* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
CARDIAC ARRHYTHMIAS &
ANTI-ARRHYTHMIC DRUGS
PART II
16th Feb 2017
ANTI-ARRHYTHMIC
or
ANTI-DYSRHYTHMIC DRUGS
2
Antidysrhythmic Drugs
• A classification of antidysrhythmic drugs based
on their electrophysiological effects was
proposed by Vaughan Williams in 1970.
• It provides a good starting point for discussing
mechanisms, although many useful drugs do
not fit neatly into this classification.
• Furthermore, emergency treatment of serious
dysrhythmias is usually by physical means (e.g.
pacing or electrical cardioversion by applying a direct
current shock to the chest or via an implanted device)
rather than drugs
3
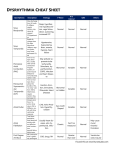
Antidysrhythmic DrugsClassification
There are 4 classes:
• Class I: Inhibitors of Na+ influx (voltage sensitive
Na)- subdivided into Ia, Ib and Ic
• Class II: ß-adrenoceptor antagonists
• Class III: Drugs that substantially prolong the
cardiac action potential
• Class IV: Calcium antagonists
4
Class I Drugs-Inhibitors of Na+
Influx
• Inhibit the fast Na+ channels
• also block the slow Ca2+ - Na+ channels
• reduce intracellular Ca2+ leading to a -ve
inotropic effect
• must be used with care where heart failure
is suspected
5
• inhibition of Na+ channels leads to either:
- (a) slowing of conduction
- (b) increase in refractory period
• Drugs under this class have local anaesthetic or
membrane stabilizing effect
6
Class I subgroups: Ia, Ib and Ic
• The reason for subdivision is that the earliest
examples, quinidine and procainamide (Class
Ia) have different effects from many of the more
recently developed drugs, even though all
share the same basic mechanism of action.
• A partial explanation for these functional
differences comes from electrophysiological
studies of the characteristics of the sodium
channel block produced by different class I
drugs.
7
Class Ia:
• suitable for ventricular & supraventricular
arrhythmias
• include:
quinidine
procainamide
Disopyramide
Lorcainide
8
Class Ia …
In the therapeutic concentrations they:
• raise the threshold for excitation (lengthen AP
duration)
• cause minor slowing of intra-cardiac conduction
• widen the QRS complex
• they prolong the AP and lengthen the effective
refractory period (probably results from K+
channel blockade) of atrial, ventricular &
purkinje fibres.
9
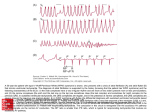
NB:
• QRS Complex is a name for the
combination of three of the graphical
deflections seen on a typical
electrocardiogram {ECG –a record or
display of a person’s heart beat produced
by electrocardiography}
• It is usually the central and most visually
obvious part of the tracing,
• It corresponds to the depolarization of the
right and left ventricles of the human heart.
10
Class Ia…
• Quinidine, procainamide & disopyramide have a
low therapeutic index
• their -ve inotropic effects extend to skeletal
muscle (aggrevation of myasthenia gravis) and
vascular smooth muscle (hypotension)
-varying degree of atropine-like effect.
11
Class Ib
• suitable for suppression of ventricular
arrhythmias after myocardial infarction
• include:
Lignocaine, Phenytoin, Mexiletene and
tocainide
Properties:
-they shorten AP duration & effective refractory
period
- have no effect on intra-cardiac conduction or
QRS complex
12
Class Ib…:
Lignocaine/lidocaine
• Has a rapid onset of action and a short half-life
(approx. 1h)
• given i/v as the 1st line drug in the treatment of
ventricular arrhythmias after myocardial
infarction and surgery
• inactive orally
• also an antagonist at muscarinic acetylcholine
receptors and may evoke mild tachycardia by
removing the effect of vagal tone on the SA
node
• SE: confusion, fits, sweating and drowsiness13
Class Ib: Phenytoin
• used almost exclusively in digitalisinduced ventricular arrhythmias
• Its general anti arrhythmic effectiveness is
less than that of lignocaine
• Side Effects: hypotension
14
Class Ib:…
Tocainide:
-analogue of lignocaine
-active orally and i/v
-has similar electrophysiological &
haemodynamic properties to lignocaine.
-longer acting
Mexiletene:
-similar electrophysiological properties to
lignocaine
- active orally and i/v
15
Class Ic
• Drugs in this group have 2 effects:
(a) slow intra-cardiac conduction
(b) widen the QRS complex
• They do not so much affect the
threshold of excitation
• Include: Flecainide, Encainide, and
Propafenone
16
Class Ic; Flecainide
• Slows conduction in atria, His-purkinje
system, accessory pathways &
ventricles
• in therapeutic concentrations it causes
lengthening of the PR & QRS intervals
• it is a powerful broad spectrum
antiarrhythmic effective vs atrial
arrhythmias, tachycardia involving
accessory pathways (Wolff-ParkinsonWhite syndrome) & ventricular
arrhythmias
17
• Class Ic:Encainide:
-similar antiarrhythmic spectrum to
flecainide
• Class Ic: Propafenone:
-has additional minor ß-blocking and
calcium channel antagonist properties
-effective against supraventricular and
ventricular arrhythmias
18
Class II: ß-adrenoceptor
antagonists
• effective in arrhythmias associated with
sympathetic overactivity or increased
circulating catecholamines
• E.g. Myocardial infarction, emotion, exercise,
anaesthesia
• they reduce automaticity (ectopic
pacemaker)
19
Class II: ß-adrenoceptor
antagonists …
• increase effective refractory period
• decrease conduction velocity
• Include:
Propranolol
Atenolol
Metoprolol
Acebutolol
Timolol
20
Class II
Bretylium:
• has adrenergic neurone blocking activity
• suppresses release of NA
• It is both Class II & III
21
Class III
Drugs That Prolong Both the Action Potential
and Refractory Period
• Also called slow repolarizers
• they block K+-channels
• prolong the duration of the plateau region of
cardiac AP
• lengthen effective refractory period
22
Drugs: Amiodarone, bretylium, sotalol
Amiodarone:
• blocks K+ & Na+ - channels
• it is a non-competitive antagonist at alpha &
ß-adrenoceptors (Class I and class II
effects)
• effective against many arrhythmias
including Wolff-Parkinson-White syndrome)
• due to side effects it is only used when
other drugs can not be used
23
• It causes irreversible liver damage,
thyroid disorders (its molecule contains
iodine)
• it causes neuropathy & pulmonary
alveolitis
Sotalol:
• it is a non-selective beta-blocker
• also has class III activity
• prolongs atrial & ventricular action
potential duration
• prolongs refractory period
24
Class IV
Inhibitors Of Calcium Influx (Calcium
antagonists)
• Inhibit the slow inward Ca2+ - current which
result in:
(1) slowed conduction
(2) prolonged refractoriness in the AV node
• useful for supraventricular tachycardia involving
the AV node.
• Blocks intranodal re-entry circuits
25
• effective in some types of re-entry
tachycardia in which the AV node is
involved
• Not effective in Wolff-Parkinson-White
syndrome
26
Class IV drug-Verapamil
• effective when the Ca2+ channels are either
activated or inactivated (occurs when frequency
of AP is high) [use-dependent]
• It is the main drug
• Used to prevent recurrence of paroxysmal
supraventricular tachycardia
• And to reduce the ventricular rate in patients
with atrial fibrillation (especially if inadequately
controlled with digoxin), provided they do not
27
have Wolff-Parkinson-White or related disorder
Class IV drug- Diltiazem:
• similar antiarrhythmic properties to
verapamil
28
• Nifedipine: not anti-arrhythmic. It does not
exhibit use-dependence
• it also blocks the slow Ca2+ channels but
it is only effective when the channels are
in the activated state
29
Not Classified
DIGOXIN:
• slows conduction and prolongs the refractory
period in the AV node and bundle of His
• used in atrial fibrillation which it does not stop
but it slows & strengthens the ventricular beat
• reduces the frequency at which impulses pass
along the conducting tissue
• Principal indication: CHF associated with atrial
fibrillation
30
Adenine nucleotides
• Adenosine & ATP
• used as substitutes for verapamil in the
treatment of supraventricular tachycardias
(adenosine is safer than verapamil)
• they act via purinergic receptors situated in the
SA & AV nodes
• stimulation of these receptors hyperpolarizes
cells resulting in suppression of automaticity
and conduction
31
•
Interrupt re-entry circuits in AV nodal
tachycardia, and AV tachycardia involving an
accessory pathway (Wolff-parkinson-White
syndrome).
ALTERNATIVE TO DRUGS
1) use of pacemakers
2) DC shock - if atrial size is normal it causes
reversion to normal rhythm in most patients
with atrial fibrillation (relapse 60% within 1 yr)
3) surgical ablation of ectopic focus or bundle of
His to control supraventricular arrhythmias pacemaker
32
References
1.
2.
3.
4.
5.
6.
7.
Lecture notes on clinical pharmacology 4th Ed. John L.
Reid, Peter C. Rubin & Brian Whiting
Basic Pharmacology 4th Ed by R.W. Foster
Pharmacology 5th ed by Rang & Dale et al
Medical Pharmacology at a glance by M.J. Neal
The Physiology of excitable cells 3rd ed by David J.
Aidley pg 313
Textbook of Medical physiology 7th ed. By Arthur C.
Guyton
Pharmacology by Rang & Dale, 7th edition, chapter 21
33
34