* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Jones Handouts [Compatibility Mode]
Survey
Document related concepts
Transcript
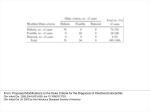
10/9/2012 I have no conflicts of interest in relation to this program Whitney Jones, PharmD Antimicrobial Stewardship Pharmacist Vanderbilt University Medical Center October 25, 2012 Understand the epidemiology associated with gramnegative resistance Discuss changing trends in resistance to antimicrobials Recognize current challenges in infectious diseases pharmacotherapy Understand the goals of antimicrobial stewardship programs and the role pharmacists may play in optimizing the use of antimicrobials Unprecedented success of antibiotics in 1960s “[It] is time to close the book on infectious diseases and declare the war against pestilence won” - US Surgeon General William H. Stewart Infectious diseases are #1 cause of mortality worldwide 3rd most common reason for hospitalization in U.S. Dellit TH. Clin Infect Dis 2007;44:159-77. www.who.int. Accessed September 12, 2012. Widespread use of antibiotics inevitably leads to resistance Definition Acquired ability of a pathogen to withstand an antibiotic that kills off its sensitive counterparts Multidrug-resistant (MDR) bacteria No consensus definition > 3 antimicrobial classes ~ 70% of bacteria causing hospital-acquired infections are resistant to > 1 antibiotic 89% of A. baumannii isolates www.cdc.gov. Accessed September 12, 2012. Rice LB. J Infect Dis 2008;197:1079-81. Pandrug Resistant Extensively Drug Resistant Antipseudomonal cephalosporins Resistant Resistant Antipseudomonal carbapenems Susceptible Resistant Piperacillin/ tazobactam Resistant Resistant Ciprofloxacin Levofloxacin Resistant Resistant Ticarcillin/ clavulanate Resistant Resistant Aminoglycosides Susceptible Resistant resistant to > 3 antibiotic classes Gaynes R. Clin Infect Dis 2005;41:848-54. 1 10/9/2012 E cloacae (n = 704) K pneumoniae non-ESBL (n = 931) K pneumoniae ESBL (n = 78) P aeruginosa (n = 1,054) A baumannii (n = 486) P-T 81 93 41 90 50 TAZ 72 93 3 82 44 CFP 95 96 44 78 43 MER 99 98 69 84 64 AMK 99 98 73 96 72 LVX 90 94 23 65 42 MIN 80 85 53 5 81 TIG 96 96 90 NA* NA† Data are % susceptible. ESBL = extended-spectrum β-lactamase; P-T = piperacillin-tazobactam; TAZ = ceftazidime; CFP = cefepime; MER = meropenem; AMK = amikacin; LVX = levofloxacin; MIN = minocycline; TIG = tigecycline. P-T = piperacillin-tazobactam; TAZ = ceftazidime; IMP = imipenem; TOB = tobramycin; CIP = ciprofloxacin. Rhomberg PR, et al. Diagn Microbiol Infect Dis. 2009;65:414-26. Dowzicky MJ, et al. Clin Ther. 2008;30:2040-2050. Financial impact in U.S. $21 – 34 billion spent annually > 8 million additional hospital days Outcome OR (95% CI) P Length of stay 1.56 0.001 Cost of hospitalization 1.57 0.003 Clinical impact P-T = piperacillin-tazobactam; TAZ = ceftazidime; IMP = imipenem; TOB = tobramycin; CIP = ciprofloxacin. Rhomberg PR, et al. Diagn Microbiol Infect Dis. 2009;65:414-26. Schwater MJ. Antimicrob Agents Chemother 2006;50:1287-62. ESBL production associated with increased mortality Organism Resistant to Mortality LOS Enterobacter 3rd-generation cephalosporins 5.02 (1.10–22.9) 1.47 (1.25–1.72) P aeruginosa imipenem 1.94 (1.22–3.10) 15.5 vs 9 days* (P = .02) Acinetobacter MDR 2.6 (0.3–26.1) 2.5 (1.2–5.2) * Mean LOS post-culture Schwaber MJ, et al. J Antimicrob Chemother. 2007;60:913-920. Cosgrove SE, et al. Arch Intern Med. 2002;162:185-190. Lautenbach E, et al. Infect Control Hosp Epidemiol. 2006;27:893-900. Sunenshine RH, et al. Emerg Infect Dis. 2007;13:97-103. 2 10/9/2012 Ahead of the curve 3.5 billions years to adapt Genetic plasticity Rapid replication ▪ 20 – 30 minutes to replicate Gram-negative pathogens Possess features of particular concern ▪ Highly efficient up-regulation or acquisition of genes that code for resistance mechanisms ▪ Plethora of resistance mechanisms Multiple mechanisms at once Single mechanism may affect multiple antibiotics Inactivating Enzyme Altered Target Decreased Permeability Efflux β-Lactams ++ + + + Aminoglycosides ++ + + + Fluoroquinolones + ++ + + Sulfonamides ++ Trimethoprim ++ + Tetracyclines + + ++ + ++ Tigecycline Polymyxins Changes in or protection of target Binding site mutations in topoisomerase II and IV ▪ Most common for fluoroquinolones Overproduction of the target ++ ++: most common mechanism +: other mechanism Adapted from: Opal SM. Mandell, Douglas, and Bennett’s Principles and Practices of Infectious Diseases. 7th ed. Philadelphia, PA: Churchill Livingstone Elsevier;2010:279-95. Drug- or class-specific efflux pumps May recognize broad range of agents ▪ MexAB-OprM pump: meropenem, fluoroquinolones, tetracyclines and tigecycline ▪ AcrAB-ToIC pump: fluoroquinolones, ampicillin, tigecycline, macrolides and oxazolidinones ▪ MexXY-OprM pump: adaptive resistance to aminoglycosides in P. aeruginosa Loss of outer membrane proteins Nicasio AM, et al. Pharmacotherapy. 2008;28:235-249. One of most common mechanisms Aminoglycoside-modifying enzymes Acetyltransferases Adenyltransferases phosphoryltransferases β-lactamase production OprD: imipenem resistance Nicasio AM, et al. Pharmacotherapy. 2008;28:235-249. Poole K. J Antimicrob Chemother. 2005;56:20-51. 3 10/9/2012 Amber classification Class A β-Lactamases penicillinases Amino Acid serine B zinc C metallo-βlactamases cephalosporinases Examples TEM, SHV, KPC, CTX-M IMP, VIM serine AmpC D oxacillinases serine OXA Commonly found in Enterobacteriaceae Confer resistance to penicillins, cephalosporins and aztreonam Cephamycins, cefepime and piperacillin-tazobactam may appear susceptible Revised susceptibility breakpoints Additional plasmid-mediated resistance Aminoglycosides and fluoroquinolones Carbapenems Drugs of choice Resistant to ESBL hydrolysis Nicasio AM, et al. Pharmacotherapy. 2008;28:235-249. Chromosomal production Common bacteria Broad terminology Ambler Class Enterobacter Citrobacter Serratia marcescens A. baumannii P. aeruginosa Class B ▪ Selection following β-lactam exposure ▪ Primarily 3rd generation cephalosporins Nicasio AM, et al. Pharmacotherapy. 2008;28:235-249. Jacoby GA, et al. N Engl J Med. 2005;352:380-391. Paterson DL, et al. Clin Microbiol Rev. 2005;18:657-686. Mushtaq S, et al. Antimicrob Agents Chemother. 2004;48:1313-1319. A D Confer resistance to penicillins, cephalosporins and aztreonam Generally including β-lactamase inhibitor combinations and cephamycins Possible resistance to cefepime and carbapenems β-Lactamases metallo-βlactamases Serine carbapenemases Examples IMP, VIM, SPM oxacillinases OXA, PSE KPC, IMI, SME Carbapenem-resistant Enterobacteriaceae Klebsiella pneumoniae carbapenemases (KPC) Jacoby GA. Clin Microbiol Rev. 2009;22:161-182. Livermore DM, et al. Trends Microbiol. 2006;14:413-420. Chow JW. Ann Intern Med 1991;115:585-90. Resistant to carbapenems, antipseudomonal cephalosporins and antipseudomonal penicillins Increased MICs, usually requiring additional First identified in 1996 in North Carolina Widespread mechanism (e.g. porin loss) to become fully resistant Aztreonam May resist hydrolysis by carbapenemases Poor clinical efficacy 4 10/9/2012 First reported in India (2006) Plasmid mediated Among the most significant multidrug-resistant (MDR) pathogens in hospitals Enterococcus faecium Staphylococcus aureus Klebsiella pneumoniae Easily transferrable Associated bacteria K. pneumoniae E. coli E. cloacae Acinetobacter baumanni Pseudomonas aeruginosa Enterobacter species Susceptible to colistin and tigecycline Colistin-resistant isolated detected Rice LB. J Infect Dis. 2008;197:1079-1081. Boucher HW, et al. Clin Infect Dis. 2009;48:1-12. CB is a 56 year old WF who presents to ED Chief complaint Culture results Many Enterobacter aerogenes Dyspnea and cough with nonpurulent sputum Afebrile WBC 6K PMH: COPD, DM, HTN, hypothyroidism Admitted to pulmonary internal medicine floor for management of COPD exacerbation Physical exam Cellulitis of LLE - erythematous, warm to touch and weeping Medical resident plans to order ceftriaxone Is this appropriate given the potential mechanisms of resistance? BB, an 78 yo AAM, presents to ED CC: fever and chills x 24 hrs SH: lives with son in Lexington, SC PMH: type II diabetes, CKD, HTN, obesity, recurrent UTIs ▪ Patient started on vancomycin and purulent fluid collected for culture…. Severity of illness Prolonged hospital length of stay (LOS) Prolonged intensive care unit (ICU) LOS Transfer from another hospital or nursing home Invasive procedure or device Immunocompromise Prior antibiotic therapy Safdar N, et al. Ann Intern Med. 2002;136:834-844. Maragakis LL, et al. Clin Infect Dis. 2008;46:1254-1263. Virk A, et al. Mayo Clin Proc. 2000;75:200-214. 5 10/9/2012 CXR – no infiltrates seen UA – cloudy, positive nitrite/leukocytes, TNTC bacteria Blood, urine and sputum cultures obtained Blood cultures Lactose-fermenting gram-negative bacilli (2 of 2) $400 - $800 million per approved agent Lower return on investment Short course therapy Need to limit use of new, broad-spectrum antibiotics ▪ Decreased efficacy with increased use Lack of available research guidance DiMassa JA. J Health Econ 2003;22:151-85. Projan SJ. Curr Opin Microbiol 2003;6:427-30. Spellberg B. Clin Infect Dis 2008;46:155-64. Boucher HW, et al. Clin Infect Dis 2009; 48: 1-12. Patient and clinician education Infection control Antimicrobial stewardship Multifaceted approach ▪ Limit inappropriate use of antimicrobials ▪ Optimize selection, dose, route, and duration ▪ Limit emergence of resistance, adverse drug reactions and minimize cost McDonald LC, et al. Clin Infect Dis 2006; 42: S65-71. Dellit TH, et al. Clin Infect Dis 2007; 44: 159-77. 6 10/9/2012 Education Prospective audit and feedback Medical/pharmacy staff education Multidisciplinary approach Antimicrobial Support Teams ▪ ▪ ▪ ▪ Pharmacy Infectious Diseases physicians Microbiology Hospital Epidemiology Surveillance of resistance and antibiotic use Management of antibiotic use Prospective audit and feedback Institution of antibiotic restrictions Therapeutic substitutions Automatic stops Antimicrobial order forms Antibiotic dose optimization Extended infusions Pharmacokinetic services provided “The struggle against antibiotic resistance is a war we will never win. The strength of trillions upon trillions of microorganisms, combined with the ancient force of evolution by constant, unrelenting variation, will inevitably overpower our drugs” by pharmacists Bug-drug mismatch Sterile site list review Review of antibiograms -American Academy of Microbiology ▪ Institutional vs. location-specific Whitney Jones, PharmD Antimicrobial Stewardship Pharmacist Vanderbilt University Medical Center October 25, 2012 7