* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download ophth-notes - WordPress.com
Survey
Document related concepts
Fundus photography wikipedia , lookup
Photoreceptor cell wikipedia , lookup
Retinal waves wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Vision therapy wikipedia , lookup
Contact lens wikipedia , lookup
Near-sightedness wikipedia , lookup
Visual impairment wikipedia , lookup
Cataract surgery wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Keratoconus wikipedia , lookup
Dry eye syndrome wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Macular degeneration wikipedia , lookup
Transcript
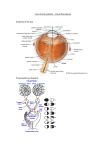
http://www.enlightenme.org/knowledge-bank/cempaedia/eye-initial-assessment The external eye Hordeolum externum (stye) o o o o infection/abscess of lash follicle – including Moll (sweat glands) or Zeis (sebum glands). Cause - usually staph Point outwards causing a lot of inflam. Mgmt- local Abx – fusidic acid Hordeolum internum o o o o Abscess/infection involving meibomian glands- or meibomian cyst Point inwards into conjunctiva and cause much inflame. CF- vision may be affected if corneal planus occurs. Mgmt- incision and curettage under LA P.M.- Chalazion is more rounded and would not have a yellow head. Blepharitis o o o o o Lid inflam Cause- stapy (bacterial form due to lid commensuals), rosacea, sebbroheic dermatitis (as a result of meibomian gland dysfunction) CF- spread to lid margins, burning, itching and scales on lashes; eye irritation, dryness (tear film dysfunction) & stickiness. O/E= conjunctivial injection (dilatation of bv) Mgmt- wipe crust from eyelids, Tears Naturale, fusidic acid and doxy- adults and erythro- children. Pinguelcula o o o o Degenerative vascular yellow/grey nodule on either side of cornea in the conjunctiva Ass- wind/sand blown environments, adult male, increased hair and skin pigmentation and sun related skin damage. If inflamed – pingueltitis – ttt with topical steroids If affecting the cornea – ptyregium - ttt- surgery Entropian o o o o Inversion of lower eyelid due to degenerative fascial muscles. Rare <40years Corneal abrasion as lashes point inwards Mgmt- taping lower eyelid, botox or surgery Ectropian o o o o Eversion of lower eyelid, Increased drainage of tears – dry eyes, eye irritation, watering and exposure keratitis Ass- old age, facial palsy Mgmt- gold plate in upper eyelid to enable closure of eyelid Upper lid malposition o o o Can be due to globe hypetrophy/excess tissue (pseudoproptosis) or intrinsic levator weakness (true proptosis). Due to congential, mechanical (xanthalasama, odemal, upper lid tumour), endocrine (hyperthyrodisim), CNS (3rd nerve palsy, Horners). Congential ptosis corrected surgically. Lagopthalmos o o o o Inability/difficulty closing the eyelid over globe Corneal ulcers and keratitis Causes: exophthalmos, mechanical impairment of lid movement, leprosy, paralysed orbicularis oculi, Mgmt- lubrication with liquid paraffin oil. May require tarsograpphy, Dendritic ulcers/herpes simplex virus keratitis o o o o o N.B Keratitis = inflame of cornea (Layers of cornea; epithelium, bowmans, stroma, dua’s dechemet and endothelim ) Causes by HSV, usually 1, remains dormant in trigeminal ganglion until re-activated. CF- photophoia and watering, pain, redness, blurred vision (corneal inflammation). Stain with fluroescien 1% Mgmt – acyclovir 3% (x5 daily) with steroid (to prevent corneal invasion, scarring and blindness) HSV affects corneal epithelium whereas HZO affects stroma & anterior uvea. N.B. Marginal keratitis – caused by hypersensitivity reaction to endotoxins colonising lids leading to immune complex deposition in peripheral cornea. CF=keratitis. O/E= multiple peripheral subepithelial corneal infiltrates= separated from the limbus by a clear zone. Mgmt=topical Abx & steroids Eyelid tumours Benigno o Skin papilloma, seborrehorc keratosises (basal cell papillomas) Keratocanthoma o o Pyogenic granulomata as a response to injury. Congenital vascular naevi (port wine stains and strawberry naevi can include eyelids) Malignant Basal cell cx o o o Rodent ulcer, nodular lumps with pearly edges +/- pearly telangiecstasia. 90% of malignant Mgmt- mohs microsurgery Squamous cell cx o o o Common in upper lid, increasing age and in women Arise form meibomian gland, zeis glands Mortality – 10% Malignant melaona o WLE Merkel cell cx o Violacous nodule, elderly, rapid growth Kaposi sarcoma o AIDS- post-radio, purple nodule Tears and lacrimation Anatomy o o o o o Tears/lacrimal fluid made by lacrimal gland S/T Lacrimal gland alone innervated by facial nerve as a reflex but produced by various other structures; e.g. meibomian gland, lacrimal gland etc. 1.2ul/min produced with approx. 6uL within the eye at any time Drainage occurs via S and I punctum, via ampulla, via canaculli, Valve of Rosenmuller draining into lacrimal sac, before entering nasolacrimal duct in to the I turbinate. Tears composed of IgA, contain lysozyme and B-lysin for antibacterials Acute dacrosystistis o o o Inflam of lacirmal sac – M enlargement, may spread to surrounding tissue (cellulitis) & result in systemic upset. Mgmt- imm Abx Comp- abscess formation Chronic dacrosystitis o Middle aged/elderly. o o o o Lacirmal sac distention, mucopus discharge +/- nasolacrimal duct block TTT- infection If NSD completely blocked – dacryocystorhinostomy (DCR) Ass – squamous cell cx Nasolacrimal duct non-canalization o o By 1 yr- should be canalized if not requires probing under GA CF – persistent watery eye & prone to attacks of conjunctivitis Dry eyes syndrome (keratoconjunctivits sicca) o o o Problem due to reduced production (old age, Sjogren’s syndrome), or excessive evaporation (post-exposure keratitis) or mucin deficency in tears (stevens-johnson syndrome, chemical burns, phemigoid, avitaminosis A) I- schirmers test >15mm in 5min Sx ttt- artificial tears Excess lacrimation o Causes – emotion, corneal abrasion. Foreign body, entropian, conjunctivitis, acute glaucoma, iritis. Ephiphora o o o Normal volume but not drained to I meatus Causes- ectropian, blocked drainage system (idiopathic/tumour) TTT- DCR for NLD obstruction. Orbital Swelling o o Lesions in the bony orbit = proptosis (protrusion of orbit) If excessive pressure= deviation of eyeball +/- diplopia Orbital cellulitis-SOS o o o o o o o Causes; HIB, staph a, strep pyognes, strep pneumoniae Spreads from paranasal sinus, esp post sinusitis, external ocular, dental injury/infection Typical CF- child, swelling (conjunctival injection), inflam of orbit, fever and reduced eye mobility Optic nerve affected=RAPD I- Prompt CT Mgmt- IV Abx cefuroxime +/-surgery (drainage of abscess) Comp- blindness (optic nerve compression) & systemic (cavernous sinus thrombosis, abscess meningitis) o N.B. Ass- rhabdomyosarcoma DDx- pre-septal cellulitis- only eyelid affected, no ocular involvement Carotico-cavernosus fistula o o o o o o Post rupture of carotid artery aneurysm, backflow of blood into cavernous sinus Causes; spontaneous, trauma (75%). CF- engorgement of vessels, lid & conjunctiva oedema. O/E exophthalmos may be pulsatile with loud bruit (heard as buzzing) over eye +/- tinnitus I- cerebral angiopathy Mgmt- embolization or ligation N.B. Carotid artery dissection – ALWAYS- CF=sudden onset of Horner’s (MAP= mipancoastosis, anhydrosis & partial ptosis-Muller’s muscle) with headache, pain in the face, neck/jaw, X of recurrent neck trauma= high proportion in young people. Urgent CT. Aneurysmal dilatation= mass effect on sympathetic fibres=Horner’s syndrome. Mgmt= observation, anticoag, carotid artery stenting/ligation. Orbital tumour o o o o o o o 1o neoplasia rare 3% orbital mets (breasts, lung, GI) Children- unilateral proptosis = 1st sign of neuroblastoma Nasopharyngeal tumours may invade orbit Mucoceles and pyoceles pf ethmoid and frontal sinus. DDx=Hyperthyroidism; Graves ( eye disease- 30%. Autoimmine reaction to orbital antigens= infiltration= oedema. CF= proptosis, chemosis, & conjunctivial injection (redness), lid retraction, lid lag, restrictive eye movments & diplopia) Conjunctivial redness=propotosis & lid retraction=corneal exposure. If unttt= corneal ulceration & compressive optic neuropathy. Inferior rectus most affected, then medial rectus I-CT orbit Opthalmic shingles (herpes zoster opthalmicus-HZO) o o o Accounts for 20% of HZO involvement >55% thoracic spinal nerve involvement >50% involves eyes , cornea; signs +/-iritis, >40% sectoral iris atrophy CF- pain and neuralgia in V1 Trigeminal, with blistering rash, involving the eyelid, Hutchinson sign (nasociliary branch invovled), headache, blurry vision o o o Comp if ImmunoComp- dissemination & post-herpetic neuralgia – chronic pain in the region of rash that can be delibitating Mgmt- Aciclovir x5/24hrs/7 days or famciclovir x1/24hrs/7days Refer – if >3days redness & Hutchinson sign (tip of nose) for ddx of anterior uveitis. Retinoblastoma o o o o o 1/15000 cases. AD, hereditary version, RB gene located 13q14. Common tumour among children CF- loss of red reflex- leukocoria, strabismus. Good prognosis but loss of vision in affected eye due to enucelation. Also chemo/radio. Screen relatives Eye movements and squints (strabismus, psudosquints (prominent epicanthic folds) tropia and phoria) Non-paralytic squints- due to lazy muscles o o o o o o Start in childhood I- corneal reflection and cover test (Gobin’s principle= evaluate all aspects of strabisums) Esotropia (convergent) – turned in o Common in children o No causes/ due to hypermetropia Exotropia (divergent) – one eye turned out o Occur in older children and often intermittent Hypertropia – turned up Hypotropia- turned down o Mgmt- 3O’s- optical (1% cyclopentolate to relax and mydriasis for thorough examination e.g. cataracts, macular scarring, retinonlastoma & provide spectacles) orthoptic (cover good eye with patch), operation (resection and recession of rectus muscles, botox) Paralytic squints- due to paralyzed muscles 3rd nerve palsy o o o CF- down and out and out, ptosis (due to levator palpebral superiosis), proptosis, fixed and dilated pupil, aniscoria (different-sized pupils) Causes- PCAneurysm- unless proven otherwise/ microvascular ischaemia (DM, HTN)- will spare pupil Mgmt- refer to neurosurgery, but ischaemic 3rd palsy- resolves in 3mnths. 4th nerve palsy o o CF- diplopia and unable to look down and out, ocular torticolii (tilted head). Causes- trauma, diabetes, tumour & idiopathic 6th nerve palsy o o o o CF- diplopia in horizontal plane and unable to look out Causes- tumour (increasing IOP), trauma to base of skull, MS. Mgmt- botox, Pupils Physiology o o Light shown in on eye, travels along afferent CN2 (Optic nerve) to LGN (thalamus) on either side. From LGN, efferent travel via occulomotor nerve (CN3) to ciliary muscles to enable dilatation via sympathetic or constriction via parasympathetic. Afferent defects o o o o RAPD on light swinging test aka Marcus Gunn pupil. CF- on swinging test, affected eye shows consensual response but not direct response therefore afferents affected. Constriction to accommodation still occurs Pathway-light, optic nerve, pre-tectal nucleus of mid-brain- EWN – to both ciliary muscles via oculomotor. Causes- optic neuritis, optic atrophy, retinal disease Efferent defects o o 3rd nerve- thus same as before Causes- cavernous sinus lesion, superior orbital fissure syndrome (fracture of SOF ), diabetes or PCA aneurysm. Horner’s syndrome o o o o Disruption of sympathetic fibres CF=unilateral facial anhydrosis, partial ptosis and miosis Congenital Horner’s – iris heterochromia Causes- Pancoast tumour (subset of lung cancers- in pleural apex, affecting brachial plexus= pain, in shoulder & ulnar nerve distribution or arm & hand, upper limb wasting, can affect LEFT recurrent laryngeal=hoarse voice), MS, aortic aneurysm, mediastinal masses. Holmes-Adie pupil o o o o o Def- infection affecting pogstganglionic of parasympathetic. Initially unilateral then bilateral pupil dilatation with delayed response to near vision effectto Typical – young woman, sudden blur of near vision, dilated pupil, slow to accommodation, esp to light (looks unreactive unless >15min intense light) I- Slit lamp= wormy movements of iris (iris streaming ), tonic pupil Holmes-Adie syndrome= absent knee/ankle jerks, tonic pupils and low BP Argyll-Roberton pupil o Causes- neurosyphyllis and DM- o o CF= bilateral miosis, pupil irregularity (they are both small but different sizes) and no response to light, but response to accommodation fast aka Prostitutes pupils accommodates but does not react. I- spongy iris, pupil dilates poorly (parasympathetic affected) and maybe ptosis. Other causes of fixed dilated pupils o Mydriasis, trauma (blow out fracture)= acute rise in orbital pressure, can fracture thin Inferior and medial walls= oedema, muscle entrapment & nerve damage=diplopia, acute glaucoma, coning. N.B Ddx for diplopia= Ocular myositis (inflame disorder of 1/more EOMs, superior and inferior mostly affected, CF=diplopia with pain (pronounced on muscle involved), diagnosis with CT/MRI=muscle thickening, mgmt.=immunosuppression), MG (autoimmune neuromuscular – autoantibodies to Ach, CF=ptosis (bilateral & variable increasing with fatigue) & diplopia, facial & proximal muscle wasting, dysphagia & dysponoea. Ass=thymomas, I= Ach R antibody, antistriated muscle antibody & Tensilon test, ice pack placed for 2min improves ptosis. Mgmt= oral anticholinesterase= pyridostigmine ) Iris Sectorial Iris heterochromia o DDx- normal variant, herpes simplex opthalmicus, Waardenburg syndrome Type 1 – AD (snhearing loss, pigmented abnormalities of hair and skin and dystopia canthorum (wide nasal bridge)) Refraction o o o Dependent on eye ball length and medium Cornea 2/3, iris 1/3 Normal eyeball length = ~2.5cm Myopia o o o o Short sightedness – due to large eyeball, therefore focussing before hitting the retina, requiring concave lenses. Genetic 18P, 12Q; rarely born myopic, develops by 6, settles at late teens, if it continues increases risk of cataracts. Environ- thought to do with increased exposure to close range in early life and mRNA and [MMP] Mgmt- glasses, contacts, LASIK. Eye tests every 6 months when young. Pathological myopia o Rare <3% o o >6doipoters even >20dipoters Comp- secondary degeneration leading to retinal detachment, choroidoretianl atrophy and macular bleeding. Hypermetropia o o Long sightedness due to short eyeball thus focusing beyond retina, n eed convex lenses CF- tiredness of gaze, convergent squints in children N.B. Emmetropia = normal refractive power N.B. Amblyopia= lazy eye – with no organic cause/ strabismus – if in children must be correct <6 Astigmatism o o o Distortion in horizontal/vertical planes due to asymmetry of curvature of cornea/lens Can exist on its own + hypermetropia or + myopia Mgmt= toric lenses Presbyopia o o o Young lens are able to accommodate within 0.35sec Ability decreases due to stiffness of lens by 40years and is complete by 60 years Requires reading glasses. VF defects Assessment o o o o Tests o o o Unilateral/Bilateral Are borders clear Vertical/horizontal plane Acuity? Amsler grid – central vision at 30cm, appears distorted (metamorphosia) if maculopathy Finger confrontation Hat-pin confrontation Causes o Ischemia (stroke, TIA, migraine) o Tumour o AV malformation o Abscess o Drugs P.M. PITS- also craniopharyngioma affects optic chiasm Superiorly= inferior/lower quadrant defect, whereas pituitary tumour affects optic chiasm Inferiorly= superior/upper quadrant defect. The red eye Acute closed angle glaucoma o o o o o o Aqueous humour produced by ciliary body and drained via canal of Schlemm. Acute closed- reduced drainage due to blockage, raised pressure=ischemia= corneal, iris & retina CF= red painful eye, corneal haze/glare (corneal oedema), fixed & dilated pupil, IOP increases form 15-20mmHg to >40mmHg, n&v (abdo pain), reduced vision, corneal oedema (Must be reduced <4hrs to prevent irreversible visual damage) O/E- close both eyes, the one affected is tender & harder Typical- middle aged, night time or dark room, dilated pupil, >40, female & hypermetropic Mgmt- analgesia & antiemetics, pilocarpine (2-4%), timolol-non-selective beta blocker (topically), acetazolomid (carbonic anhydrase inhibitor 500mg IV- due to N&V), mannitol and finally peripheral iridectomy (at 12o’clock position in both eyes-so that eyelid covers defect in iris & prevents scattering of light) Anterior uveitis (acute iritits) o o o Uvea= ciliary body, choroid and iris thus anterior refers to inflame of ciliary body and iris Ass= AS, sarcoidosis, IBD, Behcet’s, reactive arthirits & ocular trauma. CF= acute pain, photophobia, acuity decreased, normal pressure, blurred vision, small pupil initially then irregular or dilates due to adhesions (synechiae) o o o o o/e=redness around limbus(ciliary flush) I- Talbots test- pain on finger confrontation & slit lamp= white ppt (floating infalm cells & flare-protein exudates), sometimes sterile (hyopyon) Mgmt- cycloepentolate (topical mydriatic- relieve ocular pain) to prevent synechaie (adhesions) and ttt with prednisolone every 2hrs to reduce inflam. Comp=cataracts & 2o glaucoma N.B- Posterior uveitis- minimal pain, photophobia but mainly complain of visual blurring & floaters. N.B. Systemic investigations- if bilateral, granulomatous or recurrent. Conjunctivitis o o o Causes; bacterial (purulent discharge),viral (infectious adenovirus & prodrome= sore throat, low-grade fecer & myalgia) or allergic (giant/cobblestone papillae). CF- bilateral with discharge, red, hyperamic vessels that can be moved over sclera. Acuity NOT affected. Eyes burn, itch & lacrimate. Discharge can stick lids together TTT – bacterial – chloramphenicol (topical broad spectrum), allergicantihistamines (emedastine) N.B Neonatal conjunctivitis/ophtlamia neonatarum – 1st 28days of life. CF=bilateral discharge & eyelid oedema Corneal abrasion o o o o Breach of epithelium, occurs without keratitis, e.g. trauma CF=pain, photophobia, blurred vision I- fluroresein 1% (orange drops turn green on blue dye if epithelial breach ) Ttt- chloramphenicol N.B. Penetrating eye injury= early closure of corneoscleral laceration with Abx as delay= endopthalmitis which if severe=blindness. Corneal ulceration o o Causes; bacterial, fungal or viral or from vasculitis Mgmt- gentamicin & cefuroxime/ ofloxacin but do corneal scrape and mc& s for blood agar and chocolate agar (Haemophilus B & N. menin) and liaise with microbiology. N.B. Bacterial keratitis- S.aures, Strep & pseudomonas. But N.gonorr, one of the few that can penetrate corneal epithelium. Predisposing; contact lenses, trauma, blepharitis & immunosuppressant. Bacterial keratitis=permanent corneal scarring, corneal thinning & perf, mgmt=corneal grafting. Episcleritis o o o o o o Inflam below conjunctiva – inflam nodule More common than scleritis but not as painful/or life threatening Blood vessels engorged look blue (segmental hyperemia) & are movable. CF= aches, tender, acuity ok Ass=RF, PAN/SLE Mgmt- topical vasoconstrictors (phenylephrine), but usually self-limiting NOT Scleritis o o o o o SOS50% - bilateral, middle-aged women CF=v. painful and engorged bv (entire sclera), oedema of conjunctiva with scleral thinning (risk of perf), acuity rarely affected Ass- connective tissue disorders (RA) & HZO Mgmt-oral NSAIDS but if severe; topical& `systemic corticosteroids or immunosuppressive. Subconjunctivial haemorrhage o o Self-limiting but alarming I- BP check Sudden PAINLESS loss of vision Questions o o o o Onset <6hrs requires imm ttt Headaches Pain on eye movements Co-morbidities – control Anterior ischemic optic neuropathy o I- fundscopy shows pale/swollen optic disc o Arteritic o 5-10% o Optic nerve damage due to posterior ciliary artery blockage (inflammation, atheroma or emboli, e.g. GCA(medium to large sized arteries)) o Due to thromboembolism in artery o CF- malaise, jaw claudication, pulseless temporal artery, tender scalp/unilateral headache & neck pain o N.B. systemic signs; fever, myalgia, malaise, reduced appetite and loss of weight o I- ESR and CRP increases, temporal artery biopsy o o/e= swollen disc & flame hameorrages o o Mgmt- prednisolone to stop blindness, may require up to a year. Non-arteritic- Atherosclerosis o 90-95% o Causes- DM, HTN, increase in lipids and smoking. o Modify factors to prevent other eye being affected o Histology=necrosis & apoptosis at level of photoreceptors Vitreous haemorrhage o o o o o Leakage of blood from retinal vessels, new vessels (diabetic proliferative retinopathy), branch, central retinal vein/artery, retinal tear, retinal detachment, trauma etc Comps- retinal detachment CF if small= floaters/spots if moderate= red dots/no red reflex I- B-US helps exclude retinal detachment. Mgmt- spontaneously absorbed, might require vitrectomy if large. In DM- wait 3mnths post photo-coag. Posterior vitreous detachment Retinal detachment Dense shadow that Flashes of light starts peripherally (photopsia) - in the progresses towards the peripheral field of central vision vision A veil or curtain over Floaters, often on the field of vision the temporal side of Straight lines appear the central vision curved Central visual loss Vitreous haemorrhage Large bleeds cause sudden visual loss Moderate bleeds may be described as numerous dark spots Small bleeds may cause floaters Subacute loss of vision- optic neuritis o o o o o o Unilateral loss of acuity, can take hours or days CF- RAPD, red desaturation, pain on eye moments (In RBN, optic nerve sheath compresses the optic nerve), also central scotoma. CF= 60%-normal, swollen- 23%, 18%-hyperaemia & blurred with peripapillary haemorrhages -2%. Recovery over 2-6wks - 45-80% will have MS <15years Mgmt- methylprednisolone for 3 days followed by oral corticosteroid for 11 days might delay LT disability Other causes- neurospyhillis, other demyelination, Leber’s optic atrophy, diabetes and vitamin deficiency, viral infections, vasculitis N.B Optic papilitis if optic head is affected & retrobulbarneuritis (RBN) if optic nerve affected posteriorly. In RBN- acute stage looks unaffected, with optic atrophy occurring mnths later, in papillitis – optic disc swelling. N.B. Papilledema= bilateral optic disc swelling = blurring of the optic disc margins & venous engorgement. Transient loss of vision o o o o Ischaemic (stroke, migraine, TIA) MS Subacute glaucoma Papilloedema. Central retinal artery occlusion o o o o o Not as common as CRVO; can affect central/branch Thromboembolic cause; check BP, DM, HTN, (CVD-carotid and valves) CF= CF-90%, RAPD(sec) I- pale fundus, cherry red spot Mgmt- <90minutes =required increasing blood flow to retina, ocular massage, removed aq fluid from anterior chamber (paracentesis) and anti-HTN agents/LT-antiplatelet therapy/carotid endarterectomy. Central retinal vein occlusion o o o o o o o Increases with age and is more common than CRAO CF=CF I- Fundoscopy- tortuous dilated vessels, optic nerve swelling (papilloedema) and retinal haemorrhages (diffuse flame shaped1) RF- DM, HTN, old age raised IOP, smoking & lipids. Types; ischemic (cotton wool, RAPD-if severe case) and non- ischemic LT outcome form 6 months to 1 year; macular oedema and iris neovacualrisation (IRIS RUBREOSIS) = <100 day neovascular glaucoma (RUBREOTIC GLAUCOMA). TTT of neovascular glaucoma – aggressive pan-retinal laser photocoagulation/intravitreal injection of anti-VEGF Branch retinal vein occlusion o o o o o Unilateral vision loss, Retinal ischaemia leads to VEGF TTT of neovascularisations - photocoagulation TTT of macular oedema- grid pattern argon laser photocoagulation (+/arterial crimping) o/e= produces haemporrgahe & vessel tortuosity & corresponds with VF Gradual loss of vision Charles Bonnet syndrome o Visual hallucination, elderly, with gradual loss of vision Chroiditis (choroidoretinitis) o o o o o Inflam of choroid by orgs leading to granulomatous appearance Toxocara, toxoplasmosis>sarcoidosis and TB I- CXR, Mantoux test, serology Mgmt- dependent on orgs Acute phase- blurred vision, grey/white raised patch, vitreous opacities and cells in A chamber & Late phase- choroid retinal scar Choroid melanoma o o o Common malignant tumour Grey/black mottled appearance with haematogenous spread or orbital spread/raised brown fundal mass Mgmt- enucleation, irradiation, photocoagulation, microsurgical resection. Age related macular degeneration o o o o o o Chief cause of blindness in UK Elderly affecting central vision Types; Wet (chroroidal new vessels, showing fluid exudation) and Dry (drusen and degeneration at macular, usually both eyes affected, atrophy & retinal pigment epithelial changes) Mgmt WET > DRY. Wet- photodynamic therapy, laser and intravitreal anti-VEGF. Wet has the worst prognosis. Advise to quit smoking and increase green veg Optic atrophy o o o I- pale/swollen optic disc Causes increase in IOP, Paget’s disease of skull, retinal damage, ischemia Causative; tobacco, methanol, lead, arsenic, quininine. Optic nerve drusen o o Abnormal metabolism leads to build up calcium in mitochondria, exudation = calcified mitochondria I- optic disc irregular, lumpy yellow matter, no optic cup and abnormal branching patterns of vessels. Chronic simple (open angle) glaucoma o o o o o Asx until VF affected, as central vision intact therefore late presentation and irreversible optic nerve atrophy >21mmHg requires yearly screen = optic disc cupping, nerve damage, scotomata near blind spot. Nasal and Superior fields are lost first (temporal last) >0/4 cup to disc=glaucoma. Fundsocpy= pale optic discs (atrophy), cup widens and deepens, so blood vessels appear to have breaks as they disappear into the cup(sharp turning=bayoneting) RF o >35, (+)ve Fx, Black, myopia, diabetic/thyroid eye disease. – raised IOP, only indicator of pressure thus lowering prevents glaucoma. Tests o o o VF screening Optic disc ratio/cupping – 0.4-0.7, >0.9=severe IOP Drug ttt- reduce IOP by 30% baseline o o o o o o Prostaglandin analogues (latonprost)- increase uvealscleral drainage SE: long eye lashes, changes to pigmentation of iris and around eye, pruritus and irritation B blocker- timolol – decrease production of aqueous. SE- dry eyes, low exercise tolerance, allergy. CI- asthmatics and heart failure A-adrenergic blockers- brimonidine- increase drainage and decrease production of aq humour. SE-lethargy & dry mouth. Miotics- pilocarpine- increase aq flow drainage SE-miosis, brow ache and reduced acuity. Carbonic anhydrase inhibitors- acetazolamide – decrease production of aq humour. SE: dyspepsia, low K+, paraesthesia. CI-pregnancy. Sympathomimetics- dipivefrine – CI heart disease, high BP & closed angled glaucoma. SE, red eyes/low vision, sore. Surgery if drug ttt fail o o o Trabeculectomy- to increase drainage into a conjunctival bleb. Comp= early failuire, hypotony, bleb leakage, infection Argon laser trabeculoplasty- short-term. Cataracts o o o o o Measure fasting bm Worldwide top cause of blindness, then vitamin A def, trachoma and onchichoreisis. Opacification of lens- leukoria if mature, Can be congenital >75% of >65 & 20% of 45-65 yr olds. o o Avoid high oxidative stress e.g. smoking. Different types; o Christmas tree/dot (dystrophia myotonica), o nuclear cataracts (old age) o Corticol/spoke like/wedge (old age) o Anterior and Posterior pole (localized and inherited, lie in visual axis) o Subcapsular (steroid use & deep to lens capsule ) o blurred vision, gradual vision loss +/- frequent spectacle changes, dazzling in bright lights and may cause mononuclear diplopia. Children- squint, loss of binocular function, leukoloria, nystagmus. Pinhole can improve visual acuity, as blurred vision due to refractive error CF Surgery o o o o o o o o Temp relief- mydriatic drops, sunshades but if affection lifestyle & cannot read 67 feet for driving then surgery. Risk of surgery- 2% serious Day case under LA- involves small slit at limbus, phaecoemulsification (broken by US) of lens contents (via cannula), placement of artificial lens capsule (foldable). P lens remains and can thicken, 5-30% opacifies= return of cataract, a small hole is made using a YAG laser. Comp= A uveitis, retinal detachment, VH, glaucoma = permanent visual loss. Post-op bacterial endopthalmitis- rare comp- proptosis & restriction of eye movement 2o to enlargement of EOM (cf=poor vision, pain & significant inflammation <2wks of surgery. Fundoscopy= obscured by vitritis) After phaeco- normal activities can assume the following day Abx & anti-inflam drops for 3-6weeks post-op. Comps- P lens rupture, dry/gritty eyes (Viscotears) The retina o o Consists of 2 layers; neurosensori retina and pigmented retina. Macular 5mm, contains fovea, fovea centralis- high concentration of cones – for visual acuity Optic disc o Note colour(pink), cup (0.4-0.7) and contour (ovoid in astigmatism) & 2:3 A:V ratio. Retinal detachments o o o P- rhegmentous – rhegma is a break in epithelium e.g. retina tear leading to fluid accumulation that results in the separation of retina (neurosensory from RPE= accumulation of vitreous fluid in subretinal space), secondary to intraocular prob, post cataract surgery. Increased risk in myopics – esp post cataract surgery. 4 F’s= flashes (50%), floaters, field defects & fall in acuity CF- curtain falling down (SUDDED PAINLESS), if superior falls down then inferior fields lost, red eye reflex lost. If macula affected= no central vision. o o o I- ballooning, grey effect. On slit lamp= Shafer’s sign (floating pigment cells in the in A vitreous) Mgmt- vitrectomy, gas tamponade (silicon oil) silicon lens implant. Cryotherapy/laser coag secures retina. Post-op re-detachment – 5-10% Prognosis- if macular detachemed >24hrs = full recovery unlikely. Retinitis pigmentosa o o o o Inherited, usually AR, but AD has best prognosis, X linked has worst prognosis. CF= Funnel (aka tunnel) vision, worse at night, at 20 some have <6/60 and by 50, some have ability to read (25%). O/E= black bone spicule-shaped pigmentation, mottling of retinal pigment epithelium. Ass; Refsum disease (cerebellar ataxia, peripheral neuropathy, deafness, ichthyosis/fishy-scale), usher syndrome (SNHL), Alport syndrome (different types) Toxoplasma o o Intracellular protozoan I-bilateral punched out holes, heavily pigmented chorioretinal scars & if macular affected, decrease in acuity. Macula Macular holes o o Full thickness defect of retinal tissue, involving fovea = decreased acuity. 3/1000 >55yrs, 12% chance of other eye being affected Presentation o o Distorted vision with visual loss. Tiny punched out area centre of macula – yellow white deposits at base o Slit lamp= semi-translucent area over hole= grey halo of detached retina I Causes o Idiopathic. Age-related shrinkage of perifoveal vitreous cortex, traction on fovea, detachment and macula holes. Displacement of fovea- underlying xanthophyll pigment. Stages o o o o 1=yellow spot at fovea; yellow donut shaped ring. Vision usually good, 50% progress to 2. 2=<400nm. Full thickness macula hole, with cuff of subretinal fluid. Vision reduced with image distortion. 3=>400nm, with localizd separation of vitreous cortex. 4= complete hole with vitreous seperation from entire macula and disc Tests o o o Amsler grid OCT FA Mgmt o o o o o Stage 1- wait and see may resolve spontaneously/ Vitrectomy, creating an air bubble (tamponade)- Pt lying on face 1-2 wks post-op. <95% closure rates. May require additional surgery Comp= RD, iatrogenic retinal tears, enlargement of hole. <2 years many develop cataracts. The eye in DM o o o <150/85 will prevent DM retinopathy Cause of blindness – 20-65 30% have ocular problems at presentation. Structural o Diabetes accelerated glycsolication- increases sorbitol via aldose reductase – age-related cataracts, Patho o o o o o o Micorangiopathy in capillaries, precapillary arterioles and venules cause occlusion +/leakage Vascular occlusion leads to new vessels forming on choroid, retina, iris- VH = proliferative DMR New vessels are fibrous leading to traction- retinal detachment Occlusion also causes cotton wool spots (ischaemic nerve fibres) Vascular leakage- as pericytes are lost, capillaries bulge (micoraneurysms) Oedema and hard exudates (lipoprotein & lipid filled macrophages) o Rupture of micro aneurysm – flame shaped haemorrhages – deep= blot haemorrhages. Classification o o o o Before; background, pre-proliferative and proliferative +/- maculopathy Now – non-proliferative diabetic retinopathy classed as mild, moderate and severe, can become sight threatening proliferative DMR Proliferative DMR- fine new vessels appear on optic dsic, retina =VH (more common in DM1, 50% blind in 5 years) Maculopathy mapped; foveola, foveola centralis, parafoveal and perifoveal. Leakage from vesssels= macular oedema & threaten vision. (More common in DM 2) Traditional classification New classification Mild NPDR Background retinopathy microaneurysms (dots) blot haemorrhages (<=3) hard exudates Pre-proliferative retinopathy 1 or more microaneurysm Moderate NPDR microaneurysms blot haemorrhages hard exudates cotton wool spots, venous beading/looping and intraretinal microvascular abnormalities (IRMA) less severe than in severe NPDR cotton wool spots (soft exudates; ischaemic nerve fibres) > 3 blot haemorrhages venous beading/looping deep/dark cluster Severe NPDR haemorrhages more common in Type I DM, blot haemorrhages and microaneurysms in 4 treat with laser quadrants photocoagulation venous beading in at least 2 quadrants IRMA in at least 1 quadrant Treatment o o o Control of bm & treat co-morbidities Photocoag by laser- treat maculopathy (grid/focal) and proliferative retinopathy (panretinal)- scatter laser >1000 applications may require 2 sessions. N.B. Pan-retinal does not improve vision, prevents blindness. VH- viterectomy Ocular palsies o o Argyll-Roberstons & Horners (topical 4% cocaine will only dilate normal eye, due to cocaine blocking the re-uptake of NA, in Horner’s, NA is not secreted thus no effect. Ddx= Pancoast tumour of lung) 3rd & 6th Tropical eye disease Trachoma o o o Chlymydia trachomatis – one of the causes of blindness Spread by flies, related to cattle Prevention- face washing & good water/sanitation. Staging o o o o 1- Lacrimation, follicles in the upper lid show granular appearance 2-erythema, larger follicles and both lids affected. Pannus of capillaries grow towards cornea 3-scar tissue as follicles rupture & pannus more advanced. 4- inversion of eyelid and irritation by eyelashes. Cornea may ulcerate. Mgmt o o o o Mass anti-trachoma treatment – tetracycline 1% eye ointment 12hrly- for 5 days each month for 6 months. Active disease, tetracycline 250mg.6h po for 14 days & 8hrly for 6 weeks. Single dose azithromycin in children is 78% effective in children. Surgery- e.g. lid margin splitting + tarsal plate fracture +everting sutures Onchioresiss/ river blindness o o o o o o Microfilarea of namtode onchocero volvulus, transmitted by black flies of Simulim species, 95% Africans affected Unless eyes affected, most confined to skin Fly bites =nodules which microfilarea released, invade structures of eye, Investigation- dead or swimming/ floating in Anterior Microfilarea cause inflame, then fibrosis occurs around them, reaction causes cornal opacitis (nummular keratitis ) Chronic iritis = synechia & may ppt cataracts, with iris becoming totally fixed. Tests o Skin-snip tests, triple antigen serology, PCR. Mgmt o Ivermecting- single dose every 6-12monts till adults die aka macroflirae (lympathic system) Xeropthalmia & keratomalacia o o o o o o o o o Vitamin A deficiney, 2-5yrs. Night blindness & dry conjunctivae Cornea unwettable & loses transparency Bitots spots (small grey plaques) raised from interpalpebral conjunctivia Vit A reverses changes Early corneal xerosisi reversible. Keratomalacia- softening of cornea, +/- perf and extrusion of intraocular contents. Mgmt- retinol palmitate or retinyl palmitiate Avoid vit A in pregnancy. Blindness and partial sight Causes o o o o o o o Trachoma Cataracts Glaucoma Keratomalacia Onchooreciases. DMR Irreversible and in developed coutnries = age-related macular degeneration The Law o o Registrable <3/60 or >3/60 with reduced VF Partially sighted = <6/60 or >6/60 with VF Colour blindness o o o o Red/green mostly sex linked 8 in males & 0.5 in females Blue-yellow acquired, 1:1 Ischiara 16 plates Monochromatism- due to born without cones, were all cones contain same visual pigment. Drugs in the eye o Eye unable to retain drops, every 5 min between drops & hold 2hrly Mydriatic o o o o Tropicamide- every 3hrs Cyclopentoalte- 24hrs- prevents syncheia, as it’s a cycloplegic =blurred vision, don’t drive Not to be used is acute close angle glaucoma Miotics o o Pilocarpine = reduces acuity, parasympathetic sweating, brow ache due to ciliary spasm, flue-like syndrome, sweating, urinary frequency, dyspepsia. Local anaesthetics o o Tetracaine – abolishes cornel reflex In children- proxymetacaine (less stinging) Steroids & NSAIDs o Increase IOP and may progress dendritic ulcer so beware Iatrogenic eye disease o o Glaucoma may be ppt by steroid use, some mydriatic and anti-cholinergics (e.g. antiparkinson’s and TCAs) Ethambutol stains contact lenses and any visual SEs should be reported. Contact lenses o o o o o o o o o o 80% wear cosmetic Medical reasons to -12 in hypermetropia. >+10 in myopia & keratoconus (degenerative condition with blurred vision the only symptom) Hard lenses 8.5-9mm Gas permeable – may mist up during the day Soft- lenses – 4 wks then disposes Toric- astigmatism Extended wear lenses can be worn up to 4 months. Hard lenses – 2 solution one for cleaning & one for storage SE= corneal ulcers/abrasion, giant papillary change, to mucoprotein in lenses & keratoconjunctivities Mgmt of pseudomonas cornal ulcers- oflaxacin Miscellaneous CMV Retinitis Affects immunocomp (e.g. post renal-ttt) CF= yellow-white retinal necrosis & haemorrhage (pizza pie) Choroidal neovascularization Greyish lesions beneath the macula Leakage of bllodd/fluid= acute onset of central visual loss due to photoreceptor damage.