* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download American Heart Association Target Drug Therapy Guidelines for
Neuropsychopharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Theralizumab wikipedia , lookup
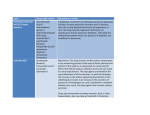
Adherence (medicine) wikipedia , lookup
American Heart Association Target Drug Therapy Guidelines for Heart Failure Heart Failure (HF) : Heart failure is a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. The following guidelines are from the American Heart Association’s 2009 Updated Guidelines. The Staging, Level of Evidence criteria and the complete set of guidelines can be found at http://circ.ahajournals.org/cgi/reprint/119/14/e391. Drug Therapy for Patients with Current or Prior Symptoms of HF and Low LVEF (Stage C): Class I: (Level of Evidence) a. It is recommended that diuretics and salt restriction should be used in patients with fluid retention. (C) b. One of the three recommended beta-blocker therapies should be used unless contraindicated. The recommended beta-blockers are: bisoprolol, carvedilol, or sustained release metoprolol succinate. (A) c. Angiotensin II receptor blockers are recommended for patients that are ACEI intolerant. (A) d. NSAIDS, most antiarrhythmic drugs and most calcium channel blockers should be avoided in these patients due to their potential to adversely affect the clinical status of the patient. (Vasoselective calcium channel blockers are an exception and may be used.) (B) e. Addition of an aldosterone antagonist is recommended in these patients with moderately to severe symptoms of HF who can be carefully monitored for preserved renal function and normal potassium concentration. Risks may outweigh benefits but patient should be consistently monitored. (Exact numbers in guidelines pg 22) (B) f. The combination of hydralazine and nitrates is recommended to improve the outcomes for African- American patients with moderate-severe symptoms on optimal therapy with ACEIs, beta-blockers, and diuretics. (B) Class IIa: a. It is reasonable to treat patients with atrial fibrillation and HF with a strategy to maintain sinus rhythm or with a strategy to control ventricular rate alone. (A) b. Angiotensin II receptor blockers are a reasonable alternative to an ACEI as first-line therapy in patients with mild-moderate HF, especially if patient is currently taking and ARB for another indication. (A) c. Digitalis can be beneficial in these patients to decrease hospitalizations for HF. (B) d. The addition of a combination of hydralazine and a nitrate is reasonable for these patients who are already taking an ACEI and beta-blocker for HF symptoms and have persistent symptoms. (B) Class IIb: a. The combination of hydralazine and a nitrate might be reasonable in patients who cannot be given an ACEI or ARB due to drug intolerance, hypotension, or renal insufficiency. (C) b. The addition of an ARB may be considered in persistently symptomatic patients with reduced LVEF who are already being treated with conventional therapy. (B) Class III: a. Routine combination of an ACEI, ARB, and aldosterone antagonist is not recommended for these patients. (C) b. Calcium channel blockers are not indicated as routine treatment for these patients. (A) c. Hormonal therapies other than to replace deficiencies are not recommended and may be harmful to these patients. (C) Table 1.Oral Diuretics Recommended for Use in the Treatment of Chronic Heart Failure Maximum Total Daily Duration of Drug Initial Daily Dose(s) Dose Action Loop Diuretics Bumetanide 0.5 to 1.0 mg once or twice 10 mg 4 to 6 hours Furosemide 20 to 40 mg once or twice 600 mg 6 to 8 hours Torsemide 10 to 20 mg once 200 mg 12 to 16 hours Thiazide Diuretics Chlorothiazide Chlorthalidone Hydrochlorothiazide Indapamide Metolazone 250 to 500 mg once or twice 12.5 to 25 mg once 25 mg once or twice 2.5 mg once 2.5 mg once 1000 mg 100 mg 200 mg 5 mg 20 mg 6 to 12 hours 24 to 72 hours 6 to 12 hours 36 hours 12 to 24 hours 5 mg once 12.5 to 25 mg once 50 to 75 mg twice 20 mg 50 mg† 200 mg 24 hours 2 to 3 days 7 to 9 hours Potassium-Sparing Diuretics* Amiloride Spironolactone Triamterene Sequential Nephron Blockade Metolazone Hydrochlorothiazide Chlorothiazide (IV) 2.5 to 10 mg once plus loop diuretic 25 to 100 mg once or twice plus loop diuretic 500 to 1000 mg once plus loop diuretic IV indicates intravenous; and mg, milligrams. *Eplerenone, although also a diuretic, is primarily used in chronic heart failure as a suppressor of the rennin-angiotensin-aldosterone system † Higher doses may occasionally be used with close monitoring. Table 6. Inhibitors of the Renin-Angiotensin-Aldosterone System and Beta Blockers Commonly Used for the Treatment of Patients With HF With Low Ejection Fraction Drug ACE Inhibitors Captopril Enalapril Fosinopril Lisinopril Perindopril Quinapril Ramipril Trandolapril Initial Daily Dose(s) Maximum Doses(s) 6.25 mg 3times 2.5 mg twice 5 to 10 mg once 2.5 to 5 mg once 2 mg once 5 mg twice 1.25 to 2.5 mg once 1 mg once 50 mg 3 times 10 to 20 mg twice 40 mg once 20 to 40 mg once 8 to 16 mg once 20 mg twice 10 mg once 4 mg once Angiotensin Receptor Blockers Candesartan Losartan Valsartan 4 to 8 mg once 25 to 50 mg once 20 to 40 mg twice 32 mg once 50 to 100 mg once 160 mg twice Aldosterone Antagonists Spironolactone Eplerenone 12.5 to 25 mg once 25 mg once 25 mg once or twice 50 mg once Table 2. Inhibitors of the Renin-Angiotensin-Aldosterone System and Beta Blockers Commonly Used for the Treatment of Patients with HF with Low Ejection Fraction. Table 1.Oral Diuretics Recommended for Use in the Treatment of Chronic Heart Failure Maximum Total Daily Duration of Drug Initial Daily Dose(s) Dose Action Loop Diuretics Bumetanide 0.5 to 1.0 mg once or twice 10 mg 4 to 6 hours Furosemide 20 to 40 mg once or twice 600 mg 6 to 8 hours Torsemide 10 to 20 mg once 200 mg 12 to 16 hours Thiazide Diuretics Chlorothiazide Chlorthalidone Hydrochlorothiazide Indapamide Metolazone 250 to 500 mg once or twice 12.5 to 25 mg once 25 mg once or twice 2.5 mg once 2.5 mg once 1000 mg 100 mg 200 mg 5 mg 20 mg 6 to 12 hours 24 to 72 hours 6 to 12 hours 36 hours 12 to 24 hours 5 mg once 12.5 to 25 mg once 50 to 75 mg twice 20 mg 50 mg† 200 mg 24 hours 2 to 3 days 7 to 9 hours Potassium-Sparing Diuretics* Amiloride Spironolactone Triamterene Sequential Nephron Blockade Metolazone Hydrochlorothiazide Chlorothiazide (IV) 2.5 to 10 mg once plus loop diuretic 25 to 100 mg once or twice plus loop diuretic 500 to 1000 mg once plus loop diuretic IV indicates intravenous; and mg, milligrams. *Eplerenone, although also a diuretic, is primarily used in chronic heart failure as a suppressor of the rennin-angiotensin-aldosterone system † Higher doses may occasionally be used with close monitoring. Table 6. Inhibitors of the Renin-Angiotensin-Aldosterone System and Beta Blockers Commonly Used for the Treatment of Patients With HF With Low Ejection Fraction Drug Initial Daily Dose(s) Maximum Doses(s) ACE Inhibitors Captopril 6.25 mg 3times 50 mg 3 times Enalapril 2.5 mg twice 10 to 20 mg twice Fosinopril Reference: 5 to 10 mg once 40 mg once Incorporated Into the ACC/AHA 2005 Guidelines for mg once Lisinopril American Heart Association. 2009 Focused 2.5Update to 5 mg once 20 to 40 in Adults. Perindoprilthe Diagnosis and Management of Heart Failure 2 mg once Circulation 2009;119e391-e479. Retrieved 8 to 16 mg once Quinapril from http://circ.ahajournals.org/cgi/reprint/119/14/e391 5 mg twice 20 mg twice Ramipril 1.25 to 2.5 mg once 10 mg once Trandolapril 1 mg once 4 mg once Angiotensin Receptor Blockers Candesartan 4 to 8 mg once 32 mg once