* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Forensic Psych Hospital and Clinic BC mental HealthAddictions
Survey
Document related concepts
Transcript
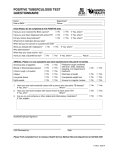
Western Node Collaborative Forensic Psychiatric Hospital and Clinics Medication Reconciliation October 2, 2006 Zaheen Rhemtulla B.Sc. (pharm) Forensic Psychiatric Hospital Forensic Clinics Forensic Psychiatric Hospital Secure, 190-bed Forensic Psychiatric Hospital Serves individuals referred by the Courts for treatment and assessment Provides treatment and support for those individuals who are deemed to require a secure inpatient facility due to their risk of harm to self and/or others Facility consists of nine clinical units (five secure, three closed and one open unit) Designated mental health facility under the Mental Health Act, which provides for involuntary admissions for treatment purposes Forensic Psychiatric Clinics 6 outpatient clinics with approximately 2000 registered clients Clinics responsible for the supervision and monitoring of persons found Not Criminally Responsible on Account of Mental Disorder (NCR-MDs) who are living in the community, and any persons who are found Unfit to Stand Trial, but have been granted a conditional discharge by the British Columbia Review Board Involves monitoring the client's progress in treatment and ensuring that the client is adhering to the conditions set out in the Disposition Order provided by the BC Review Board Clinics also conduct assessments that are ordered by the provincial courts of British Columbia (fitness to stand trial, NCR-MD, pre-sentence, and mental status) Provide assessment and treatment services for offenders on bail and probation/parole Background Information Forensic Psychiatric Hospital along with Riverview Hospital first convened a MedRec team June 2005 in response to the Safer Healthcare Now Campaign and accreditation requirements Recognizing the differing needs of Forensic Psychiatric Services, a separate Medication Reconciliation team consisting of a physician, nurses, pharmacists, and a Forensic Clinics Coordinator was formed February 2006 The goal for incorporating a medication reconciliation process for all transition points of patient care throughout the Forensic Hospital stay is December 2006 Project Charter Based on studies documenting the high percentage of adverse events occurring in hospitals due to medication errors, particularly at points of transition, Forensic Psychiatric Hospital and the Forensic Clinics are focused on providing the best possible care to the clients they serve by developing and implementing procedures and systems that result in better documentation and eliminate unintentional medication discrepancies at interfaces of care. Aims Reduce the mean number of undocumented intentional discrepancies at admission by 75% from new baseline (to be collected October 2006 once Pharmanet/MARs established) on the 2 admitting pilot wards (ASH1 and Dogwood East) by December 2006 Reduce the mean number of undocumented unintentional discrepancies at admission by 75% from new baseline (to be collected October 2006) on the 2 pilot wards by December 2006 Increase the medication reconciliation rate (success index) to 100% by December 2006 on the 2 pilot wards Improve medication information on admission by providing better access to Pharmanet and transferring agency information by Oct 2006. Forensic Psychiatric Hospital Medication Reconciliation Team Project Leader: Zaheen Rhemtulla [email protected] Administrative Leadership: Marilynn Macdougall [email protected] Risk Management: Peter Owen [email protected] Clinical Support: Jane Dumontet [email protected] Dr. Nader Sharifi [email protected] Dave Wharton [email protected] Jonie Pascual [email protected] Jennifer Dutton [email protected] Forensic Clinics Area Coordinator Ellen Haworth [email protected] Where are we in the process? Admission: BPMH reconciliation audits on all admissions to two admitting wards. Applying for all admitting physicians in the Hospital and Clinics to have Pharmanet access Working with the health care provider for BC Corrections (99% of hospital admissions are from Corrections) to consistently provide a same day MAR Discharge: Trialing a pharmacy computer generated discharge profile indicating all regularly scheduled medications the patient is to be taking upon discharge. The form is to be verified against current orders and signed by the physician(s) upon discharge. PRN medications are to be written in by the physician only if the patient requires them upon discharge. Included on the discharge profile is the last given and next due date of any long-acting injections. A copy of the current MAR is to be included in the discharge package 1.0 Mean Number of Undocumented Intentional Discrepancies 0.14 0.12 small sample size=8 patients 0.13 represents one undocumented Intentional discrepancy 0.10 Mean 0.08 0.06 Baseline data 0.04 0.02 Baseline data sample size very small=4 patients Month Actual Goal 20 06 D ec 20 06 N ov O ct 20 0 6 20 06 Se p 20 06 Au g 00 6 Ju n Ju l2 6 20 0 06 M ay 20 20 06 Ap r 06 ar M Fe b 20 20 06 6 Ja n 20 0 20 05 D ec N ov 20 05 0.00 2.0 Mean Number of Unintentional Discrepancies 0.14 small sample size=8 patients 0.13 represents one unintentional discrepancy 0.12 0.10 Mean 0.08 0.06 Baseline data 0.04 0.02 Baseline data sample size very small=4 patients Month Actual Goal 20 06 D ec 20 06 N ov O ct 20 0 6 20 06 Se p 20 06 Au g 00 6 Ju n Ju l2 6 20 0 06 M ay 20 20 06 Ap r 06 ar M Fe b 20 20 06 6 Ja n 20 0 20 05 D ec N ov 20 05 0.00 3.0 Medication Reconciliation Success Index 120% 100% 60% Baseline data 40% 20% Baseline data sample size very small=4 patients Month Actual Goal 20 06 D ec 20 06 N ov O ct 20 0 6 20 06 Se p 20 06 Au g 00 6 Ju n Ju l2 6 20 0 06 M ay 20 20 06 Ap r 06 ar M Fe b 20 20 06 6 Ja n 20 0 20 05 D ec 20 05 0% N ov Percentage 80% Keys to Success and Lessons Learned Successes: – – – Leadership buy-in and support, team commitment, funding Improvement in Pharmanet access for admission history Improvement in communication and provision of information from correctional agencies Barriers: - Data collection – difficulty accessing previous medication history when doing BPMH auditing - Small sample size Lessons Learned: - Need to improve access to medication history in order to proceed Next Steps Admissions: Continue and expand BPMH audits to all admissions to determine timely access to medication history through Pharmanet and current MARs Identify high risk patients (i.e. Over 40 y.o., more than 3 medications, high risk condition, high risk medication) who need a more comprehensive medication history Current data shows that only 25% of admissions are coming in on medications Next Steps Transfers Do an internal audit of transfer medication reconciliation. May not need additional reconciliation as present procedures involve the patient’s chart with the current MAR and medication cassette are sent with the patient to the receiving ward. In addition, the patient is followed by the same physician throughout their stay in the hospital. Discharges Utilize a “Discharge profile” to document regularly scheduled medications and prn’s required for discharge. Physicians will be able to use the form as a discharge order for pharmacy when discharge medications are required. Follow-up the process to identify effectiveness. Process will involve sending a copy of the current MAR to the receiving facility Contact Information Zaheen Rhemtulla Medication Reconciliation Project Team Leader/Clinical Pharmacist BC Mental Health and Addictions Services 2601 Lougheed Highway Coquitlam, BC V3C 4J2 604-524-7892 [email protected]