* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Abnormal bowel movement
Survey
Document related concepts
Transcript
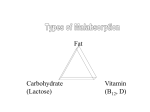
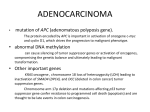
Presented by: Abdullah Al-Ruwaita Abdullah Al-Manea Yousif Al-Ansari Supervised by: Prof. Riaz Qureshi, FRCGP Bowel movement Normal Abnormal Constipation Diarrhea acute Chronic Dif: hard, dry, lumpy stools that are difficult Causes: or painful to pass - Congenital or Primary. - Secondary which includes: -Insufficient dietary fiber intake. -Inadequate fluid intake. -Decreased physical activity. -Side effects of medications. -Hypothyroidism. -Obstruction by colorectal cancer. Dif: three or more loose or watery stools per day, without abdominal bloating, pressure, and cramps commonly referred to as gas. Causes: Infections: - Viral - Bacterial - Parasites • Intestinal disorders • Reaction to certain medications • Dif: as loose stools that last for at least four weeks, usually means three or more loose stools per day. Causes: - Irritable bowel syndrome Inflammatory bowel disease Malabsorption syndromes Chronic infections. Chronic diarrhea Irritable bowel syndrome Inflammatory Bowel Disease Celiac Disease Ulcerative colitis Crohn's disease Lactose intolerance Dif: is a gastrointestinal syndrome characterized by chronic abdominal pain and altered bowel habits in the absence of any organic cause. It is the most commonly diagnosed gastrointestinal condition. prevalence of IBS in North America estimated from population-based studies is approximately 10 to 15 percent in Europe found an overall prevalence of 11.5 percent 2:1 female:male Chronic abdominal pain (as a crampy sensation and abdominal pain) Altered bowel habits (ranging from diarrhea, constipation) - Diarrhea (frequent loose stools of small, fecal incontinence and feeling of incomplete evacuation) - Constipation (Stools are often hard, may last from days to months)Other gastrointestinal symptoms Other gastrointestinal symptoms (Upper GI symptoms) Rome III diagnostic criteria: Recurrent abdominal pain or discomfort. at least 3 days per month in the last 3 months associated with 2 or more of the following: (1) Improvement with defecation (2) Onset associated with a change in frequency of stool (3) Onset associated with a change in form (appearance) of stool many disorders present with similar symptoms (r/o), Routine laboratory studies (complete blood count, chemistries) are normal in IBS. "Alarm" or atypical symptoms which are not compatible with IBS include (red flags) : • Rectal bleeding Nocturnal or progressive abdominal pain Weight loss Laboratory abnormalities such as anemia, elevated inflammatory markers, or electrolyte disturbances • • • Patients with one of these alarm symptoms require further imaging studies and/or colonoscopy It is not clear why patients develop IBS. Sometimes it occurs after an infection of the intestines. This is called post-infectious IBS. There may also be other triggers; Brain-gut signal problems (thalamic activity). GI motor problems (unpleasant stimuli). Hypersensitivity (stimulation of various receptors in the gut wall). Mental health problems (Such as anxiety, depression). Bacterial gastroenteritis. Small intestinal bacterial overgrowth. Food sensitivity (food intolerance to certain foods). Child Abuse Crohn's disease Ulcerative colitis Diverticulosis Celiac Disease Lactose intolerance Colon malignancy Peptic ulcer disease Biliary liver disease Chronic pancreatitis Medications Lymphoma of the GI Patient education: Education of the proposed mechanisms of IBS helps to validate the patient's illness experience and sets the basis for therapeutic interventions Dietary - modification: dietary history may reveal patterns of symptoms related to specific foods. Lactose (similarity that may occur in symptoms of IBS and lactose intolerance, an empiric trial of a lactose free diet should be considered ) - - Exclusion of gas-producing foods Food allergies Gluten sensitivity Carbohydrate malabsorption Fiber (increase in the intake of fiber is often recommended) Physical activity Psychosocial therapies - Cognitive behavior therapy Relaxation training - Gut-directed Hypnotherapy - MEDICATIONS: - Antispasmodic agents o o Mebeverine Alverine Dicyclomine (an anticholinergic) - Antidepressants (TCAs, SSRIs) o Mind and body often combine to increase the distress of IBS patients. Psychological intervention worth considering. IBS patients can be managed well by family physicians. Don’t forget “red flags” for referral to GI specialist is a must ! Chronic diarrhea Irritable bowel syndrome Inflammatory Bowel Disease Celiac Disease Ulcerative colitis Crohn's disease Lactose intolerance Inflammatory bowel disease (IBD) is comprised of two major disorders: 1.Ulcerative colitis (UC). 2.Crohn's disease (CD). •IBD can present at any age: –The peak :15 - 30 years. – A second peak 50 •Etiology is unknown but there are 3 main factors contributing to it : Genetic factors, environmental factors, diet. Ulcerative colitis is characterized by recurring episodes of inflammation limited to the mucosal layer of the colon. •major symptoms of UC are: -Diarrhea -rectal bleeding ( usually fresh blood ) -Tenesmus -passage of mucus -crampy abdominal pain No single modality is enough for Diagnosis . Combination of clinical picture, laboratory, Endoscopy, pathology. Colonscopy findings: –The vascular markings are lost, petechiae, exudates, touch friability, and frank hemorrhage may be present. –In Pathology, biopsy shows : –Crypt abscesses. –chronic changes including branching of crypts, atrophy of glands, and loss of mucin in goblet cells –Rule out infection –5 ASA (5-amino salicylic acids)- therapy: •Rectal ( if the UC extend less than 20 cm ) •Oral ( if the UC extend more than 20 cm +) in combination with rectal –Corticosteroids: •Systemic: Prednisolone •Local acting: enema. –Immunomodulators : •Azithyoprine •Methotrexate –Anti TNF therapy Is a disorder of uncertain etiology that is characterized by transmural inflammation of the gastrointestinal tract. SYMPTOMS: –Fatigue. –Diarrhea. –Abdominal pain. –Weight loss. –Fever. –Bleeding is very rare. Colonoscopy: • Endoscopic features include focal ulcerations adjacent to areas of normal appearing mucosa along with polypoid mucosal changes that give a cobblestone Wireless capsule endoscopy Serologic markers •Inflamatory marker : ESR, CRP •Antibody tests : •Antineutrophil cytoplasmic antibodies (pANCA) > with UC •Anti-Saccharomyces cerevisiae antibodies (ASCA) > with CD Stool markers — fecal calprotectin. The intestinal complications of Crohn's disease include the following: -Intestinal obstruction -Fistulas -Abscess -Hemorrhage (bleeding) - Unusual in Crohn's disease -Malabsorption -Carcinoma, Colonic disease increases risk of colon cancer The longer you have Crohn's disease, the more likely you are to develop complications that can be fatal. The goals of treatment of Crohn's disease are to reduce the underlying inflammation, which then relieves symptoms, prevents complications, and maintains good nutrition. Aspirin-like anti-inflammatory drugs (mesalamine) reduce the inflammation. Corticosteroids reduce inflammation and suppress the immune system. Antibiotics reduce inflammation indirectly by reducing infection. Immunosuppressants suppress the immune system. Surgery. (alternative). Celiac disease is a medical condition in which the absorptive surface of the small intestine is damaged by a substance called gluten. This results in an inability of the body to absorb nutrients: protein, fat, carbohydrates, vitamins and minerals, which are necessary for good health. SYMPTOMS: –anemia. –chronic diarrhea. –weight loss. –Fatigue. –cramps and bloating. –irritability. Screening Biopsy: A definitive diagnosis can only be made by a small bowel biopsy. Celiac disease as yet has no known cure, but can usually be effectively treated and controlled. The treatment of celiac disease is strict adherence to a GLUTEN FREE DIET FOR LIFE. Lactose intolerance means the body cannot easily digest lactose, a type of natural sugar found in milk and dairy products. Lactose intolerance occurs when the small intestine does not make enough of an enzyme called lactase. Lactose intolerance most commonly runs in families, and symptoms usually develop during the teen or adult years. It could be temporary Symptoms of lactose intolerance can be mild to severe, depending on how much lactase the body makes. Symptoms usually begin 30 minutes to 2 hours after eating or drinking milk products. symptoms may include: •Bloating. •Pain or cramps. •Gurgling or rumbling sounds in your belly. •Gas. •Loose stools or diarrhea. •Throwing up. medical To history. confirm a diagnosis: -Hydrogen breath test -Lactose tolerance test Fortunately, lactose intolerance is relatively easy to treat. No known way exists to increase the amount of lactase enzyme the body can make, but symptoms can be controlled through diet. Who is ready ? Questions ?