* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Diagnosis and Management of TB - Croydon Health Services NHS
Gastroenteritis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Common cold wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
Germ theory of disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Tuberculosis wikipedia , lookup
Behçet's disease wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Kawasaki disease wikipedia , lookup
Globalization and disease wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
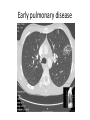
Diagnosis and Management of TB John Yates Consultant Infectious Diseases Diagnosis • Generally sub-acute illness • Any persistent symptom may indicate active tuberculosis • May be relatively mild • Any systemic symptoms – fever, weight loss, night sweats, malaise, anorexia – increase suspicion • Exposure history usually irrelevant if high risk ethnic background Sites of infection • • • • • • • • • • About 50/50 pulmonary/non-pulmonary 24% extra-pulmonary LNs 10% intra-throracic LNs 10% pleural 6% bone/joint ( 3% spine) 5% GI 3% CNS 2% miliary 1% GU Others – skin, eye, breast, Diagnosis- pulmonary • • • • • Persistent cough +/- haemoptysis Fever, weight loss, night sweats Symptoms may be very mild Usually stethoscope not useful Breathlessness uncommon unless severe, disseminated disease • May be asymptomatic • Main initial investigation – CXR • Referral to TB clinic Diagnosis - pulmonary • • • • • • • CXR Sputum, if productive, x3 for smear and culture Basic blood tests HIV test Mantoux/IGRA CT to guide bronchoscopy/biopsy if unproductive Broncho-alveolar lavage/induced sputum for smear and culture • PCR for smear positive cases/difficult diagnoses Early pulmonary disease Patch of nodules Early pulmonary disease Late pulmonary disease cavity Lymphadenopathy Asymmetrical hilar enlargement Extra-pulmonary • Cervical lymph nodes – mantoux +/- IGRA, biopsy for histology/culture • Other sites imaging/biopsy • Multifarious presentations • Main aid to diagnosis is suspicion • Don’t be put off by normal plain films of chest/abdo/spine/bone Extra-pulmonary • • • • Persistent symptoms > 2 weeks +/- night sweats/weight loss/malaise High risk ethnic backgrounds Elevated ESR/CRP, normocytic anaemia, low albumin • Back pain, abdo pain, headache etc • Please refer to TB clinic Diagnosis –extra pulmonary • Immunological tests – negative in 10% active disease for mantoux • Targeted imaging – but disease often multifocal e.g. peritoneum, lymph nodes, spine, chest simultaneously • Biopsy for histology, smear and culture Abdominal TB Ascites Lymph node mass Spinal TB Increased soft tissue around L4/5 Management • Risk assessment for Multi-Drug Resistant -MDR TB – 1.5% cases resistant to rifampicin and isoniazid • Smear positive cases sent for PCR for drug resistance • Isolation of smear positive cases for 2 weeks– usually at home but in hospital if ill or unable due to shared accommodation/homelessness • Initiate treatment – quadruple therapy – rifampicin/isoniazid/pyrazinamide, ethambutol or moxifloxacin • Monitored treatment – TB nurses, clinic • Review with culture results • MDR cases referred to St George’s