* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A. Medical History
Survey
Document related concepts
Transcript
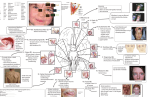
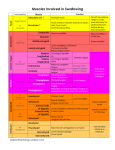
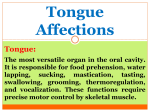
CLINICAL EVALUATION OF SWALLOWING Patient Name: Date: Patient DOB: Clinician: Patient Weight: Height: Gender: Male Female PU R PO SE S A. Medical History FO Date of Onset: Medications: Medical Diagnosis(es): Surgical History (include approximate dates): N O C T O N O D R ED U C AT IO Concern on referral: Primary Patient Complaint: PY AL Referral Source: ___ Antidepressant; ___ Antipsychotic; ___ Sedative; ___ Antihistimine; ___ Diuretic; ___Mucosal anesthetic; ___ Anticholinergic (please list medications below): CLINICAL EVALUATION OF SWALLOWING Related Medical History: Cardiac: SE S Gastroenterology (GI): Pulmonary: PO Neurological: PU R Otolaryngology (ENT): N Speech-Language Pathology: FO R Respiratory Status: O C T O N O ED U Occupation: D Primary language(s): C AT IO Social/Family: Hearing Status: PY AL Dental: YES NO Ventilator Dependent? YES NO Tracheostoma without tube? YES NO Tracheostomy Tube (If Yes, identify type:____________________________________) ___ Cuffed ___ Uncuffed ___ Fenestrated ___ Passy Muir valve ___ Finger occluded Other pertinent information (e.g. duration of placement, progression in transitioning to independent breathing, hygiene status, etc.): CLINICAL EVALUATION OF SWALLOWING B. Patient Status and Observations YES The patient is alert and oriented to time and place The patient is attentive and responds appropriately to questions SE S The patient appears confused, disoriented, or unable to respond appropriately to questions PO The patient appears ___ lethargic ___ sedated ___ unresponsive R The patient is cooperative PU The patient is uncooperative AL The patient is able to sit upright ___ independently ___with assistance O IO N PY The patient is unable to sit upright without assistance C C AT The patient is able to ambulate ___ independently ___with assistance O T The patient is immobile ___requires a wheelchair ___bedridden N ED U The patient is able to feed themselves independently O D FO R The patient requires adapted eating utensils or products to feed independently The patient is eating an oral diet ___without modification ___with modification or restriction The patient is not eating an oral diet ___NG ___NJ ___PEG ___TPN The patient is able to maintain oral hygiene ___independently ___with assistance The patient exhibits poor oral hygiene OTHER OBSERVATIONS: NO CLINICAL EVALUATION OF SWALLOWING YES C. SIGNS AND SYMPTOMS: Increased duration of meals Frequent or excessively dry mouth SE S Coughing/choking associated with eating Food or pills get stuck (ask them to point to location): PO Food remains in the oral cavity when eating, or pockets between the teeth and inside of the cheek(s) Food or liquid come out of the nose N Feel a burning sensation PY AL Food or liquid spill from the mouth while eating PU R Sensation of a lump in the throat O IO Experiences heartburn, indigestion, or burning in the chest associated with eating C C AT Experiences a wet or gurgly voice quality associated with eating T N ED Difficulty swallowing liquids O U Experiences an increased body temperature, or spikes a fever within an hour of eating a meal O D R Difficulty swallowing thicker foods that are not solid such as applesauce, mashed potatoes, or cooked vegetables FO Difficulty swallowing solid foods such as meat or raw vegetables Frequent throat clearing associated with eating Changes in smell (describe): Changes in taste sensation (describe): Onset of eating and swallowing problems was ___Sudden ___ Gradual (describe duration of onset): Swallowing problems occur during specific meals: ___Breakfast ___Lunch ___Dinner ___Snacks Swallowing problems occur during specific times of day: ___Morning ___Afternoon ___Evening ___Waken during the night OTHER SIGNS AND SYMPTOMS: NO CLINICAL EVALUATION OF SWALLOWING D. OROPHARYNGEAL SENSORY MOTOR EXAMINATION SENSE OF SMELL (CN I): Ask the patient to close their eyes and to tell you if and when they smell each of the following (do not tell them what you are offering, ask them). Indicate which of the following they correctly identified: Chocolate Coffee Peppermint PO SE S Orange rind FACE & LIPS (CN VII): I II III IV PU R If asymmetrical at rest, identify the abnormal facial quadrant Using the diagram to the right: QUADRANT I II III IV O C T O U C AT IO N PY AL Describe abnormal appearance: N O D ED SENSORY MOTOR EXAMINATION OF THE OROPHARYNGEAL MECHANISM FOR EATING FO R FACE & LIPS (CN V & CN VII) RESTING OBSERVATION The face is symmetrical at rest: Lip tremor observed: Adequate lip closure at rest: YES NO L/R Strength Sensation ROM Impaired Impaired Impaired (1 = (1 = mild, 2 = (1 = mild, 2 mild, 2 = mod, mod, 3 = severe) = mod, 3 = 3 = severe) severe) CLINICAL EVALUATION OF SWALLOWING FACE & LIPS (CN V & CN VII) YES NO L/R Strength Sensation ROM Impaired Impaired Impaired (1 = (1 = mild, 2 = (1 = mild, 2 mild, 2 = mod, mod, 3 = severe) = mod, 3 = 3 = severe) severe) SE S MOVEMENT ASSESSMENT Lift the eyebrows, or try to look at the ceiling to wrinkle the forehead: PO Close eyelids tightly against resistance: Smile widely so that the teeth show: PU R Pucker the lips as though kissing: Alternate smiling and puckering the lips as fast as possible for 7 seconds: O IO Puff out the cheeks and hold air in the mouth: N Frown while showing teeth (grimace): O O D ED FO R N U Move mouth from side to side: Say the sound, "ooh." (lip rounding during speech): Say the sound, "ee." (lip spreading during speech): Alternate saying "ooh ee ooh ee…" as quickly as possible for 7 seconds: C T C AT Puff out the cheeks and hold air in the mouth against pressure applied to each cheek and then both cheeks: Repeat the sound, "puh," as quickly as possible for 5 seconds (5-7 syllables/sec = norm for adults): Does the patient exhibit imprecise articulation of /p/? SENSORY ASSESSMENT Using a cotton ball, or Q-tip, gently touch the regions of the 3 regions of the face supplied by CN V and also the upper and lower lips and note any areas of reduced sensation: PY AL Smack the lips: CLINICAL EVALUATION OF SWALLOWING JAW & TONGUE (CN V, XII, VII, IX) YES NO ROM Strength Impaired Impaired L / R (1 = mild, 2 (1 = mild, 2 = mod, 3 = = mod, 3 = severe) severe) SE S RESTING OBSERVATION Does the jaw appear symmetrical at rest? PO Does the jaw appear symmetrical at rest? R Does the jaw exhibit a tremor? PU Does the jaw hang lower than normal? PY O C O D R Does the tongue exhibit a scalloped appearance around the edges (impressions from teeth)? Does the tongue or other oral mucosa appear dry, or exhibit signs of xerostomia? FO N O ED U Does the tongue exhibit unilateral grooves, symmetric grooves, or furrows on the surface of the tongue evidencing atrophy? T C AT IO N Does the patient have adequate and healthy dentition and oral hygiene? Does the patient exhibit poor oral hygiene and dentition status? Open the mouth widely - does the tongue appear symmetrical? Does the tongue exhibit fasciculations (the tongue must be positioned at rest in the mouth for this observation)? AL Is the patient edentulous? Does the tongue exhibit tremor in its rest position? Are there secretions, or signs of pocketed food within the oral cavity or under the tongue? Sensation Impaired (1 = mild, 2 = mod, 3 = severe) CLINICAL EVALUATION OF SWALLOWING JAW & TONGUE (CN V, XII, VII, IX) YES ROM Strength Impaired Impaired L / R (1 = mild, 2 (1 = mild, 2 = mod, 3 = = mod, 3 = severe) severe) NO SE S MOVEMENT ASSESSMENT Open mouth as wide as possible: PO Try to close your mouth against resistance: R Try to open your mouth against resistance: PU Now move the jaw to each side (left and right): N Does the patient exhibit a normal occlusion during the bite? Or malocclusion (describe): PY Clench the jaw together (i.e. bite): AL Open and close your mouth as quickly as possible for 7 seconds: C O IO Ask the patient to stick out their tongue and hold it for 2 seconds or more: FO O D Lick the periphery of the lips (along the vermillion border): With the mouth open, place the tongue tip behind the upper front teeth: With the mouth open, reach the tongue tip toward the nose: With the mouth open, place the tongue tip behind the lower front teeth: With the mouth open, reach the tongue tip toward the chin: Retract the tongue as far into the mouth as possible: R N O ED U Rapid repetitive lateral motion of the tongue between the left and right cheeks for 7 seconds (with the mouth held open): T C AT Rapid repetitive lateral motion of the tongue between the left and right angles for 7 seconds (with mouth held open): Trace the tongue along the hard palate from behind the teeth to as far back as possible (with the mouth held open): Does the patient move the tongue without needing to move the jaw? Sensation Impaired (1 = mild, 2 = mod, 3 = severe) CLINICAL EVALUATION OF SWALLOWING JAW & TONGUE (CN V, XII, VII, IX) (movement assessment, contin) YES NO ROM Strength Impaired Impaired L / R (1 = mild, 2 (1 = mild, 2 = mod, 3 = = mod, 3 = severe) severe) Sensation Impaired (1 = mild, 2 = mod, 3 = severe) Using a tongue blade, ask the patient to push the tongue tip against the tongue blade during tongue protrusion (i.e. against resistance): SE S Ask the patient to push their tongue against the inside of their left cheek against the resistance of your finger. Repeat tongue lateral strength testing with the right cheek: Using a tongue blade, apply pressure to the tongue dorsum and ask the patient to try to elevate their tongue tip against it: R PO Using a tongue blade, apply pressure to the left and then right sides of the tongue and ask the patient to try to resist their tongue being moved: PU Repeat the sound, "tuh," as rapidly as possible for 5 seconds (5-7 syllables/sec = norm for adults): Appy the Q-tip to the hard palate and soft palate regions along the midline while the patient keeps their eyes closed and raise their hand when they sense touch: Using a Q-tip and while the patient keeps their eyes closed, place it in a solution of 10% NaCl (salt) and touch it to the left side of the patient's protruded tongue and wait to see if they signal tasting it, then test the right side of the tongue in the same way: Using a Q-tip and while the patient keeps their eyes closed, place it in a solution of 10% glucose (sugar) and touch it to the left side of the patient's protruded tongue and wait to see if they signal tasting it, then test the right side of the tongue in the same way: FO O C T O N D R ED Using a Q-tip, apply light touch to the anterior left and right sides of the tongue while the patient keeps their eyes closed and raise their hand when they sense touch: O U Using a Q-tip, apply light touch to the posterior left and right sides of the tongue while the patient closes their eyes and raise their hand when they sense touch: PY N C AT SENSORY ASSESSMENT IO Does the patient exhibit imprecise articulation of /t/? Does the patient exhibit imprecise articulation of /k/? AL Repeat the sound, "kuh," as rapidly as possible for 5 seconds (5-7 syllables/sec = norm for adults): Repeat combinations of "puh tuh," "tuh kuh," and "puh tuh kuh" as rapidly as possible for 5 seconds (5-7 syllables/sec = norm for adults): CLINICAL EVALUATION OF SWALLOWING HARD/SOFT PALATE, PHARYNX, LARYNX (IX, X, XI) YES NO ROM Strength Sensation Impaired Impaired (1 Impaired (1 (1 = mild, = mild, 2 = = mild, 2 = 2 = mod, 3 mod, 3 = mod, 3 = = severe) severe) severe) L/R RESTING OBSERVATION SE S Do the palatal arches appear symmetrical? Does the hard palate appear intact? (If no, note cleft side, etc) PO Does the vault of the hard palate appear normal? (If no, note abnormality) Does the soft palate appear symmetrical? R Does the soft palate exhibit rhythmic or arrythmic movements characteristic of a myoclonus? PU Do the palatal arches appear symmetrical? Do you hear audible inhalation (i.e. stridor) or wheezing? Does the voice sound hoarse? ED D O Does the voice sound excessively breathy? Does the voice sound wet and gurgly? R C T O N U C AT Say the sound, "ah," loudly (not yelling, however) 5 times and note soft palate elevation consistency and symmetry: Do you observe lateral or posterior pharyngeal wall constriction during sustained or repeated production of "ah"? Is the patient's resonance normal? Or do you hear hypernasality or hyponasality? O IO N Does the palate elevate symmetrically during sustained phonation of "ah" (ask the patient to open their mouth wide - you may need to use a tongue blade to hold the tongue down to get a good look at the soft palate) PY AL MOVEMENT ASSESSMENT FO If the voice sounds wet and gurgly, ask the patient to clear their throat and sustained the sound, "ah," again: Does it still sound wet and gurgly? Ask the patient to take a deep breath and then bear down while holding their breath - can they hold their breath? Or do they exhibit air leakage during this task? Ask the patient to hold their breath for as long as possible and time how long they can do this (30-60 seconds is average): CLINICAL EVALUATION OF SWALLOWING HARD/SOFT PALATE, PHARYNX, LARYNX (IX, X, XI) (Movement Assessment, continued) YES NO ROM Strength Sensation Impaired Impaired (1 Impaired (1 (1 = mild, = mild, 2 = = mild, 2 = 2 = mod, 3 mod, 3 = mod, 3 = = severe) severe) severe) L/R SE S Ask the patient to perform a sharp cough - rate the cough using these descriptors: a. The cough was brisk with sharp hard onset of voicing followed by a strong audible exhalation PO b. Mildly weak cough c. Moderately weak cough R d. Severely weak cough PU e. Unable to produce a voluntary cough Do you feel elevation of the larynx during a dry swallow? AL SENSORY ASSESSMENT O IO N PY Does the patient gag or show sensitivity to touch of a tongue blade or Q-tip to the posterior 1/3 of the tongue? Does the patient gag or show sensitivity to touch of a tongue blade to the posterior oropharynx? C C AT E. Respiratory Assessment: ii) Ability to complete a dry swallow during quiet breathing without discomfort: N O T Record the number of breaths taken per second: ______ (norm = 12 – 16) U i) R O Duration of breath holding (instructed above): FO iii) D ED ___YES ___NO (If no, describe the breathing pattern relative to swallowing) F. Food Assessment: If the patient has been NPO before now, make sure they have completed oral hygiene cleaning before administering anything orally. If the patient has been eating orally, ask them to bring food they are currently eating, or observe during their meal time. FO O C T O N O D R ED U C AT IO N PY AL PU R PO SE S CLINICAL EVALUATION OF SWALLOWING CLINICAL EVALUATION OF SWALLOWING G. Recommendations: Oral versus Non-Oral nutrition and hydration: Regular PO diet (unrestricted diet) PO with modification or dietary restrictions (Specify): SE S Water protocol between meals only (requires oral hygiene) Liquids only (broth, nutritional supplements, milkshakes) PO Puree (specify runny versus thicker viscosity) R Soft and moist solids (easy to chew and easy to digest – avoid dry, PU dense, and stringy foods) NPO O C C AT Positional Strategies: IO Compensatory Strategies N Without supplemental oral intake PY AL With supplemental oral intake (specify): T Chin tuck O N U Head turn Right vs Left (circle one) O ED Lean or tilt to the Right vs Left (circle one) D OTHER: FO R Swallowing Maneuvers: Multiple swallows per bolus Breath hold prior to swallow Mendelsohn maneuver Effortful swallow Audible exhalation after the swallow OTHER: Adaptations or Compensations: Assistance with feeding CLINICAL EVALUATION OF SWALLOWING Verbal cues Food placement on plate Complete feeding assistance by other person Adaptive feeding device or method (refer to OT) Alternate liquids with food SE S Reduce rate of eating Temperature of food (specify cold, room, hot): PO Small and more frequent meals R Additional Testing Needed: PU Gastroenterology consultation Neurology consultation AL Otolaryngology consultation N O IO Dietitian consultation C C AT Home Health referral T Social Work assistance O O Videofluoroscopy N U Radiology referral ED PY Occupational Therapy consultation FO D R Chest X-Ray (with physician input) MRI (with physician input) CT (with physician input) Scintigraphy (with physician input) Flexible Endoscopic Evaluation of Swallowing (FEES) Flexible Endoscopic Evaluation of Swallowing and Sensory Testing (FEESST) Form taken from: Barkmeier-Kraemer J & Leonard R. (2014) Chapter 8: Clinical Swallow Evaluation. In: Dysphagia Assessment and Treatment Planning Workbook: A Team Approach (3rd Edition), 2013. Plural Publishing, San Diego, CA.