parallel pressure increase was observed both above and below the cannula. In several experiments, as in the one presented in Figure 1A, a second late increase in blood pressure was recorded after the initial rise. When the balloon was deflated, aU variables decreased toward control levels, which were reached after different periods of time (30-230 seconds). These cardiovascular responses were much less evident if one common carotid artery was not oc- eluded, thus allowing the full operation of that baroreceptive area. Cats with Spinal Section.—In six vagotomized cats with their spinal cord sectioned at C,, the aortic stretch produced similar circulatory responses (Table 1). Figure 2 shows one of these experiments. All variables returned to control 30-120 seconds after cessation of the stimulus. Reflex Nature of the Response.—In four cats with intact central nervous systems and in one with spinal section, 1% xylocaine was infiltrated under the adventitia of that portion of the thoracic aorta which was stretched by the balloon. Table 2 shows the very significant reduction or abolition of all of the responses to aortic stretch induced by this procedure. The small decrease in dP/dt max shown in Table 2 was not due to the stimulus; it probably resulted from some absorption of the anesthetic into the bloodstream. After administration of xylocaine, however, the cat's reactivity was still perfectly preserved, as shown by the cardiovascular responses to a strong nociceptive stimulus (clamping of the paw). Light nociceptive stimuli did not elicit cardiovascular responses because of the level of anesthesia. These experiments showed that the effects of aortic stretch were initiated from receptors located in the aortic walls. Peripheral Mechanisms of the Reflex Responses.—To assess the contributions of cardiac and peripheral vascular mechanisms to the responses elicited by aortic stretch, adrenergic blockade and cardiac denervation were carried out in some cats. Propranolol (l mg/kg, iv) was injected over a period of 30 minutes in four cats with intact central nervous systems. Left ventricular dP/dt max and %V\ MR FIGURE 1 Effects of stretching the thoracic aorta in a vagotomized cat with an intact central nervous system and both common carotid arteries occluded. CAP - carotid artery pressure (recorded proximal to the point of occlusion), FAP —femoral artery pressure, LVP - left ventricular pressure (all in mm tig), LV dP/ dt — rate of change of left ventricular pressure (mm Hglsec), and HR — heart rate (beats/min). On the left of each section are fast-speed records of each variable. The aortic stretch in this and following figures is indicated by a bar. A: Control: B: After administration of propranolol (1 mg/kg, iv). HR FIGURE 2 30..C Effects of stretching the thoracic aorta in a vagotomized cat with spinal section (Ci). Abbreviations are the same as they are in Figure 1. A: Control. B: After administration of phenoxybenzamine hydrochloride (5 mg/kg, iv). Circulation Research, Vol. XXXIV, January 1974 81 HEMODYNAMIC RESPONSES TO AORTIC STRETCH Us co: E • ' E -H -H p tOM° n t- V 00 •H M oo O MB) O | *9 io <N ^3 m as a> cs X • <c o ° 00 -H q —' pop -H CO I S_ *w A 00 on u « 2 <, - I -D S 1 cs to CD d +( q n 5 o E d d An •H •H o d CD © in O d d d d -H +1 CD d d •5 1 .§ S3 ^ spom •H -H S -Hg t-; 1-^ d Bill) T3 .SP .S" c •*' o i m |x °^ i «s <: t q O5 V 0 S so c * < 1 v it I B E - ^2 5 BC 5 00 CO H & 2a. 1 -H +1 © 00 M <o o «= n ' © in oi m W TT W +1 -H p i— n ° in M ^ •H -H p | I O c cat Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 O (o c I X 1 gc, o >, Circulation Research, VoL XXXIV. January 1974 2 'c = £ —2 = 3 S a heart rate were decreased by the drug. Aortic stretch induced a smaller but clear increase in arterial and left ventricular pressures; heart rate remained constant, and left ventricular dP/dt max increased only very slightly and slowly during the period of stimulation (Fig. IB). After slow intravenous injection of phenoxybenzamine hydrochloride (5 mg/kg) in four spinal cats, the increase in systolic pressure induced by aortic stretch was drastically reduced; arterial diastolic pressure was somewhat decreased, and pulse pressure was increased. There were slight decreases in left ventricular end-diastolic pressure. The response of dP/dt max was not significantly altered, but heart rate increased much more than it did in the control period (Table 2). The cardiac effects (heart rate, dP/dt max) of the aortic stretch were prolonged and continued after cessation of the stimulus (Fig. 2B). Sympathetic denervation of the heart was performed in some cats by cutting the cardiac nerves or by bilateral stellectomy. Although the cardiac effects of aortic stretch were reduced, they could not be abolished by denervation. Since the residual effects could have been mediated by a reflex increase in catecholamine output from the adrenal glands, the experiments were repeated in a group of adrenalectomized cats. Adrenalectomized Cats.—After removal of the adrenal glands, the aortic stretch still induced all the described cardiovascular effects in five cats with intact central nervous systems (Table 1). The magnitude of the responses was smaller than it was in the cats with adrenal glands, although the difference was statistically significant only for the arterial pressure effects. The maximum changes were observed soon after the onset of the stimulus, and the late rise in blood pressure was never seen in this group of cats (Fig. 3). Moreover, when the balloon was deflated, all variables returned to control levels after short periods of time (4-15 seconds). In two of these cats, section of the left inferior cardiac nerve and the pericoronary nerve completely abolished the cardiac effects of the stimulation. It is therefore very likely that in cats with adrenal glands the residual cardiac effects of aortic stretch after cardiac denervation are due to a reflex increase in the adrenal output of catecholamines. Effect of an Afterload Increase on Left Ventricular dP/dt max. —In six cats, an increase in systolic arterial pressure comparable to that elicited by aortic wall distention was induced by 82 LIOY, MALLIANI, PAGANI, RECORDATI, SCHWARTZ r2OO CAP FAP LVP Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 HR 225 30 sec FIGURE 3 Effects of stretching the thoracic aorta in an adrenalectomized vagotomized cat with an intact central nervous system and both common carotid arteries occluded. Abbreviations are the same as they are in Figure 1. partially obstructing the aorta with a tourniquet. The average percent rise in dP/dt max obtained in this way (+12%) was much smaller than that induced by aortic stretch (+32%). This difference was statistically significant (P < 0.05V Effect of Different Anesthetics.—The reflex effects obtained in two cats anesthetized with sodium pentobarbital (one with an intact central nervous system and one with spinal cord section) were similar to those obtained in the other cats anesthetized with the chloralose-urethane mixture. Adequacy of the Stimulus. — All the cardiovascular responses that have been described were clearly evident with stretches that increased aortic diameter, measured with a precision caliper at the point of maximum distention, only 10%. This change in aortic radius was of the same magnitude as that observed when the mean pressure of the thoracic aorta was mechanically increased (aortic stenosis) 50-60 mm Hg. A similar extensibility of the aortic walls has been reported in the dog (17). The stimulus we used was therefore comparable to changes that can be observed in physiological situations. Discussion A mechanical stretch of the walls of the thoracic aorta induced significant increases in systemic arterial blood pressure, heart rate, and left ventricular dP/dt max. These cardiovascular responses were not due to some direct interference with aortic blood flow caused by the experimental maneuver; they represented neurally mediated phenomena, since they all disappeared after infiltration of the aortic walls with a local anesthetic. The same responses were present in spinal preparations, and, therefore, the integration of the reflex appears to take place in the spinal cord. It is probable that supraspinal baroreceptive mechanisms exert an inhibitory influence on these reflex responses, because the effects of aortic stretch were greatly attenuated unless both common carotid arteries were occluded in vagotomized cats with intact brains. Gruhzit et al. (18) have observed that a rise in aortic pressure, produced in dogs by intravenous injection of epinephrine, induces a reflex hind-limb vasodilatation initiated by receptors which are probably located in the thoracic aorta and mediated by spinal afferent pathways. It is difficult to compare their results with ours because of the differences in the stimuli and the preparations. Furthermore, the fact that we always observed a rise in arterial blood pressure does not rule out the possibility that some vasodilatation occurred in some vascular territories. Alpha-receptor blockade suppressed the rise in blood pressures induced by the aortic stretch but not the increase in heart rate and left ventricular dP/dt max. Actually a much larger increase in heart rate was observed after administration of phenoxybenzamine. This increase probably resulted from inhibition of norepinephrine reuptake or interference with catecholamine metabolism by the drug (19), which would result in greater availability of adrenergic transmitter for betastimulating effects. The decrease in arterial diastolic pressure observed under these conditions was presumably due to some beta-adrenergic (20) or sympathetic cholinergic (21) vasodilatation induced by the stimulus. Thus, the experiments with alpha-receptor blockade showed that the blood pressure increase was mainly due to peripheral vasoconstriction and that the rise in dP/dt max was largely independent of the increase in afterload and could actually occur even when aortic diastolic pressure decreased during stimulation (Fig. 2B). The modest influence of increases in afterload on dP/dt max was further proven by comparing the effects of similar rises in aortic pressure during Circulation Research. Vol. XXXIV. January 1974 83 HEMODYNAMIC RESPONSES TO AORTIC STRETCH Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 reflex responses and during mechanical constriction of the aorta (see Results). The administration of a beta-receptor blocking agent did not affect the increases in blood pressure but completely abolished the tachycardia and drastically reduced the increase in dP/dt max. The very small residual effect on dP/dt max probably depended mostly, if not exclusively, on the rise in afterload (22, 23). The validity of left ventricular dP/dt max as an index of myocardial contractility was supported in these experiments by the fact that its maximum value was always attained before the opening of the semilunar valves (23). However, before assuming that the increase in dP/dt max was the result of an increase in sympathetic discharge to the heart, other factors should be ruled out, i.e., changes in afterload, preload, heart rate, and circulating catecholamines (13, 22, 23). The role of afterload has already been discussed. The influence of changes in preload on dP/dt max (23) must have been minimum, since left ventricular end-diastolic pressure remained practically constant during aortic stretch. It also seems unlikely that the rise in dP/ dt max resulted primarily from a staircase phenomenon (23) caused by the simultaneously elicited tachycardia, because heart rate only increased a few beats per minute even though dP/ dt max increased much more substantially (in average 30% over control values). Another point that should be discussed is the contribution of the adrenal glands to the observed cardiovascular responses. On purely theoretical grounds, an increase in afferent nervous activity involving several spinal segments (T7-Ti0) in part corresponding to those from which the splanchnic nerves originate should reflexly stimulate adrenal secretion. This supposition was supported by the fact that the cardiac effects of aortic stretch could not be completely suppressed by cardiac denervation. This last observation contrasts with results found when cardiovascular responses are elicited through afferent cardiac sympathetic fibers projecting to higher segments of the spinal cord (13, 14). However, the persistence of all the reflex responses in adrenalectomized cats proved that they were only partly due to increased cateeholamine output from the adrenal glands. As predicted, in these cats cardiac denervation completely abolished the reflex increases in heart rate and dP/dt max. In conclusion, our experiments indicate the existence of spinal cardiovascular reflexes initiated by Circulation Research. VoL XXXIV, January 1974 mechanical stimuli acting on vascular sensory endings. We are not suggesting that the thoracic aorta represents another reflexogenic area in the classical sense: on the contrary, it is likely that nervous control of circulation is obtained through a variety of neural circuits (1, 3, 4) and that spinal reflexes represent diffuse, elementary mechanisms. The spinal reflex discussed in the present paper appears to operate by a positive feedback mechanism: a stimulus likely to duplicate the effects of an increase in aortic blood pressure produces a further increase in blood pressure, heart rate, and dP/dt max. Thus, the conception that nervous control of the circulation is exerted exclusively through negative feedback mechanisms seems to be in conflict with some of the experimental evidence. References 1. HEYMANS, C , BOUCKAERT. J.J., FARBER, S., AND HSU, F.Y.: Spinal vasomotor reflexes associated with variations in blood pressure. Am] Physiol 117:619-625, 1936. 2. GAMMON, CD., AND BRONK, D.W.: Discharge of impulses from pacinian corpuscles in the mesentery and its relation to vascular changes. Am J Physiol 114:77-84, 1935. 3. FERNANDEZ DE MOLINA, A., AND PERL, E.R.: Sympathetic ac- tivity and the systemic circulation in the spinal cat. J Physiol (Lond) 181:82-102, 1965. 4. BEACHAM, W.S., AND KUNZK, D.L.: Renal receptors evoking a spinal vasomotor reflex. J Physiol (Lond) 201:73-85, 1969. 5. MALLIANI, A., SCHWARTZ, P.J., AND ZANCHETTI, A.: Sym- pathetic reflex elicited by experimental coronary occlusion. Am J Physo 217:703-709. 1969. 6. BROWN, A.M., AND MALLIANI, A.: Spinal sympathetic reflexes initiated by coronary receptors. J Physiol (Lond) 212:685-705, 1971. 7. MALLIANI, A., PACANI, M., RECORDATI, C , AND SCHWARTZ, P.J.: Spinal sympathetic reflexes elicited by increases in arterial blood pressure. Am J Physiol 220:128-134, 1971. 8. ANDREWS, C.H., ANDREWS, W.H.H., AND ORBACH, J.: Sym- pathetic reflex elicited by distension of the mesenteric venous bed. J Physiol (Lond) 226:119-131, 1972. 9. SCHAEFFER, H.: Central control of cardiac function. Physiol Rev 40(suppl. 4):213-249, 1960. 10. FOLKOW. B., AND NEIL. E.: Circulation. London, Oxford University Press, 1971, p 583. 11. MALLIANI, A., RECORDATI, G., AND SCHWARTZ, P.J.: Nervous activity of afferent cardiac sympathetic fibres with atrial and ventricular endings. J Physiol (Lond) 229:457-469, 1973. 12. PETERSON, D.F., AND BROWN, A.M.: Pressor reflexes pro- duced by stimulation of afferent cardiac nerve fibers in the cardiac sympathetic nerves of the cat. Circ Res 28:605-610, 1971. 13. MALLIANI, A., PETERSON, D.F., BISHOP, V.S., AND BROWN, A.M.: Spinal sympathetic cardiocardiac reflexes. Circ Res 30:158-166, 1972. 84 14. LIOY, MALLIANI, PAGANI, RECORDATI, SCHWARTZ MALLIANI, A., PARKS, M., TUCKETT, R.P., AND BROWN, A.M.: 19. IVERSEN. L.L., AND LANGER. S.Z.: Effects of phenoxybenzamine on the uptake and metabolism of noradrenaline in the rat heart and vas deferens. Br J Pharmacol 37:627-637, 1969. 20. VIVEROS, O.H., GARLICK, D.G., AND RENKIN, E.M.: Sym- Reflex increases in heart rate elicited by stimulation of afferent cardiac sympathetic nerve fibers in the cat. Circ Res 32:9-14, 1973. 15. 16. 17. 18. SCHWARTZ, P.]., PACANI, M., LOMBARDI, F., MALLIANI, A., AND BROWN, A.M.: Cardiocardiac sympathovagal reflex in the cat. Circ Res 32:215-220, 1973. FRY, D.L.: Physiologic recording by modern instruments with particular reference to pressure recording. Physiol Rev 40:753-788, 1960. NICOLOSI, G.R., AND PIEPER, H.P.: Aortic smooth muscle responses to changes in venous return studied in intact dogs. Am J Physiol 221:1209-1216, 1971. GRUHZIT, C.G., FREYBURGER, W.A., AND MOE, G.K.: Nature of the reflex vasodilatation induced by epinephrine. J Pharmacol Exp Ther 112:138-150, 1954. pathetic beta adrenergic vasodilatation in skeletal muscle of the dog. Am J Physiol 215:1218-1225, 1968. 21. UVNAS, B.: Sympathetic vasodilator system and blood flow. Physiol Rev40(suppl.4):69-76, 1960. 22. GLEASON, W.L., AND BRAUNWALD, E.: Studies on the first derivative of the ventricular pressure pulse in man. J Clin Invest 41:80-91, 1962. 23. FURNIVAL, CM., LINDEN, R.J., AND SNOW, H.M.: Inotropic changes in the left ventricle: Effect of changes in heart rate, aortic pressure and end-diastolic pressure. J Physiol (Lond) 211:359-387, 1970. Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 Circulation Research, Vol. XXXIV, January 1974 Reflex Hemodynamic Responses Initiated from the Thoracic Aorta FRANCO LIOY, ALBERTO MALLIANI, MASSIMO PAGANI, GIORGIO RECORDATI and PETER J. SCHWARTZ Downloaded from http://circres.ahajournals.org/ by guest on May 7, 2017 Circ Res. 1974;34:78-84 doi: 10.1161/01.RES.34.1.78 Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1974 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7330. Online ISSN: 1524-4571 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circres.ahajournals.org/content/34/1/78 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation Research is online at: http://circres.ahajournals.org//subscriptions/