* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Polymerase Chain Reaction as a Diagnostic Tool for Detecting
Zinc finger nuclease wikipedia , lookup
DNA sequencing wikipedia , lookup
DNA replication wikipedia , lookup
DNA profiling wikipedia , lookup
DNA nanotechnology wikipedia , lookup
DNA polymerase wikipedia , lookup
United Kingdom National DNA Database wikipedia , lookup
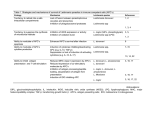
Brief Report Polymerase Chain Reaction as a Diagnostic Tool for Detecting Leishmania M. Brecelj, F. Pikelj, F. Gubenšek, G. Anderluh Summary Polymerase chain reaction (PCR) has been used to identify a Leishmania parasite in a cutaneous ulcer from a 27-year-old patient infected during travel in Peru. The available classical diagnostic methods could not confirm the diagnosis in a sufficiently short time. Therefore, two sets of oligonucleotides were designed and with both of them fragments of the expected size were obtained. The sequence of the fragment derived from kinetoplast DNA corresponds to the Leishmania Viannia complex. Polymerase chain reaction has advantages over classical diagnostic methods, which makes it an important technique in those hospitals and clinical laboratories in Europe which lack standard diagnostic tests for Leishmania. Key Words Leishmania · Diagnosis · Polymerase chain reaction · Mini-exon · Kinetoplast DNA Infection 2000;28:111–113 Introduction Leishmaniasis is a parasitic disease, endemic in 88 countries around the world. It is estimated that about 350 million people are at risk of infection and that two million new cases of leishmaniasis occur annually. The disease has a wide range of clinical symptoms, cutaneous, mucocutaneous and visceral. Cutaneous leishmaniasis has been a recurrent problem for settlers and travelers in the tropical and subtropical regions of the Old and New World. Travelers, infected during the journey, usually develop a full clinical picture within a few months after they return home, when the disease is frequently misdiagnosed or recognized only after a delay. Furthermore, laboratories in areas where leishmaniasis is seldom encountered lack the appropriate diagnostic capabilities. Proper identification of the parasite species is important for the treatment and prognosis of the disease [1–3]. Standard diagnostic methods include direct microscopy, histological examination with Giemsa staining and immunohistochemistry, microbiological cultures and Infection 28 · 2000 · No. 2 © URBAN & VOGEL serological methods. In recent years the polymerase chain reaction (PCR) has been successfully introduced and proved to be a sensitive and powerful tool for determining the parasite species in visceral [4–7] and cutaneous [8–10] leishmaniasis. However, because of the lack of appropriate oligonucleotides and commercial kits, reports of successful diagnosis in clinical laboratories, especially in Europe, have been scarce. A patient with a cutaneous lesion was admitted to the Clinic for Infectious Diseases at the Clinical Centre, Ljubljana, Slovenia, 3 months after traveling to Peru. The clinical picture suggested a diagnosis of leishmanian ulcer. Since none of the quick diagnostic methods available could confirm the presence of the parasites, we tried to prove the etiology of the lesion using PCR. Two sets of oligonucleotides were used to amplify minicircle kinetoplast DNA (kDNA) and mini-exon gene from Leishmania DNA. Both sets of primers yielded products of the expected size. The sequence of the minicircle fragment was determined and confirmed the presence of kDNA of the Leishmania Viannia complex. The approach used is suitable for diagnosis in centers not equipped for classical diagnostic evaluation of leishmanial infections, since it is fast, easy to perform and does not need large amounts of highly purified DNA. Materials and Methods A 27-year-old patient was admitted to the Clinic for Infectious Diseases, University Clinical Centre, Ljubljana, Slovenia, 3 months after returning from a 3-month visit to Peru. He presented with a cutaneous lesion on his right shank, that began as a red papule at the M. Brecelj, F. Pikelj Clinic for Infectious Diseases, Clinical Centre, Japljeva 2, SLO-1000 Ljubljana, Slovenia F. Gubenšek Dept. of Biochemistry and Molecular Biology, Jozef Stefan Institute, Jamova 39, SLO-1000 Ljubljana, Slovenia, and Faculty of Chemistry and Chemical Technology, University of Ljubljana, Askerceva 5, SLO-1001 Ljubljana, Slovenia G. Anderluh (corresponding author) Dept. of Biology, Biotechnical Faculty, University of Ljubljana, Vecna pot 111, SLO-1000 Ljubljana, Slovenia; Phone: +386-61-1233388, Fax: +386-61-273390, e-mail: [email protected] Received: May 17, 1999 • Revision accepted: January 25, 2000 111 M. Brecelj et al.: PCR detection of Leishmania site of an insect bite and had gradually developed into a cutaneous ulcer measuring 7 5 cm in size. The lesion had been accompanied by painful enlargement of a regional lymph node over the previous 2 weeks. Direct examination of Giemsa-stained material, obtained by scarification of the ulcer edge, did not lead to a diagnosis. Biopsy specimens of the ulcer edge and the enlarged lymph node were cultivated on NNN medium for 3 weeks. The specimen from the ulcer edge yielded a growth of leishmanial parasites, while the lymph node specimen remained sterile. Enzyme-linked immunosorbent assay (ELISA) using antigens of Leishmania donovani was performed twice at an interval of 4 weeks.The serologic reactions were negative on both occasions. Parasite DNA was isolated from the cutaneous lesion, using SDS and proteinase K [11].A sample of approximately 5 mm3 was dissolved in Tris-EDTA buffer, pH 8.0. After extraction with SDS and proteinase K at 55 °C, the solution was phenolized twice and DNA precipitated with ethanol and sodium acetate.The pellet was resuspended in 50 µl of distilled water. In addition, a further 1-mm3 sample from the lesion was resuspended in 20 µl of 1 PCR buffer and 3 µl was used for amplification. Two sets of oligonucleotides were designed to amplify specifically Leishmania DNA. Oligonucleotides B1(+) and B1(–) were used to amplify the 131-bp fragment of the conserved part of minicircle kDNA from four New World species of Leishmania [8]. The second set of primers, composed of oligonucleotides B2(+) and B2(–), was designed to amplify a mini-exon repeat of Leishmania genomic DNA [9]. The sequences of the primers were as follows: B1 (+) (5'– gga att CCC GAC ATG CCT CTG GGT A–3'), B1 (–) (5'– cga att CAC TAT ATT ACA CCA ACC CCT A–3'), B2 (+) (5'– gga att cAC TTT ATT GGT ATG CGA AAC TTC–3'), and B2 (–) (5'– cga att CAG AAA CAG ATA CTT ATA TAG CG–3'). They all contained the EcoRI site (underlined). Regions of complementarity with Leishmania DNA are shown in capital letters. For PCR amplification 50 pmoles of each oligonucleotide, 4 µl of prepared sample and 2.5 units of Taq polymerase were used in a total volume of 50 µl in buffer supplied by the manufacturer (Perkin-Elmer). 30 amplification cycles were performed with denaturation at 95 °C for 1 min, annealing at 62 °C for 1 min and extension at 72 °C for 1.5 min. Products were analyzed on 1.5% agarose gels. The fragment amplified with oligonucleotides B2(+) and B2(–) was visible only after secondary PCR. For this, a small portion of primary PCR mixture, usually 2 µl (1/25 of primary PCR), was used. Fragments obtained after amplification with B1(+) and B1(–) oligonucleotides were further digested with EcoRI and inserted into pUC19, where their sequence was checked using a T7 sequencing kit (Pharmacia) and S35 ∞dATP (Amersham). exon is composed of a moderately conserved region, consisting of an exon and an intron, from 94–140 nucleotides in length, and a variable length spacer. Mini-exon amplification enables discrimination, according to the length of the amplified fragment, between different Leishmania parasites: New World Dermotropic (Viannia) (approximately 230 bp), New World Dermotropic (Leishmania) (approximately 300 bp), Old World Dermotropic and Old and New World Visceral species (approximately 410 bp). We obtained a fragment of approximately 230 bp (Figure 1) which clearly belongs to the New World Dermotropic species of the Viannia complex. This fragment was visible only after the secondary PCR. This is a consequence of the relatively low abundance of mini-exon DNA (100–200 copies per genome) in contrast to kDNA (up to 10,000 copies per kinetoplast), from which fragments were obtained readily in the first round of amplification. With the other set of oligonucleotides we amplified a part of the conserved minicircle kDNA. kDNA has been most often used as a source of Leishmania DNA for PCR diagnosis. It is found exclusively within large mitochondria called kinetoplasts and is composed of about twenty 20 kbp large circles and up to 10,000 copies of approximately 800 bp minicircles. The minicircle DNA is a suitable target for diagnostic PCR, due to its abundance [12]. De Bruijn and Barker [8] sequenced minicircle from four species of Leishmania (Viannia) braziliensis complex and derived oligonucleotides for use in diagnosis of parasites from this complex. On the basis of their data, we designed oligonucleotides B1(+) and B1(–) which enabled amplification of a 131-bp constant region of minicircles. The fragment obtained using these primers was of expected size. In addition, we determined the nucleotide sequence and found it to match the published sequence of L. (V.) braziliensis complex [8]. Further, we have shown that it is not necessary to use a common protocol of DNA isolation using proteinase K and phenol extraction [5, 11, 13]. As is evident from figure 1 (lane 2) the fragment was also obtained by simply resuspending a few µl of scarificate from the ulcer edge in 1 PCR buffer and using such a mixture for amplification. Results and Discussion PCR was employed to establish the presence of Leishmania in the skin ulcer of the patient. Figure 1 shows the results of amplification using the sample of Leishmania DNA from the patient. With both sets of oligonucleotides, fragments of the expected sizes were amplified with template DNA extracted by standard procedures [11]. To exclude contamination with the patient’s DNA the same conditions were used for amplification of human DNA. In this case, no products were observed (data not shown). The B2(+) and B2(–) pair of oligonucleotides was designed according to the sequence of the mini-exon repeat from the genome of Leishmania parasites [9]. The mini- 112 Figure 1 Amplification of Leishmania DNA. Using B1(+) and B1(–) oligonucleotides we were able to amplify a product of 131 bp with extracted DNA (lane 1) and DNA from the ulcer scarificate resuspended in 1 PCR buffer (lane 2). With B2(+) and B2(–) oligonucleotides the fragment of approximately 230 bp was seen only after the secondary PCR amplification (lane 3). M: molecular weight standards Infection 28 · 2000 · No. 2 © URBAN & VOGEL M. Brecelj et al.: PCR detection of Leishmania In conclusion, PCR-based identification has proved to be highly sensitive and easy to perform. This is particularly important for many hospitals and clinical laboratories in Europe, which seldom encounter cases of infection with Leishmania, because it enables rapid confirmation of the identity of the parasite in laboratories which are not equipped for standard diagnostic tests. Acknowledgments The authors would like to thank Dr. Roger H. Pain for his critical reading of the manuscript. This work was supported by a grant from the Ministry of Science and Technology of Slovenia. References 1. 2. 3. 4. Navin TR, Arana BA, Arana FE, Berman JD, Chajón JF: Placebocontrolled clinical trial of sodium stibogluconate (Pentostam) versus ketoconazole for treating cutaneous leishmaniasis in Guatemala. J Infect Dis 1992; 165: 528–534. Herwaldt BL, Bermann JD: Recommendations for treating leishmaniasis with sodium stibogluconate (Pentostam) and review of pertinent clinical studies. Am J Trop Med Hyg 1992; 46: 296–306. Olliaro PL, Bryceson ADM: Practical progress and new drugs for changing patterns of leishmaniasis. Parasitol Today 1993; 9: 323–328. Smyth AJ, Ghosh A, Hassan MQ, Basu D, de Bruijn MHL, Adhya S, Mallik KK, Barker DC: Rapid and sensitive detection of Leishmania kinetoplast DNA from spleen and blood samples of kalaazar patients. Parasitology 1992; 105: 183–192. Infection 28 · 2000 · No. 2 © URBAN & VOGEL 5. Osman OF, Oskam L, Zijlstra EE, Kroon NCM, Schoone GJ, Khalil ETAG, El-Hassan AM, Kager PA: Evaluation of PCR for diagnosis of visceral leishmaniasis. J Clin Microbiol 1997; 35: 2454–2457. 6. Qubain HI, Saliba EK, Oskam L: Visceral leishmaniasis from Bal'a, Palestine, caused by Leishmania donovani is identified through polymerase chain reaction and restriction fragment length polymorphism analysis. Acta Trop (Basel) 1997; 68: 121–128. 7. Noyes HA, Reyburn H, Bailey JW, Smith D: A nested-PCR-based schizodeme method for identifying Leishmania kinetoplast minicircle classes directly from clinical samples and its application to the study of the epidemiology of Leishmania tropica in Pakistan. J Clin Microbiol 1998; 36: 2877–2881. 8. de Bruijn MHL, Barker DC: Diagnosis of New World leishmaniasis: specific detection of species of the Leishmania braziliensis complex by amplification of kinetoplast DNA. Acta Trop (Basel) 1992; 52: 45–58. 9. Fernandes O, Murthy VK, Kurath U, Degrave WK, Campbell DA: Mini-exon variation in human pathogenic Leishmania species. Mol Biochem Parasitol 1994; 66: 261–271. 10. Osman OF, Oskam L, Kroon NCM, Schoone GJ, Khalil ETAG, ElHassan AM, Zijlstra EE, Kager PA: Use of PCR for diagnosis of post-kala-azar dermal leishmaniasis. J Clin Microbiol 1998; 36: 1621–1624. 11. Sambrook J, Fritsch EF, Maniatis T: Molecular cloning: a laboratory manual, 2nd edn. Cold Spring Harbor Laboratory Press, Cold Spring Harbor, New York 1989. 12. Englund PT, Hajduk SL, Marini JC: The molecular biology of trypanosomes. Annu Rev Biochem 1982; 51: 695–726. 13. Alexander B, Lozano C, Barker DC, McCann SHE, Adler GH: Detection of Leishmania (Viannia) braziliensis complex in wild mammals from Colombian coffee plantations by PCR and DNA hybridization. Acta Trop (Basel) 1998; 69: 41–50. 113