* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download presentation slides - New Jersey College Health
Ages of consent in South America wikipedia , lookup
Homosexuality wikipedia , lookup
Human female sexuality wikipedia , lookup
Sexual fluidity wikipedia , lookup
Sex in advertising wikipedia , lookup
Reproductive health wikipedia , lookup
Sexual attraction wikipedia , lookup
LGBT people in prison wikipedia , lookup
Sex reassignment therapy wikipedia , lookup
Gender dysphoria wikipedia , lookup
Heterosexuality wikipedia , lookup
History of human sexuality wikipedia , lookup
Ego-dystonic sexual orientation wikipedia , lookup
Female promiscuity wikipedia , lookup
Sexual ethics wikipedia , lookup
Sex and sexuality in speculative fiction wikipedia , lookup
Rochdale child sex abuse ring wikipedia , lookup
Gender dysphoria in children wikipedia , lookup
Gender roles in non-heterosexual communities wikipedia , lookup
Non-heterosexual wikipedia , lookup
Lesbian sexual practices wikipedia , lookup
Slut-shaming wikipedia , lookup
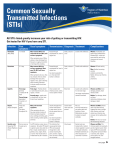
Care of LGBTQ Population in College Health Uri Belkind, MD Clinical Director, Health Outreach to Teens (HOTT) Callen-Lorde Community Health Center March 9, 2016 OBJECTIVES • Identify the particular health needs of LGBT college students. • Understand the importance of creating safe spaces and of the sexual history to recognize specific health needs of LGBT college students. • Discuss specific health services needed to provide comprehensive care to the LGBTQ population. Importance of this training • Both youth and the LGBTQ community are marginalized, which is associated with increased health risks. • Clinicians rarely receive training specific to LGBTQ youth. • Providing LGBTQ youth-competent care is a skill. Terms, definitions, acronyms… • LGBTQ: Lesbian, Gay, Bisexual, Transgender, Questioning/Queer • SOGI: Sexual orientation and gender identity – Sexual orientation and gender identity are two separate concepts and do not always “match” Sexual Orientation • Identity: a label – “I am…” • LGBTQ, pansexual, asexual… • Behavior: most clinically relevant – “I have sex with…” • MSM, WSW, MSWM, TFSM, TMSWM… • Attraction: doesn’t always align with above – “I like…” Sexual Orientation: Identity NYC YRBS 2013 Sexual Orientation: Behavior NYC YRBS 2013 Gender Identity GENDER IDENTITY SEX • CHROMOSOMES • ANATOMY Gender Identity GENDER IDENTITY SEXUAL ORIENTATION Gender Identity • Identity: a label – “I am…” • Male, Female, Transfemale/male, Genderqueer, GNC, Non-binary… • Expression: communication of one’s gender – “I appear and/or behave…” • Masculine, Feminine, Androgynous • Role: society’s expectations of each gender – “Be a man!”, “That’s not ladylike” • Masculine, Feminine, Neutral Sexuality is a Spectrum (And there are no “Should’s” or “Should not’s”) Case 1. WZ • 20yo Asian male • STI screening • Identifies as gay LGBT Health Disparities • Victimization • Homelessness • Mental health – – – – – Anxiety, Depression, PTSD Suicidality Eating Disorders Substance use High-risk sexual behaviors • ↓Education LGBT Sexual Health • MSM have higher rates of some STIs – Gonorrhea – Primary and secondary syphilis – HIV • WSW might have higher rates of: – Trichomonas – Bacterial vaginosis College LGBT Sexual Health (Compared to heterosexual counterparts) MEASURE LESBIAN BISEXUAL ♀ GAY BISEXUAL ♂ #partners = ↑ ↑ ↑ Oral Sex = = ↑ ↑ Vaginal Sex ↓ = ↓↓ ↓ Anal Sex ↓ ↑ ↑↑ ↑↑ Oral = = ↑ ↑ Vaginal ↓↓ ↓ = = Anal = = = = = ↑ ↑ ↑ Safer sex: HIV Test Oswalt. 2013 College LGBT Sexual Health (Compared to heterosexual counterparts) STI LESBIAN BISEXUAL ♀ GAY BISEXUAL ♂ Chlamydia = = = = Gonorrhea = = ↑ = Genital HSV = ↑ = = Genital warts = = ↑ = Hep B or C = = = = HIV = = ↑ = Oswalt. 2013 Case 1. WZ (cont.) • Multiple male sexual partners • Anal and Oral sex – Versatile • Condoms sometimes • Doesn’t ask partners if they know their HIV status HIV and LGBT Youth • 1:4 new HIV infections 13-24yo • Young MSM 1:5 new HIV infections • Black youth 57% HIV infections in youth • 20-24yo group highest # of HIV diagnosis • 2 per 1000 college students are HIV+1 1ACHA-NCHA-II Anal Sex and HIV risk HIV Prevention • Condom use – Insertive anal sex: 63% effective – Receptive anal sex: 72% effective • Serosorting: 54% effective • TASP: 96% effective (maybe higher) • PrEP: 92% effective (maybe higher) • nPEP: ? effectiveness • Screening and treating other STIs Mental Health Disparities • Eating-related pathology (TG>G/B>F) – Diagnosis of ED – Diet pill use – Vomiting or laxative use • Depression and Suicidality – Felt sad: Bisexual > GL – Attempted suicide: 3xGL, 5xBisexual – Sought MH: Non-het 2x Diemer, 2015 NYC YRBS, 2013 Victimization Straight Missed school b/c felt unsafe G/L Bullied on school property Bisexual Unsure Experienced physical dating violence NYC YRBS, 2013 Experienced sexual dating violence Case 2. DD • 18yo Hispanic female • Requesting EC Taking a sexual history • Don’t assume: Patients are heterosexual Bisexuality is a phase Sexual orientation based on gender of partner Sexual orientation or gender identity based on appearance • Sexual orientation or gender identity is the same as last visit • LGBTQ patients are engaging in risky behavior • LGBTQ patients have unsupportive families • • • • Case 2. DD (cont.) • Had a few drinks at a party last night • Had consensual sex with a friend who identifies as bisexual. • Didn’t use barrier protection, not on BC. • DD says she came out as bisexual but thinks she identifies more as a lesbian Creating safe spaces • Provider sensitivity: • For LGBTQ youth, the strongest predictor of disclosing orientation/ identity was discussing sexual health with their provider • Recommendation to promote disclosure: “Just ask me” • Lesbians who were out to their providers were more likely to receive a pap test and other preventative care • Lesbian and bisexual youth are at least 2 times more likely than heterosexual youth to have unplanned pregnancies • You may be one of the few people with whom they feel comfortable discussing these issues Creating safe spaces • First impressions are important: patients will walk in and assess for affirmation • Assess and change current clinical environment - Clinic brochures and posters, health education materials - Unisex bathrooms • Ensure your intake forms are inclusive of multiple gender identities and sexualities - Establishes non-judgmental attitude • Advertise the cultural competency of your practice - Create and post non-discrimination, diversity policies, and confidentiality policy around clinic Creating safe spaces Creating safe spaces Taking a sexual history • Some questions to ask everyone: • Have you ever been or are you in a relationship? • How old is your partner(s)? How would you describe the relationship? • Have you had sex or been intimate with guys, girls, or both? • If you have not had sex yet, what are your plans about sex in the future? • Has anyone every touched you in a way that made you feel uncomfortable? • Do you talk with your parents or other adults about sex and sexual issues? Taking a sexual history • Do you (or your partner) use anything to prevent getting an STI? – How often- always, most of the time, sometimes, or never? – By site • Have you ever been told that you had an STI? • Have you ever traded sex for money, drugs, a place to stay, or other things you need? If at risk for pregnancy: • Do you (or your partner) use anything to prevent getting pregnant? • Have you ever been pregnant? What happened with that pregnancy? Asking about Gender and Sexual Behavior Some patients are going to be offended that you don’t assume heterosexuality or that they are cisgender; similarly, other patients will be relieved that you don’t. • “Do you consider yourself male, female, transgender or another gender?” OR • “What gender do you consider yourself?” • “What is your preferred gender pronoun (PGP)?” Asking about Gender and Sexual Behavior If the patient is sexually active include the following questions: – Have you gone down on anyone (had oral sex) – Have you had anal sex? – Do you share sex toys? • For MSM and MTF with M: “Do you top, bottom or both?” • For opposite-sex partnering: “Do you have penilevaginal sex?” • For WSW and FTM with F: “Do you share sex toys?” May need to use different wording for transgender patient: “What wording do you use to describe your genitalia? I am asking so I can use the correct term when asking questions.” Sexual behaviors “by site” Case 2. DD (cont.) • Declines birth control because she “doesn’t have sex with men very often.” • Declines STI testing since this was the first time she had condom-less intercourse with a guy. Case 3. SM • 19yo, identifies as transmale • Comes in for a physical • Interested in starting masculinizing hormone therapy Trans* • Person whose gender identity or expression differs from their sex assigned at birth • Umbrella term – MTF: Male-to-Female, Transwoman – FTM: Female-to-Male, Transmale – Gender variant, gender non-conforming, gender queer, non-binary, etc. Transgender is not… • A verb – You don’t transgender into… – There is no transgendering... • A noun – The transgender came... – Transgenders tend to... Transitioning • Process and time during which a person begins to live as their new gender • “Transitioning” means different things to different people • 4 main aspects: – – – – Social Legal Medical Surgical People may not be interested in all aspects of transition and there is no right order on how to transition TG Health care needs Knowledge is important but sensitivity even more so. It’s ok to not know, it’s not ok to not ask. • Discomfort with exam especially of genitalia and breasts – “How do you refer to those body parts?” – Explain reason for exam and give patient option to refuse Trans* patients • Assure the patient that many are uncomfortable with the exam and that they may stop the exam at any time • Provide information of why the exam is necessary • Ask about PGP and terms for anatomy • Discuss steps of exam before and during • Maintain best practices for both anatomy and hormonal milieu What more can we do? • Multi-site STI testing Urine-only would have missed: Kent, 2005 63.6% 69.6% What more can we do? • Trans* care: – Help patients access hormone therapy – Administer hormone injections – Teach patients to self-inject safely – Harm reduction approaches (???) What more can we do? • HIV+ patients: – Communicate with pt’s PMD (w/consent) – Help patients obtain medications • Rx by mail • Help with refills • Keep meds for patients if confidentiality issues – Help patients attend f/u visits What more can we do? • nPEP: – Discuss with all patients, especially those at higher risk – Provide starter packs or identify nearby health centers that do – Have resources for patients that need further care (beyond starter packs) What more can we do? CONTINUE TO BE ADVOCATES ON BEHALF OF OUR PATIENTS Care of LGBTQ Population in College Health THANK YOU!