* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Palpitations - Back to Medical School
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Jatene procedure wikipedia , lookup
Electrocardiography wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
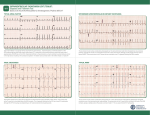
DIAGNOSING & TREATING PALPITATIONS Lee Graham Consultant Electrophysiologist Yorkshire Heart Centre PALPITATIONS • Definition: ‘an uncomfortable sensation in which a person is aware of their heart beat which may be irregular, pounding, forceful or rapid’ DIAGNOSTIC PATHWAY • History • Examination • Resting ECG • Symptom-ECG correlation • Additional investigations • Treatment HISTORY • Onset / offset characteristics • Age of onset • Perceived rate • Description of regularity • Duration and frequency • Associated symptoms (e.g. polyuria) • Neck pulsations • Triggers / relieving factors • Nocturnal symptoms HISTORY • Red Flag features (referral suggested) • Exercise induced • Associated syncope • Unexplained “seizure” • Chest pain • Family history of premature sudden cardiac death • Underlying structural heart disease HISTORY • Drug history including OTC medicines • Decongestants • Alcohol • Antidepressants • Psychotropics • Antibiotics & antifungals • Antihistamines • Methadone • Recreational drugs EXAMINATION • Cardiovascular • Pulse • Blood Pressure • Heart murmurs • Signs of heart failure • Features of thyroid disease RESTING ECG • Features to check • Sinus rhythm / arrhythmia • PR interval (WPW) • QRS duration / bundle branch block • ST segment shape (LVH / LV aneurysm / brugada) • QT interval (long or short) • Presence of Q waves (previous infarct) • T wave inversion (cardiomyopathy or IHD) Consider referral for any abnormal ECG PR interval Normal 3 to 5 small squares (120 - 200ms) QRS duration Normal up to 3 small squares (120ms) QT interval Depends on heart rate QTc 440 ms men QTc 460 ms women WOLFF-PARKINSON-WHITE SYNDROME BRUGADA SYNDROME HYPERTROPHIC CARDIOMYOPATHY DIAGNOSTIC YIELD FROM CLINICAL ASSESSMENT Not sufficiently accurate to exclude clinically significant arrhythmia Thavendiranathan et al. JAMA 2009;302:2135-43 SYMPTOM-ECG CORRELATION • 12-lead ECG taken with symptoms • Holter monitoring (24h - 7 day) • Event recorder with / without looping memory (patient activated device) • Implantable loop recorder (ILR) HOLTER MONITOR • Requires typical symptoms during recording • Useful if symptoms occur several times per week • Asymptomatic arrhythmias • Useful for patients who are unable to trigger a monitoring device e.g. syncope EVENT RECORDER • Useful for less frequent symptoms • Longer duration of symptoms • Symptoms need to be reasonably well tolerated IMPLANTABLE LOOP RECORDERS AMBULATORY MONITORING OPTIONS 24h- 7 days 7-30 days 36 months Time (months) CASE VIGNETTE • 68y old man • 10 month history of palpitations • Onset with exertion • Syncopal on two occasions • Normal cardiovascular exam • Normal resting ECG ILR implanted ILR SYMPTOM – RHYTHM CORRELATION DIAGNOSTIC YIELD FROM MONITORING Investigation ECG during symptoms Holter Event recorder ILR Any arrhythmia Clinically significant arrhythmia 3-26% 2% 34% 3-24% 30-60% 17-19% - 73% Thavendiranathan et al. JAMA 2009;302:2135-43 ADDITIONAL INVESTIGATIONS • Structural cardiac disease • Echocardiogram • Cardiac MRI • Exercise tolerance test • Cardiac catheterisation • Electrophysiological study +/- catheter ablation PALPITATIONS-COMMON CAUSES • Sinus Tachycardia • Ectopics (PAC’s / PVC’s) • Supraventricular tachycardia (AVNRT / AVRT / atrial tachycardia) • Atrial flutter • Atrial fibrillation • Ventricular tachycardia SINUS TACHYCARDIA • Onset and termination are gradual (i.e. not paroxysmal) • Perceived rate relatively slow • May persist for several hours or days • Normal P wave morphology • Physiological • sensitive to autonomic modulation • Inappropriate • Usually resting rate >100bpm ;mean >95bpm on 24h Holter INAPPROPRIATE SINUS TACHYCARDIA • Poorly understood • Young women most commonly affected • Associated symptoms of dyspnoea, pre-syncope & fatigue • Association with Postural Orthostatic Tachycardia Syndrome • Treatment unsatisfactory • Beta-blockers or rate limiting Ca antagonist • Ivabradine • Catheter modification of the sinus node can be attempted ECTOPICS • Usually sudden onset • Perceived as ‘missed beats’ often followed by thud & fluttering • rate relatively slow • More commonly noticeable at rest or in bed • Often described as persistent for several hours or days • Sporadic • Reassurance • Treatment usually not required although beta-blockers can be helpful RV OUTFLOW TRACT ECTOPY / VT RV OUTFLOW TRACT ECTOPY / VT • Frequent ectopics / salvos • Catecholamine sensitive • Treat with beta-blockers • Catheter ablation offers 80% chance of cure if remains symptomatic • 1% risk tamponade SUPRAVENTRICULAR TACHYCARDIA • Usually sudden onset / offset (except atrial tachycardia) • Perceived rate rapid and regular • Pounding pulsation in neck (AVNRT) • Variable duration • Vagal manoeuvres may terminate • Usually adenosine sensitive • Reentry most common mechanism (except atrial tachycardia) • AVRT/AVNRT/atrial tachy WOLFF-PARKINSON-WHITE SYNDROME • Short PR interval No conduction delay • Delta wave • Ventricular preexcitation • AVRT most common arrhythmia • AF more common and may be preexcited • Small risk of sudden death AV node Accessory pathway WOLFF-PARKINSON-WHITE SYNDROME ATRIOVENTRICULAR REENTRANT TACHYCARDIA Conduction down AV node • Usually narrow complex • Rarely broad complex • Often frequent episodes starting in childhood Up accessory pathway AV REENTRANT TACHYCARDIA PREEXCITED AF • AF may conduct rapidly over accessory pathway • Irregular broad complex tachycardia • Risk of degeneration to VF • Avoid AV node blockers PREEXCITED AF MANAGEMENT OF WPW • Refer to an electrophysiologist • EPS and catheter ablation if symptomatic • 95% curative (<1% risk) • Reasonable to offer asymptomatic patients EPS • Flecainide antiarrhythmic drug of choice AV NODAL REENTRANT TACHYCARDIA • ~ 60% of all SVT F > M Slow pathway • Onset often later than in AVRT • Beta-blockers or verapamil first line antiarrhythmics • Catheter ablation 95% curative but 1% risk AV node damage Fast pathway AV NODAL REENTRANT TACHYCARDIA ATRIAL FLUTTER • Regular or irregular palpitations • Paroxysmal or persistent • Saw tooth baseline • Atrial rate usually 300 min • Ventricular rate variable 2:1 block common • Often difficult to rate (or rhythm) control • Catheter ablation 90-95% curative and should be offered as first line (<1% risk) “TYPICAL” ATRIAL FLUTTER CATHETER ABLATION FOR TYPICAL FLUTTER ATRIAL FIBRILLATION • Assess symptoms • Control ventricular rate • Assess thromboembolic risk • Rate vs. rhythm control strategy WHO SHOULD BE OFFERED RHYTHM CONTROL • Symptomatic AF despite adequate rate control • Young symptomatic patients • AF related heart failure • AF secondary to corrected trigger or cause EHRA. EHJ 2010;31:2369-2429 RHYTHM CONTROL FOR AF • Antiarrhythmic drug therapy • Beta-blockers • Flecaininde • Sotalol, amiodarone, dronedarone • Cardioversion • Catheter ablation PULMONARY VEIN TRIGGERS DRIVE PAROXYSMAL AF RATIONALE FOR AF ABLATION • Electrical isolation of the pulmonary veins • Prevents “triggers” and “drivers” of AF • Creates electrically inexcitable “scar” around the PV’s which blocks PV ectopics from entering the left atrium • More effective in paroxysmal than in persistent AF THE IDEAL PATIENT FOR AF ABLATION ? • Arrhythmia related symptoms • Refractory or intolerant to at least one class 1 or 3 drug • ? Young age • Paroxysmal rather than persistent AF • Short duration of symptoms • Structurally normal heart • Informed and motivated CATHETER ABLATION FOR AF • ~ 70% success rates • Often multiple procedures required • 3-4 hour procedure • 3-4% risk major complication • Stroke 0.5-1% • Cardiac tamponade 1-2% • Usually second line ANY QUESTIONS?