* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular Toxicology
Survey
Document related concepts
Transcript
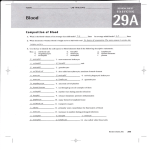
Introduction to Toxicology EV 460/660 & BI 460/660 Fall 2014 Toxic Effects on the Cardiovascular System Overview of Cardiovascular System Structure and Function 1. Structure – a pump (heart), series of flexible tubes (blood vessels), and a working fluid (blood) 2. Functions – transport (gasses, nutrients, wastes, chemical messengers), pH balance, osmotic regulation (water and electrolyte balances), bodily defense, hemostasis, hormone production, thermoregulation Brief Review of Blood 1. Composition – plasma and formed elements (RBCs, WBCs, and platelets/thrombocytes) 2. Plasma – water, proteins (albumins, globulins, fibrinogen), nutrients, and electrolytes) 3. Hematopoiesis – bone marrow, pluripotent stem cells, poietins (colony-stimulating factors) 4. RBCs – O2 & CO2 transport, pH buffering, hemoglobin, brief life span, anucleated 5. WBCs – granulocytes vs. agranulocytes, phagocytes vs. immunocytes 6. Platelets – hemostasis 7. Formed element general pathological suffixes – “-cytosis” = abnormally high level, “-penia”= abnormally low level, toxic effects usually result in abnormally low levels Toxic Effects on the Blood (hematotoxicity) 1. Effects on plasma proteins (albumins & fibrinogen) – to be covered under hepatotoxicity 2. Effects on globulin plasma proteins and lymphocytes – to be covered under immunotoxicity 3. Granulocytopenia – typically drug-induced (rather than toxin/toxicant action), ex. phenothiazines, non-steroidal anti-inflammatory compounds 4. Thrombocytopenia – typically drug-induced (rather than toxin/toxicant action), ex. quinidine, phenacetin, myelosuppressive anti-cancer drugs 5. Pancytopenia – (all formed elements) – due to severe damage/destruction of bone marrow, often toxin/toxicant induced, ex. ionizing radiation, benzene, lindane, chlordane, nitrogen mustards, arsenic 6. Anemia – general definition – reduced oxygen-carrying capacity of blood -- many types and many causes (drug, toxin/toxicant, nutritional, hereditary, or secondary to other pathophysiology) -- generally due to decreased (or defective) RBCs and/or decreased hemoglobin 7. RBC number – a balance between rate of production and rate of destruction 8. Decreased rate of production of RBCs -- aplastic anemia – direct damage to bone marrow, benzene -- nephrotoxic -induced anemia -- ↓ erythropoietin secondary to toxic actions of Hg or Cd 9. Increased rated of destruction or shortened life span of RBCs -- direct hemolytic effects – ex. saponin, phenylhydrazine, arsine, naphthalene -- shortened RBC life span – ex. Pb, Hg 10. Impaired hemoglobin synthesis – ex. Pb 11. Hypoxia -- general definition of hypoxia – inadequate O2 levels, maybe due to ↓ O2 levels in inspired air, maybe secondary to cardiovascular, pulmonary, or neural pathophysiology 12. Chemically-induced hypoxia -- maybe at cellular level of O2 utilization – see cyanide and ETS under cellular mechanisms -- maybe due to alterations in O2 transport by hemoglobin – a hematotoxic effect 13. Impaired O2 transport by hemoglobin -- carboxyhemoglobinemia – CO binding to hemoglobin -- methemoglobinemia – oxidation of heme, Fe2+ → Fe3+, primarily nitrates → nitrites, but also some organic compounds, adult vs. infant susceptibility Brief Review of Heart Structure and Function 1. Trilaminar -- endocardium, myocardium, epicardium/pericardium 2. Atria – ventricular differences, right – left differences 3. Intracardiac valves 4. Contractile cardiocytes – functional syncitium, intercalated discs, roles of Ca2+ 5. Intrinsic pacemaker system – components, automaticity 6. 7. 8. Autonomic innervation – sympathetic vs. parasympathetic effects Medullary cardiac control center; peripheral receptors (baroreceptors) Hormone production -- ANF Toxic Effects on the Heart (cardiototoxicity) 1. Toxicity may result from direct (heart) and/or indirect (ex. CNS, renal, endocrine) effects 2. Direct effects may include alterations in: cell membrane lipids, cell membrane proteins (ion channels and second messenger enzymes), cell membrane excitability, cellular energy metabolism, and essential ion availability 3. Secondary negative impacts of decreased cardiac function -- decreased blood flow (ischemia) -- decreased O2 (hypoxia) and nutrient delivery to cells -- decreased removal of metabolic wastes -- decreased removal of toxicants/toxins and metabolites 4. General classes of cardiotoxic compounds (one proposed organization) -- pharmaceutical agents – sympathomimetics, antibacterial aminoglycoside antibiotics, anthracyclines and other anti-neoplastic agents -- industrial chemicals – industrial solvents (toluene, halogenated hydrocarbons, ketones, glycol ethers) with multiple mechanisms of toxicity; and heavy metals (Cd, Pb, Co, As, Hg) -- endogenous and natural products – steroid hormones (and synthetic analogs) and cytokines, many animal and plant toxins 5. Cardiotoxic effects include alterations in heart rhythm, alterations in heart contractility, and death of heart cells (cardiac myopathy) 6. Arrhythmias – irregular heart rhythms (numerous types) -- tachycardia, bradycardia, fibrillation, ectopic beats -- may result from direct and/or indirect effects -- direct effects often due to changes in membrane excitability, ion channels, ion availability 7. Decreased contractility -- may result from direct and/or indirect effects -- direct effects often due to changes in energy metabolism, ion channels, ion availability -- maybe secondary to cardiac myopathy -- may lead to congestive heart failure 8. Cardiac myopathy -- often result from direct effect, often due to altered energy metabolism -- leads to congestive heart failure Brief Review of Blood Vessel Structure and Function 1. Pulmonary vs. systemic circulation 2. Types of blood vessels (arteries, arterioles, capillaries, venules, veins) 3. Trilaminar structure of large & medium vessels – tunics 4. Artery vs. vein vs. capillary structure 5. Resistance, flow, pressure relationship 6. Vasomotor changes – vasodilation vs. vasoconstriction 7. Pressure changes – hypertension vs. hypotension Toxic Effects on Blood Vessels (vasculotoxicity) 1. Degenerative changes to blood vessels – atherosclerosis A Descriptive pathology of atherosclerosis - plaques B. Effects of atherosclerosis on blood flow, blood pressure, risk of blood clots C. Risk factors D. Potential adverse effects E. Hypotheses for etiology (see figures) F. Toxicants associated with development of atherosclerosis 2. Pressor effects of toxicants A. Indirect, non-cardiovascular effects of poisons on blood pressure/volume B. Indirect, cardiotoxic effects on blood pressure (both direct & indirect actions on heart) C. Systemic reactions to toxins/toxicants affecting blood pressure – histamine D. Vasculotoxic agents promoting 1. hypotension 2. hypertension