* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Survey
Document related concepts
Transcript
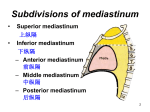
The CVS Mediastinum and pericardium Dr. Nabil Khouri MD, MSc, Ph.D Size & Location of Heart Average Size of Heart • 14 cm long • 9 cm wide • posterior to sternum • medial to lungs • anterior to vertebral column • base lies beneath 2nd rib • apex at 5th intercostal space • lies upon diaphragm The Location of the Heart within the Thoracic Cavity Figure 20.2a, b 3rd 4th The mediastinum is a broad central partition that separates the two laterally placed pleural cavities. It extends: from the sternum to the bodies of the vertebrae; and from the superior thoracic aperture to the diaphragm It contains the thymus gland, the pericardial sac, the heart, the trachea, and the major arteries and veins. It also serves as a passageway for structures such as the esophagus, thoracic duct, and various components of the nervous system as they traverse the thorax on their way to the abdomen. The Mediastinum MEDIASTINUM • • • • 1. Superior Mediastinum 2. Anterior mediastinum 3. meddle mediastinum 4. posterior mediastinum The Superior Mediastinum Boundaries Ant: Manubrium sterni Post: T-1 to T-4 Sides: Mediastinal pleura Sup: Plane of thoracic inlet Inferior: Imaginary line joining sternal angle and lower border T-4 10 Superior Mediastinum: Contents: Muscles: • Sternohyoid • Sternothyroid • Longus colli Thymus: (in childhood & puberty) Veins: • SVC • Lt & Rt brachiocephalic veins, • Lt Sup Intercostal vein Arteries: • Arch of Aorta • Brachiocepalic artery • Lt Common carotid • Lt subclavian artery 11 Trachea & Esophagus Nerves: • Vagus • Phrenic • Cardiac & • Lt recurrent laryngeal nerve (b/w trachea & oesophagus) Thoracic Duct Lymph nodes: • Brachiocephalic, • Tracheobronchial, The Thymus gland DEVELOPMENT- bilateral 3rd pharyngeal pouches EVOLUTION- largest at birth or during infancy increases slightly during 1st decade of life and decrease thereafter the site of T-cell production, Secrets Thomasine hormone which promotes the maturation of T cells Roughly a bi-lobed structure Normal weight- 5 – 50 gm The Superior Mediastinum 14 SECTION at T-4 15 Sterno-pericardial ligament. Internal thoracic artery & branches Anterior Mediastinum-(narrowest) Boundaries Ant: Body of sternum Post: Pericardium Sides: Mediastinal pleura Sup: Imaginary plane Inf: Diaphragm 17 Middle Mediastinum: Boundaries ????? Superior: Inferior: Posterior: Anterior: 18 Middle Mediastinum Contents: Heart enclosed in pericardium Arteries: Ascending Aorta, Pulmonary trunk with its Lt & Rt branches Veins: SVC, Termination of Azygos, Pulmonary veins Nerves: Phrenic, Deep cardiac plexus Bifurcation of Trachea with two principal bronchi Tracheobronchial lymph nodes 19 The Heart & the pericardium Anatomy of the Heart Wall Epicardium – covers the outer surface of the heart and is the same as the visceral pericardium and anchors the heart to the surrounding structures Myocardium – muscular wall of the heart (cardiac muscle cells) Endocardium – inner surface of the heart Components of the heart wall include (three layers) Epicardium – visceral pericardium Myocardium – cardiac muscle layer forming the bulk of the heart Endocardium – endothelial layer of the inner myocardial surface PERICARDIUM •The pericardium is supplied by several arteries that are in the area (e.g., the internal thoracic), and by the phrenic nerves, which contain vasomotor and sensory fibers. Pericardial pain is felt diffusely behind the sternum but may radiate. PERICARDIAL LAYER The Pericardium • The fibrous pericardium • The outermost layer, • Firmly bound to the central tendon of the diaphragm. • Extrapericardial fat, which may be visible radiographically, is often found in the angles between the pericardium and diaphragm on each side. • The pericardium is attached to the sternum (by the sternopericardial ligaments) and is adherent to the mediastinal pleura except where the two are separated by the phrenic nerves. • The serous pericardium: • Is a closed sac, subdivided into • the parietal layer of which lines the inner surface of the fibrous pericardium and is reflected onto the heart as the visceral layer, or epicardium. The potential space between the parietal and visceral layers contains a thin film of fluid and is known as the pericardial cavity. • Because of the manner in which the reflections of the pericardium occur during development at the arterial and venous ends of the heart, when the pericardial sac is opened interiorly in the adult it is possible to pass a finger posterior to the aorta and pulmonary trunk (arterial end of heart) and anterior to the left atrium and superior vena cava (venous end of heart). This passage is termed the transverse sinus of the pericardium • The reflection at the venous end is complicated and occurs as an inverted U along the pulmonary veins and inferior vena cava: this recess is termed the oblique sinus of the pericardium. Superior Vena Cava Aorta Pulmonary trunk Pulmonary Arteries Inferior Vena Cava The Posterior Mediastinum Boundries: The anterior boundary of the posterior mediastinum is the posterior pericardial wall. The posterior boundary is the anterior surfaces of the bodies of thoracic vertebrae T5-T12. Left Right Posterior pericardium The posterior wall of the pericardial cavity. The heart has been removed, we will able to see the cut borders of the major vessels entering and leaving the heart. The oblique pericardial sinus is clearly seen within the four pulmonary veins and inferior vena cava at this point. The Esophagus & vagus Nerves • When the pericardium is removed, – The esophagus can seen along with its plexus derived from the left and right vagus nerves. – The left vagus emerges from the plexus as the anterior vagal trunk and the right vagus becomes the posterior vagal trunk as the esophagus passes through the diaphragm to enter the abdomen,. – The branches from the sympathetic chain can also be seen • You can also see that the trachea splits into the right and left primary bronchi at the level of the junction between the superior and inferior mediastinum. • Once the esophagus has been removed, the thoracic aortan can be seen • The thoracic aorta starts at the T4T5 junction and extends the full length of the posterior mediastinum passing through the aortic hiatus of the diaphragm into the abdomen. • The thoracic aorta gives rise to the posterior inter-costal arteries which together with the posterior intercostal veins and intercostal nerves to form the neurovascular bundle that travels along the inferior border of a rib. • It also gives rise to bronchial branches that enter the root of the lung to supply the bronchi and lung tissue in addition to posterior pericardial arteries The thoracic aorta The thoracic duct Posterior and between the esophagus and thoracic aorta, you will find the thoracic duct, It is a fragile lymphatic duct that begins in the abdomen as the cisterna chyli at T4-T5 lumbar level. It travels through the superior mediastinum on its way into the neck, where it will enter the venous system at the junction of the internal jugular and left subclavian veins. Alongside and Posterior to the thoracic duct, the veins that drain the walls of the thorax, the azygos and hemiazygos veins. Each of these veins begin in the abdomen as the ascending lumbar veins. The hemiazygous veins: The upper intercostal spaces are drained by the superior hemiazygos vein and the lower the inferior hemiazygos vein. These two veins may join as one hemiazygos vein that passes behind the thoracic duct to empty into the azygos vein. The two veins may just as frequently pass into the azygos separately, forming two hemiazygos veins. The azygos and hemiazygos veins Splanchnic nerves If you reflect or remove the azygos system of veins, the next structures in the posterior mediastinum would be the splanchnic nerves, Specifically the greater splanchnic nerves. These nerves are derived from the sympathetic chains, thoracic ganglion T5 to T10. The lesser splanchnic nerves that are derived from ganglion T10 and T11. Some anatomist may describe the least splanchnic that is derived from ganglion T12. Remember, according to anatomists, the sympathetic chain is not part of the posterior mediastinum. The most posterior item in the posterior mediastinum is the anterior longitudinal ligament which completely covers the anterior surfaces of the bodies of the vertebrae. This extends from the sacral part of the vertebral column all the up to the skull. The sympathetic chain You should be able to identify the sympathetic ganglion white communicating ramus (preganglionic neurons) gray communicating ramus (postganglionic neurons) roots of the splanchnic nerves (postganglionic neurons) posterior intercostal veins posterior intercostal arteries intercostal nerves