* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download High Morbidity and Mortality in Adults Hospitalized for Respiratory
Survey
Document related concepts
Oesophagostomum wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Hepatitis C wikipedia , lookup
West Nile fever wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Henipavirus wikipedia , lookup
Hepatitis B wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Transcript
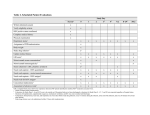
Clinical Infectious Diseases Advance Access published August 13, 2013 MAJOR ARTICLE High Morbidity and Mortality in Adults Hospitalized for Respiratory Syncytial Virus Infections N. Lee,1,2 G. C. Y. Lui,1 K. T. Wong,3 T. C. M. Li,1 E. C. M. Tse,1 J. Y. C. Chan,4 J. Yu,3 S. S. M. Wong,3 K. W. Choi,1 R. Y. K. Wong,1 K. L. K. Ngai,5 D. S. C. Hui,1,2 and P. K. S. Chan2,5 1 Department of Medicine and Therapeutics, 2Stanley Ho Center for Emerging Infectious Diseases, 3Department of Radiology and Organ Imaging, The Jockey Club School of Public Health and Primary Care, and 5Department of Microbiology, Chinese University of Hong Kong, Hong Kong Special Administrative Region, China 4 Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 Background. Better understanding of complications and outcomes of adults hospitalized with respiratory syncytial virus (RSV) infection is necessary. Methods. A retrospective cohort study was conducted on all adults (≥18 years) admitted to 3 acute care general hospitals in Hong Kong with virologically confirmed RSV infection during 2009–2011 (N = 607). Adults hospitalized for seasonal influenza during the period were used for comparison (n = 547). Both infections were prospectively diagnosed following a standard protocol. Independent reviews of chest radiographs were performed by radiologists. Main outcome measures were all-cause death, respiratory failure requiring ventilatory support, and hospitalization duration. Cox proportional hazards models were used for analyses. Results. The mean age of RSV patients was 75 (SD, 16) years; 87% had underlying conditions. Lower respiratory and cardiovascular complications were diagnosed in 71.9% (pneumonia, 42.3%; acute bronchitis, 21.9%; chronic obstructive pulmonary disease/asthma exacerbation, 27.3%) and 14.3% of patients, respectively; 12.5% had bacterial superinfections. Supplemental oxygen and ventilatory support were required in 67.9% and 11.1%, respectively. Crude all-cause mortality was 9.1% and 11.9% within 30 days and 60 days, respectively; mean length of stay of survivors was 12 (SD, 13) days. Advanced age, radiographic pneumonia, requirement for ventilation, bacterial superinfection, and elevated urea level and white blood cell count were independently associated with poorer survival. Systemic corticosteroid use was associated with longer hospitalization and secondary infections. The overall outcomes of survival and length of stay were not significantly different from those in influenza. Conclusions. RSV can cause severe lower respiratory complications in older adults, resulting in respiratory failure, prolonged hospitalization, and high mortality similar to seasonal influenza. Corticosteroids did not seem to improve outcomes. The unmet need for antiviral therapy and vaccination against RSV in adults should be promptly addressed. Keywords. RSV; hospitalization; respiratory failure; lower respiratory tract infection; adults. Respiratory syncytial virus (RSV) is known to be an important cause of lower respiratory tract infection in Received 23 March 2013; accepted 8 June 2013. Correspondence: N. Lee, MD, Chinese University of Hong Kong, 9/F Clinical Sciences Bldg, Prince of Wales Hospital, Shatin, Hong Kong, SAR (leelsn@cuhk. edu.hk). Clinical Infectious Diseases © The Author 2013. Published by Oxford University Press on behalf of the Infectious Diseases Society of America. All rights reserved. For Permissions, please e-mail: [email protected]. DOI: 10.1093/cid/cit471 infants and young children, leading to hospitalizations and deaths [1]. Its impact in adults, however, has only been appreciated in recent years. It has been estimated that RSV infects 3%–10% of adults annually; although most infections are mild, increasing evidence suggests that severe lower respiratory tract infections can occur, especially among older adults and those with underlying conditions [2–4]. RSV may have accounted for 5%–15% of community-acquired pneumonia, 9%–10% of hospital admissions for acute cardiorespiratory diseases, and excessive deaths during seasonal peaks [3, 4]. The disease Outcomes of Hospitalized Adults With RSV • CID • 1 METHODS Study Population and Case Finding Procedures A retrospective cohort study on hospitalized adults with RSV infections was conducted. All patients aged ≥18 years admitted to 1 of the 3 participating medical units between 1 January 2009 and 31 December 2011 (ie, 36 months) with laboratoryconfirmed RSV infections were studied (N = 607). In Hong Kong, peak RSV activities occur in spring or summer, or both, with yearly variations [12, 13]. No case was excluded from the analysis. All 3 participating hospitals (A, B, and C) are acute care, general public hospitals operating under the Hospital Authority of Hong Kong. The 3 hospitals serve an urban population of >1.5 million accounting for >20% of the population in Hong Kong [14, 15]. The Hospital Authority is the main provider of acute medical care in Hong Kong. Ethical approval for the study was obtained from the institutional review boards of the Hospital Authority of Hong Kong and the Chinese University of Hong Kong. During the study period, respiratory viral infections including RSV and influenza in the hospitalized adults were prospectively diagnosed according to a standard protocol as part of patients’ routine care, as previously described [14–16]. In brief, patients presenting with symptoms of acute respiratory infections were admitted if they developed potentially serious medical conditions and/or if their exacerbation of chronic illnesses or their severe symptoms were considered to be impossible to be managed at home [14, 16]. Nasopharyngeal aspirates (NPAs) were collected at presentation from all such patients, regardless of perceived etiology and disease severity, to test for RSV and influenza antigens using an immunofluorescence assay (see next section) [4, 12, 14–16]. In a minority of cases where NPA cannot be performed, nasopharyngeal flocked 2 • CID • Lee et al swabs were collected for testing. Test results were generally made available to physicians within a few hours to assist patient management and infection control precautions. In addition, chest radiography was performed at admission for all patients, and sputum samples were routinely collected for bacterial culture. Blood cultures were also performed when there were signs of sepsis [14–16]. Data Collection and Definitions of Variables All patients with laboratory-confirmed RSV infections admitted during the study period were identified from a computerized laboratory record system. Patients’ electronic (hospital Clinical Management System [CMS]) and written records were reviewed, and the clinical and laboratory information was systematically recorded using a standardized research tool [14– 16]. Clinical data collected included demographics, comorbidities, illness onset time, presenting symptoms, cardiorespiratory complications, requirement for supplemental oxygen therapy and/or ventilatory support, antibiotic use, use of systemic corticosteroids (eg, intravenous hydrocortisone, oral prednisolone), hospitalization duration, and all-cause death. Laboratory data included routine blood test results and bacterial pathogens cultured from respiratory and/or blood samples at presentation and during hospitalization [14]. Pneumonia was defined as physician-diagnosed pneumonia based on symptoms and signs of acute lower respiratory tract infection together with new pulmonary infiltrates on a patient’s chest radiographs [5, 14–17]. Acute respiratory failure requiring ventilatory support was defined as persistent respiratory failure despite supplemental oxygen therapy (eg, SaO2 <92%) which necessitated the use of noninvasive positive pressure ventilation (NIPPV) or invasive mechanical ventilation for support [14, 15]. The main outcome measure in this analysis was all-cause death; the secondary outcome measures were (1) development of acute respiratory failure requiring ventilatory support and (2) total duration of hospitalization among survivors [14, 15]. In addition, we compared the RSV patients with a cohort of patients admitted to these hospitals for seasonal influenza in 2009–2011 [14, 15]. The same research tools and definitions were used for both study cohorts. Patients hospitalized with pandemic 2009 H1N1 infections were not included for comparison as they were significantly younger and shown to have a different clinical course compared to seasonal influenza, as described elsewhere [15]. Virological Investigations All NPAs collected were subjected to viral antigen detection for a panel of respiratory viruses including RSV, influenza A and B, and parainfluenza 1, 2, and 3 viruses using an immunofluorescence assay (IFA) as previously described [14–16]. NPA contained more abundant epithelial cells for immunofluorescence staining; false-positive results are rare (see Discussion) [3, 4, 12, 18–20]. Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 burden of RSV can approach that of influenza [3, 5–8]. However, except, perhaps, in the profoundly immunosuppressed, little is known about the clinical manifestations, complications, and outcomes of severe RSV infections in adults. Factors associated with severe and fatal infections are largely unknown. Data from Asian countries are particularly scarce [9–12]. This study examined a large cohort of adults hospitalized with laboratory-confirmed RSV infections in Hong Kong, China. Clinical, laboratory, and radiological findings were reported and analyzed to identify factors associated with pneumonia development, respiratory failure, and death. Their severity of illness and outcomes were compared with patients admitted for seasonal influenza during the same period. Such information, when available, not only improves our understanding on severe RSV disease in adults and its impact on the healthcare system, but also provides valuable data to support future planning of clinical trials on RSV therapeutics and prevention. In brief, NPA samples were washed with phosphate-buffered saline. The cells were fixed on the wells of a glass slide with acetone and stained with respiratory virus–specific antibodies (LIGHT DIAGNOSTICS Respiratory Syncytial Virus FITC Reagent, Chemicon/Millipore). Specific fluorescent signals were cross-checked by 2 experienced technicians and reviewed by clinical virologists. A repeat sample would be requested if necessary. Virus isolation was performed for all influenza cases using methods previously described (but not routinely for RSV because of its low sensitivity and logistic demands) [4, 16, 12]. performed for the whole cohort, and repeated in the subgroup with additional radiographic reviews performed. We also compared the manifestations and outcomes of RSV patients to a concurrent seasonal influenza cohort using similar analytic methods [14, 15]. All probabilities were 2-tailed, and a P value of <.05 was considered to indicate statistical significance. We also calculated a conservative, Bonferroni-adjusted P value threshold (P < .002) for the multiple comparisons in Table 1 for reference. Statistical analysis was performed using PASW Statistics software, version 18.0. Radiographic Assessment RESULTS Statistical Analysis The Student t, Mann-Whitney U, and χ2 tests with continuity correction were used for univariate comparisons whenever appropriate. Variables with P values < .1 in the univariate analyses were entered into multivariate Cox proportional hazards models (backward, stepwise regression) to determine independent factors associated with death that occurred within 30 days and 60 days from time of hospitalization [6, 8, 14, 15]. Variables including demographics, comorbidities, cardiorespiratory complications, ventilation requirement, bacterial superinfection, and corticosteroid use were examined. Adjusted hazard ratios (AHRs) and 95% confidence intervals (CIs) were calculated for each explanatory variable. An AHR >1 indicated a higher chance of death. A Kaplan-Meier curve was constructed to show survival of patients with or without pneumonia development, and compared using the log-rank test. Cox regression models were also used to determine independent factors associated with time to hospital discharge. Multivariate logistic regression was used to analyze factors associated with pneumonia and acute respiratory failure requiring ventilatory support; adjusted odds ratios (AORs) and 95% CIs were reported for explanatory variables [14–16]. Analyses of clinical outcomes were Patient Descriptions and Clinical Manifestations During the 3-year study period, a total of 607 RSV cases were diagnosed among the hospitalized adults: 2009, n = 123; 2010, n = 237; 2011, n = 247. The median RSV-positive rate among submitted respiratory samples during the seasonal peaks of the years was: 5.8% (interquartile range [IQR], 4.8%–6.5%), 6.6% (IQR, 5.8%–9.8%), and 9.1% (IQR, 5.7%–13.7%), respectively (Figure 1). Patients’ baseline characteristics and clinical manifestations are described in Table 1. The mean and median ages were 75 (SD, 16) years and 80 (IQR, 68–86) years, respectively; 87.3% had 1 or more coexisting medical conditions (eg, chronic lung diseases, 35.6%, major systemic comorbidities, 74.0%; immunocompromised, 13.7%; see Table 1). The mean and median time of admission from symptom onset was 2.6 (SD, 2.2) days and 2 (IQR, 1–3) days, respectively. Fever (75.0%), cough (87.5%), sputum production (81.2%), and wheezy breathing and dyspnea (68.9%) were the commonest presenting symptoms. One or more complications were documented in 80.4%. Lower respiratory tract complications were diagnosed in 71.9%, including pneumonia (42.3%), acute bronchitis (21.9%), and exacerbation of chronic obstructive pulmonary disease (COPD)/asthma (with or without pneumonia, 27.3%). Bacterial superinfection was evidenced in 12.5% at presentation; Streptococcus pneumoniae, Haemophilus influenzae, and Pseudomonas aeruginosa were the commonest isolates (Table 1). Cardiovascular complications (eg, exacerbation of heart failure, acute coronary events) were diagnosed in 14.3% of patients. Among the subset of patients with additional radiographic review performed, 141 of 286 (49.3%) had shown active pneumonic changes; consolidations (23.8%) and ground-glass opacities (19.9%) were the commonest findings. Most (81.8%) changes were unilateral. Examples of patients’ chest radiographs at presentation are shown in Figure 2. Symptoms associated with radiographic pneumonia included fever (82.0% pneumonia vs 72.5% without pneumonia, P = .058) and wheezy breathing and dyspnea (79.9% vs 66.2%, P = .010). Runny nose (23.7% vs 35.2%, P = .035) and sore throat (9.4% vs 16.2%, P = .086) were less common. Multivariate analysis showed that presence of Outcomes of Hospitalized Adults With RSV • CID • 3 Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 To further characterize RSV-related lower respiratory tract complications and their impacts in adults, additional, detailed radiographic review was performed for all RSV cases admitted to the largest study site (hospital A, n = 286; 47% of the entire cohort). The chest radiographs at admission were reviewed by 2 independent, experienced radiologists using dedicated Picture Archiving and Communication System workstations in retrospect; images were interpreted in consensus for the few discrepant cases [21–23]. The reviewers were blinded to all clinical information of patients and their outcomes. Previous chest radiographs were used for comparison whenever available (86%). The chest radiographs were assessed for the presence of any active lung parenchymal changes (including consolidation, ground glass opacity, and reticulonodular shadows) that were compatible with the diagnosis of pneumonia, and their patterns and extent [22, 23]. Radiologists’ reviews were considered final. Table 1. Baseline Characteristics, Presenting Symptoms, Complications, and Outcomes of 607 Adults Hospitalized With Respiratory Syncytial Virus Infection, 2009–2011 Variable RSV (N = 607) Influenza (N = 547) P Value Age, y, mean (SD) 75.1 (16.4) 74.7 (16.6) .650 Male sex Resident of long-term care facility 48.6 32.9 49.5 30.5 .749 .378 Comorbidity, major systemic (except chronic lung diseases)a 74.0 65.8 Chronic lung diseasesa Symptom onset to admission, d, mean (SD) 35.6 2.6 (2.2) 24.1 2.0 (1.7) <.001 <.001 .003 Fever >37.5°C 75.0 94.2 <.001 Cough Sputum production 87.5 81.2 85.7 72.5 .513 .010 68.9 53.2 <.001 Sore throat Runny nose 11.8 25.6 14.3 30.2 .364 .214 Pneumonia 42.3 36.7 .006 Lower respiratory complicationsb Cardiovascular complicationsb 71.9 14.3 55.6 13.3 <.001 .653 Complications, anyb 80.4 72.8 .002 Bacterial infection, overallc Bacterial infection, at presentationc 14.8 12.5 14.3 9.1 .790 .066 Supplemental oxygen therapy 67.9 59.0 .002 Ventilation, noninvasive or invasive 30-day mortality 11.1 9.1 6.2 8.0 .003 .538 60-day mortality 11.9 8.8 .086 Time to death, d, median (IQR) Extended care in subacute hospitals 13 (7–29) 25.2 7 (3–13) 19.7 .001 .027 7 (5–14) 6 (5–11) .238 Duration of hospitalization for survivors, d, median (IQR) Data are percentages unless otherwise indicated. Patients hospitalized with seasonal influenza during the same period are used for comparison. RSV cohort: hospital A, 47.4%; B, 32.5%; C, 20.1%; never-smoker, 43.7%; (non-Chinese, 1; pregnant female, 1). Specimen for diagnosis: nasopharyngeal aspirate, 90.6%; nasopharyngeal flocked swabs, 9.1%; bronchial/tracheal aspirates, 0.3%. Seasonal influenza cohort: H3N2, 79.2%; H1N1, 0.7%; B, 20.1%; >95% immunofluorescence assay positive (nearly all confirmed with culture; remainder diagnosed by culture/polymerase chain reaction); 91.2% received oseltamivir treatment [14–16]. Two patients had RSV and influenza A coinfection. A Bonferroni-corrected P value significance threshold (P < .002) is calculated for reference. Abbreviations: IQR, interquartile range; RSV, respiratory syncytial virus; SD, standard deviation. a Major systemic comorbidity: congestive heart failure; cerebrovascular, neoplastic, and chronic liver or renal diseases; other chronic cardiovascular and neurologic conditions (except hypertension); diabetes mellitus; autoimmune disorders; immunocompromised (immunocompromising conditions and/or use of immunosuppressants). Chronic lung diseases: chronic obstructive pulmonary disease, asthma, bronchiectasis, and pulmonary fibrosis [14–16]. b Lower respiratory complications: pneumonia, acute bronchitis, acute exacerbation of chronic obstructive pulmonary disease/asthma. Cardiovascular complications: exacerbation of heart failure, atrial fibrillation, acute coronary events, acute cerebrovascular events. Other complications: drowsiness, delirium, seizure (6.1%); syncope, fall, renal impairment, dehydration, metabolic disturbances (15.9%). Patients may have >1 complication [14–16]. c Bacterial superinfection: evidenced by positive culture of a bacterial pathogen from respiratory (sputum, bronchial/tracheal aspirates) and/or blood samples; infections with onset >2 days after admission were considered hospital-acquired [14, 15]. At presentation: Streptococcus pneumoniae, 15; Haemophilus influenzae, 14; Staphylococcus aureus, 5; Moraxella catarrhalis, 2; Pseudomonas aeruginosa, 20; Klebsiella spp, 10; other gram-negative bacteria, 9; other gram-positive cocci, 1. Hospital-acquired: P. aeruginosa, 5; other gram-negative bacteria, 9. Most (94.7%) patients received antibiotic treatment. major systemic comorbidities (AOR, 1.85; 95% CI, 1.05–3.26) and elevated white blood cell counts (AOR, 1.07; 95% CI, 1.01– 1.13, per unit increase) were independently associated with radiographic pneumonia, adjusted for demographic and bacteriological variables (Supplementary Data 1). Patient Management and Outcomes Systemic corticosteroids were given to 38.9% of patients to treat acute airway diseases (eg, COPD/asthma exacerbations), and 4 • CID • Lee et al antibiotics were used in 94.7% of cases. Two-thirds (67.9%) of patients were given supplemental oxygen therapy; 11.1% developed persistent respiratory failure and required ventilatory support (NIPPV, 9.1%, invasive ventilation, 2.0%). Underlying chronic lung diseases, pneumonia ( particularly the presence of ground-glass opacities), and elevated serum urea and alanine aminotransferase levels were shown to be independent factors associated with requirement of ventilatory support (Table 2). Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 Wheezy breathing and dyspnea The crude all-cause mortality within 30 days and 60 days of this RSV cohort was 9.1% (n = 55) and 11.9% (n = 72), respectively. The median time to death was 13 (IQR, 7–29) days after admission (90th percentile, 45 days). The reported direct causes of death were pneumonia (n = 48), COPD exacerbation (n = 5), acute cardiovascular events (n = 12), and underlying medical conditions complicated by pneumonia/sepsis (n = 7) Comparisons With Seasonal Influenza When patients with RSV were compared with hospitalized patients with seasonal influenza (n = 547), we found that patients with RSV infections were similar in age but more frequently had underlying chronic lung diseases and major systemic comorbidities; time to presentation was longer; wheezy breathing and dyspnea was more frequent; and high fever was less common (Table 1). Substantial proportions of patients in both cohorts had cardiorespiratory complications. Rates of use of supplemental oxygen and assisted ventilation tended to be higher among RSV patients, but there was no significant difference in Figure 2. Representative frontal chest radiographs of patients with respiratory syncytial virus (RSV) infections. A, Frontal chest radiograph of a male RSV patient with underlying diabetes mellitus and ischemic stroke. There are ground glass opacities at the right middle, right lower, and left lower zones. He had a normal white blood cell (WBC) count (8 × 109/L), and no bacterial pathogen was isolated. He required supplemental oxygen therapy. B, Frontal chest radiograph of an elderly male RSV patient with history of old tuberculosis and diabetes mellitus. It shows consolidative changes at the left lower zone. He had a normal WBC count (5 × 109/L), and no bacterial pathogen was isolated. Outcomes of Hospitalized Adults With RSV • CID • 5 Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 Figure 1. Time of hospital admission of 607 adult patients with virologically confirmed respiratory syncytial virus (RSV) infection, Hong Kong, 2009–2011. RSV seasonal peaks occurred during weeks 35–41 in 2009, weeks 8–14 in 2010, and weeks 33–39 in 2011; the median test positivity rates during these periods were 5.8% (interquartile range [IQR], 4.8%– 6.5%), 6.6% (IQR, 5.8%–9.8%), and 9.1% (IQR, 5.7%–13.7%), respectively [12, 13]. Abbreviation: RSV, respiratory syncytial virus. (Table 3). For the survivors, the median and mean durations of hospitalization were 7 (IQR, 5–14) days and 12 (SD, 13) days, respectively. Development of pneumonia in adult RSV patients was associated with lower survival; mortality within 30 days and 60 days for pneumonia cases was 15.6% (vs 4.3%) and 20.3% (vs 5.7%), respectively (Figure 3). Cox regression analyses showed that advanced age >75 years, pneumonia, requirement for ventilatory support, bacterial superinfection, and elevated serum urea level and white blood cell count were independent factors associated with lower survival, adjusted for potential confounders (Table 4; Supplementary Data 2). Use of systemic corticosteroids was not shown to be associated with survival. However, advanced age, presence of comorbidities, requirement for ventilatory support, and use of systemic corticosteroids were shown to be independently associated with longer hospitalization durations (Table 5; Supplementary Data 2). Rates of cultureproven, hospital-acquired bacterial infection were higher in patients who received corticosteroids than in those who did not (4.3% vs 1.1%, P = .012). Table 2. Explanatory Variables Associated With Acute Respiratory Failure Requiring Ventilatory Support in Hospitalized Respiratory Syncytial Virus Patients as Shown in the Final Logistic Regression Models Variables Associated With Acute Respiratory Failure Adjusted Odds Ratio (95% Confidence Interval) P Value RSV cohort, all cases (N = 607) No. Pneumonia 35 Pneumonia, COPD Pneumonia, multiorgan failure 5 2 Pneumonia, renal failure 2 Pneumonia, acute cardiovascular events Pneumonia, carcinoma of lung 3 1 <.001 Pneumonia 1.84 (1.03–3.28) .038 Acute cardiovascular events 8 1.05 (1.01–1.10) .008 Acute cardiovascular events, pneumonia Acute cardiovascular events, sepsis 3 1 1.01 (1.00–1.02) .004 COPD exacerbation 3 COPD exacerbation, sepsis COPD exacerbation, GI bleeding 1 1 Underlying malignancy (pneumonia) 5 1 1 Underlying chronic lung diseases Pneumoniab 3.65 (1.52–8.75) .004 3.05 (1.22–7.61) .017 GI bleeding (pneumonia) CAPD peritonitis (pneumonia) Serum alanine aminotransferase concentration, IU/L 1.01 (1.00–1.02) .037 Total Covariates in the model (all cases) included age, sex, major systemic comorbidity, and culture-confirmed bacterial superinfection. Overall, 18.7% and 15.0% of patients with chronic lung diseases and pneumonia, respectively, developed respiratory failure requiring ventilatory support. Covariates in the model (subgroup) included age, sex, major systemic comorbidity, culture-confirmed bacterial superinfection, and serum urea concentration at presentation. Abbreviation: RSV, respiratory syncytial virus. Additional radiographic review performed by independent radiologists. b Presence vs absence of ground-glass opacities on chest radiographs, as confirmed by radiologists. the overall outcomes of survival and duration of hospitalization from influenza patients, as shown in the univariate and multivariate analyses (Table 1; Supplementary Data 3 and 4). DISCUSSION Our data show that RSV can cause severe lower respiratory complications in older adults, resulting in respiratory failure, prolonged hospitalization, and high mortality similar to influenza. Corticosteroids did not seem to improve clinical outcomes. The unmet need for effective antiviral therapy and vaccination against RSV in adults should be promptly addressed. To our knowledge, this study describes the largest adult cohort of hospitalized RSV patients reported to date, and represents one of the few studies performed in Asia [9–11]. Consistent with data from Western countries, such patients were mostly of advanced age and had underlying chronic lung diseases or other major medical comorbidities [3–5, 17]; notably, >70% suffered from severe lower respiratory complications, including pneumonia, acute bronchitis, and exacerbations of • CID • Lee et al 72 Altogether, 72 patients died within 60 days postadmission; 52 (72.2%) had pneumonia diagnosed at presentation. The 50th, 75th, and 90th percentiles of time to death were 13, 29, and 45 days postadmission, respectively. Abbreviations: CAPD, continuous ambulatory peritoneal dialysis; COPD, chronic obstructive pulmonary disease; GI, gastrointestinal. COPD/asthma, and 14% developed cardiovascular complications [7, 17]. Although fulminant RSV pneumonia is typically described in patients who are profoundly immunosuppressed (eg, recipients of hematopoietic stem cell transplant) [2, 3, 24], we found clinicoradiological evidence of pneumonia (unilateral, patchy, ground glass opacity or consolidation) in >40% of these hospitalized adults, which was associated with high fever, dyspnea, and respiratory failure (more than two-thirds of cases required supplemental oxygen) [2–5, 17]. Upper respiratory symptoms of runny nose and sore throat could be absent [2–4, 6, 17, 21]. Importantly, we documented the poor outcomes of adults hospitalized for RSV infection: >10% of cases necessitated ventilatory support and the overall death rate exceeded 10% [2, 4, 5]. Pneumonic cases were shown to have the worst prognosis, with a ventilation rate of about 15% and mortality as high as 15%–20%. For the survivors, prolonged hospitalization was often required for the management of cardiorespiratory complications (eg, COPD exacerbation, congestive heart failure) [5]. Late deaths occurred because of secondary infections, cardiovascular events, or decompensation of comorbid conditions (Table 3) [6, 8]. Furthermore, we were able to show that among hospitalized adults, clinical manifestations, complications, and outcomes of RSV infection are comparable to those of seasonal influenza (majority being A/H3N2 in this series) [3, 5, 6]. Although in RSV patients, wheezy breathing and dyspnea might be more common, and the magnitude of fever sometimes lower, such symptoms Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 3.45 (1.93–6.20) Serum alanine aminotransferase concentration, IU/L Subgroupa (N = 286) 6 Cause of Death Underlying chronic lung diseases Serum urea concentration, mmol/L a Table 3. Reported Direct Causes of Death in 72 Patients Hospitalized With Respiratory Syncytial Virus Infection Table 4. Explanatory Variables Associated With Death in Hospitalized Respiratory Syncytial Virus Patients as Shown in the Final Cox Proportional Hazards Models (N = 607) Variables Associated With Death Adjusted Hazard Ratio (95% CI) P Value Events censored within 30 days postadmission Advanced age (>75 y) 2.85 (1.43–5.68) could not reliably differentiate it from influenza [3, 4, 17]. High rates of respiratory (56%–72%) and cardiovascular (13%–14%) complications occurred in both infections, with substantial proportions of patients requiring supplemental oxygen therapy (59%–68%) and ventilatory support (6%–11%) [5, 6]. Respiratory failure appeared to be more common among RSV patients, but there was a higher prevalence of chronic lung diseases among them. The overall outcomes of survival and hospitalization duration were not shown to be significantly different between RSV and influenza patients after adjustment for confounders [4–9]. Unlike influenza, antiviral treatment or vaccine is currently not available for RSV. Ribavirin and immunoglobulins have been used to treat (or prevent) severe RSV pneumonia in immunocompromised patients; however, controlled data are lacking, and whether these can be applied to the older adults are uncertain [3, 4, 24–26]. Our findings thus highlight the need for therapeutic and preventive interventions against RSV in adults. Recent progress on their development and the obstacles encountered has been reviewed elsewhere [3, 4, 24]. In addition, we examined the roles of bacterial infections and systemic corticosteroids in adult RSV infections. We found evidence of bacterial superinfection in about 15% of patients during their course of illness, which was a significant contributory factor to mortality (similar in influenza diseases) [4, 5, 9, 15, 17]. 2.80 (1.53–5.14) Requirement of ventilatory support Bacterial superinfection 6.21 (3.39–11.35) 2.02 (1.11–3.66) .001 Serum urea concentration, mmol/L 1.04 (1.00–1.08) .035 1.05 (1.00–1.10) Total WBC count, ×109/L Events censored within 60 days postadmission .059 <.001 .021 Advanced age (>75 y) 2.10 (1.18–3.73) .011 Pneumonia Requirement of ventilatory support 2.99 (1.75–5.11) 4.65 (2.71–7.98) <.001 <.001 Cardiovascular complications 1.71 (.97–3.02) .063 Bacterial superinfection Serum urea concentration, mmol/L 2.04 (1.20–3.48) 1.05 (1.01–1.08) .009 .004 Total WBC count, ×109/L 1.06 (1.01–1.10) .009 Adjusted hazard ratio >1 indicated increased risk of death. Covariates in the models included sex, major systemic comorbidities, chronic lung disease exacerbations, hospital site, and use of systemic corticosteroids. Subgroup analysis on cases with additional radiographic reviews showed similar results (Supplementary Data 2). Abbreviations: CI, confidence interval; WBC, white blood cell. As such, any bacterial infection should be promptly detected and treated according to local resistance profiles. Besides S. pneumoniae and H. influenzae, P. aeruginosa and other gram-negative bacilli may need to be considered in patients with underlying chronic lung diseases [4, 9, 15]. Corticosteroids Table 5. Explanatory Variables Associated With Duration of Hospitalization Among Survivors (n = 535) as Shown in the Final Cox Proportional Hazards Model Variables Associated With Duration of Hospitalization Adjusted Hazard Ratio (95% Confidence Interval) P Value Advanced age (>75 y) 0.74 (.62–.89) .001 Comorbidity, major systemic 0.77 (.64–.94) .010 Requirement of ventilatory support 0.39 (.28–.54) <.001 Use of systemic corticosteroids 0.76 (.63–.91) .002 An adjusted hazard ratio <1 indicated a lower chance of discharge. Covariates in the model included sex, chronic lung disease exacerbations, presence of pneumonia, bacterial superinfection, and hospital site. Subgroup analysis on cases with additional radiograph reviews showed similar results (Supplementary Data 2). The median duration of hospitalization among patients who received systemic corticosteroids was 8 (interquartile range [IQR], 5–18) days, and 6 (IQR, 5–12) days in patients who had not received corticosteroids; 73% of patients who received systemic corticosteroids also received inhaled corticosteroids [14–16]. Outcomes of Hospitalized Adults With RSV • CID • 7 Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 Figure 3. Kaplan-Meier survival curves of 607 adults hospitalized for respiratory syncytial virus (RSV) infection. Patients who developed pneumonia were shown to have lower survival. Among RSV patients who had pneumonia, the crude 30-day and 60-day mortality was 15.6% and 20.3%, respectively (4.3% and 5.7%, respectively, in those without pneumonia). Subgroup analysis on cases with additional radiograph reviews showed similar results (data not shown). .003 Pneumonia 8 • CID • Lee et al therapies and immunization of high-risk adults (eg, small interfering RNA, fusion protein inhibitor, newer generation immunoglobulins, subunit vaccines) [3, 4, 24, 38, 39] are urgently needed. Supplementary Data Supplementary materials are available at Clinical Infectious Diseases online (http://cid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author. Note Potential conflicts of interest. All authors: No reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed. References 1. Nair H, Nokes DJ, Gessner BD, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet 2010; 375:1545–55. 2. Cesario TC. Viruses associated with pneumonia in adults. Clin Infect Dis 2012; 55:107–13. 3. Walsh EE. Respiratory syncytial virus infection in adults. Semin Respir Crit Care Med 2011; 32:423–32. 4. Murata Y, Falsey AR. Respiratory syncytial virus infection in adults. Antivir Ther 2007; 12(4 Pt B):659–70. 5. Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med 2005; 352:1749–59. 6. Widmer K, Zhu Y, Williams JV, Griffin MR, Edwards KM, Talbot HK. Rates of hospitalizations for respiratory syncytial virus, human metapneumovirus, and influenza virus in older adults. J Infect Dis 2012; 206:56–62. 7. Jansen AG, Sanders EA, Hoes AW, van Loon AM, Hak E. Influenzaand respiratory syncytial virus-associated mortality and hospitalisations. Eur Respir J 2007; 30:1158–66. 8. van Asten L, van den Wijngaard C, van Pelt W, et al. Mortality attributable to 9 common infections: significant effect of influenza A, respiratory syncytial virus, influenza B, norovirus, and parainfluenza in elderly persons. J Infect Dis 2012; 206:628–39. 9. Choi SH, Hong SB, Ko GB, et al. Viral infection in patients with severe pneumonia requiring intensive care unit admission. Am J Respir Crit Care Med 2012; 186:325–32. 10. Xiang Z, Gonzalez R, Ren L, et al. Prevalence and clinical characteristics of human respiratory syncytial virus in Chinese adults with acute respiratory tract infection. J Med Virol 2013; 85:348–53. 11. Olsen SJ, Thamthitiwat S, Chantra S, et al. Incidence of respiratory pathogen in persons hospitalized with pneumonia in two provinces in Thailand. Epidemiol Infect 2010; 138:1811–22. 12. Chiu SS, Chan KH, Chen H, et al. Virologically confirmed populationbased burden of hospitalization caused by respiratory syncytial virus, adenovirus, and parainfluenza viruses in children in Hong Kong. Pediatr Infect Dis J 2010; 29:1088–92. 13. Center for Health Protection, Hong Kong SAR. Seasonal increase in RSV activity. Communicable diseases watch. Available at: http://www. chp.gov.hk/files/pdf/cdw_v9_6.pdf Accessed 30 January 2013. 14. Lee N, Choi KW, Chan PK, et al. Outcomes of adults hospitalised with severe influenza. Thorax 2010; 65:510–5. Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 are commonly used to treat wheezy attacks and exacerbations of COPD/asthma in adults, including those triggered by viral infections [16, 27]. In this large RSV cohort, we did not observe any benefit on clinical outcomes with systemic corticosteroid treatment in the multivariate analyses, adjusted for disease severity. Instead, increased bacterial infections and longer hospitalization duration were found. Limiting our analysis to a patient subset presenting with wheezy breathing and dyspnea showed similar results (data not shown). We cannot eliminate indication bias, but these findings are supported by randomized controlled trials in young children, which revealed lack of clinical benefit and inconsistent control of inflammatory cytokine responses with corticosteroids [28–30]. A recent adult study reported similar findings; it also showed that humoral immunity against RSV was diminished, although virus control appeared unaffected [31]. Emerging evidence suggests worse outcomes with corticosteroid use in influenza pneumonia [16, 32]. Taken together, it is suggested that the decision to treat RSV patients with corticosteroids should be weighed against the potential risks, and be limited to a short course if used [4, 25, 31]. Further study is indicated. The strengths of our study include a large sample size, multicenter design, and virological confirmation of cases. Identical clinical settings and research methods had allowed more precise comparisons between the 2 viral infections. Chest radiographs were independently reviewed; the detailed findings will be reported separately [22]. Our study is limited by its retrospective nature; therefore, variables least prone to bias were chosen as outcome measures, and confounders adjusted carefully in multivariate analyses. The use of IFA instead of PCR for the diagnosis of RSV in our service settings could also be a limitation. IFA is highly specific (95%–99%), and moderately sensitive (80%–94%, higher with NPA) in children; the sensitivity in adults is generally lower because of lower virus shedding levels [3, 4, 12, 18–20, 33]. Although increased test sensitivity can be expected in the older, hospitalized adults with severe RSV disease because of their higher viral titers and longer virus shedding durations [34–36], it is possible that some cases, especially the milder ones, had remained undetected. Using PCR (without or without paired serology) for diagnosis should reveal a greater disease burden [4, 34]. We have planned to perform PCR, neutralizing antibodies, and virus subtyping in our patients in the near future (evidence suggests that both serotypes A and B circulate in Asia) [10]. In conclusion, adults hospitalized for RSV infection have high morbidity and mortality, comparable to outcomes in influenza patients. Studies on disease pathogenesis (eg, viral dynamics, immune response, viral–bacterial interactions) [3, 4, 34–36]; strategies to improve case finding, diagnosis, and infection control in the hospital setting (eg, PCR, serology, aerosol transmission) [3, 4, 17, 34, 35, 37]; and development of antiviral 27. Rabe KF, Wedzicha JA. Controversies in treatment of chronic obstructive pulmonary disease. Lancet 2011; 378:1038–47. 28. Somers CC, Ahmad N, Mejias A, et al. Effect of dexamethasone on respiratory syncytial virus-induced lung inflammation in children: results of a randomized, placebo controlled clinical trial. Pediatr Allergy Immunol 2009; 20:477–85. 29. Ermers MJ, Rovers MM, van Woensel JB, Kimpen JL, Bont LJ; RSV Corticosteroid Study Group. The effect of high dose inhaled corticosteroids on wheeze in infants after respiratory syncytial virus infection: randomised double blind placebo controlled trial. BMJ 2009; 338:b897. 30. Fernandes RM, Bialy LM, Vandermeer B, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev 2010; CD004878. doi:10.1002/14651858. 31. Lee FE, Walsh EE, Falsey AR. The effect of steroid use in hospitalized adults with respiratory syncytial virus-related illness. Chest 2011; 140: 1155–61. 32. Lee N, Hui DS. Dexamethasone in community-acquired pneumonia. Lancet 2011; 378:979–80. 33. Casiano-Colón AE, Hulbert BB, Mayer TK, Walsh EE, Falsey AR. Lack of sensitivity of rapid antigen tests for the diagnosis of respiratory syncytial virus infection in adults. J Clin Virol 2003; 28:169–74. 34. Walsh EE, Peterson DR, Kalkanoglu AE, Lee FE, Falsey AR. Viral shedding and immune responses to respiratory syncytial virus infection in older adults. J Infect Dis 2013; 207:1424–32. 35. Duncan CB, Walsh EE, Peterson DR, Lee FE, Falsey AR. Risk factors for respiratory failure associated with respiratory syncytial virus infection in adults. J Infect Dis 2009; 200:1242–6. 36. DeVincenzo JP, Wilkinson T, Vaishnaw A, et al. Viral load drives disease in humans experimentally infected with respiratory syncytial virus. Am J Respir Crit Care Med 2010; 182:1305–14. 37. Lindsley WG, Blachere FM, Davis KA, et al. Distribution of airborne influenza virus and respiratory syncytial virus in an urgent care medical clinic. Clin Infect Dis 2010; 50:693–8. 38. Bonavia A, Franti M, Pusateri Keaney E, et al. Identification of broadspectrum antiviral compounds and assessment of the druggability of their target for efficacy against respiratory syncytial virus (RSV). Proc Natl Acad Sci U S A 2011; 108:6739–44. 39. DeVincenzo J, Lambkin-Williams R, Wilkinson T, et al. A randomized, double-blind, placebo-controlled study of an RNAi-based therapy directed against respiratory syncytial virus. Proc Natl Acad Sci U S A 2010; 107:8800–5. Outcomes of Hospitalized Adults With RSV • CID • 9 Downloaded from http://cid.oxfordjournals.org/ by Norman Sharples on August 20, 2013 15. Lee N, Chan PK, Lui GC, et al. Complications and outcomes of pandemic 2009 influenza A (H1N1) virus infection in hospitalized adults: how do they differ from those in seasonal influenza? J Infect Dis 2011; 203:1739–47. 16. Lee N, Chan PK, Hui DS, et al. Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis 2009; 200:492–500. 17. Walsh EE, Peterson DR, Falsey AR. Is clinical recognition of respiratory syncytial virus infection in hospitalized elderly and high-risk adults possible? J Infect Dis 2007; 195:1046–51. 18. de-Paris F, Beck C, Machado AB, et al. Optimization of one-step duplex real-time RT-PCR for detection of influenza and respiratory syncytial virus in nasopharyngeal aspirates. J Virol Methods 2012; 186:189–92. 19. Chan KH, Peiris JS, Lim W, Nicholls JM, Chiu SS. Comparison of nasopharyngeal flocked swabs and aspirates for rapid diagnosis of respiratory viruses in children. J Clin Virol 2008; 42:65–9. 20. Ohm-Smith MJ, Nassos PS, Haller BL. Evaluation of the Binax NOW, BD Directigen, and BD Directigen EZ assays for detection of respiratory syncytial virus. J Clin Microbiol 2004; 42:2996–9. 21. Lee N, Chan PK, Wong CK, et al. Slow viral clearance and hyperactivated inflammatory responses in adults hospitalized for severe pandemic 2009 influenza A(H1N1) virus pneumonia. Antiviral Therapy 2011; 16:237–47. 22. Wong S, Yu J, Lee N, Lui G, Wong KT, Ahuja A. Initial radiographic features as outcome predictor of adult RSV respiratory tract infection. In: European Congress of Radiology, Vienna, Austria, March 2013 (abstract). 23. Syha R, Beck R, Hetzel J, et al. Human metapneumovirus (HMPV) associated pulmonary infections in immunocompromised adults—initial CT findings, disease course and comparison to respiratory-syncytial-virus (RSV) induced pulmonary infections. Eur J Radiol 2012; 81:4173–8. 24. Shah JN, Chemaly RF. Management of RSV infections in adult recipients of hematopoietic stem cell transplantation. Blood 2011; 117: 2755–63. 25. Park SY, Baek S, Lee SO, et al. Efficacy of oral ribavirin in hematologic disease patients with paramyxovirus infection: analytic strategy using propensity scores. Antimicrob Agents Chemother 2013; 57:983–9. 26. van Woensel JB, Vyas H; STAR Trial Group. Dexamethasone in children mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus: a randomized controlled trial. Crit Care Med 2011; 39:1779–83.