* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chronic Kidney Disease
Survey
Document related concepts
Transcript
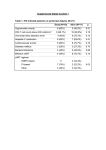
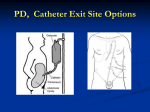
Dialysis • Begun when the patient’s uremia can no longer be adequately managed conservatively • Initiated when the GFR <5 – 10% 0f normal Dialysis • The movement of fluid and molecules across a semipermeable membrane from one compartment to another Dialysis • Two methods of dialysis available Peritoneal dialysis (PD) Hemodialysis (HD) General Principles of Dialysis • Diffusion • Osmosis • Ultrafiltration Osmosis and Diffusion Across Semipermeable Membrane Fig. 45-5 DIALYSATE • Is an electrolyte solution that is similar to that of normal plasma, except contains no potassium • Different concentrations Peritoneal Dialysis Dialysis Solutions and Cycles • Available commercially in 1- or 2-L plastic bags with glucose concentrations of 1.5%, 2.5%, and 4.25% Peritoneal Dialysis Catheter Placement • Peritoneal access is obtained by inserting a catheter (Tenckhoff) through the anterior wall • Technique for catheter placement varies • Usually done via surgery Tenckhoff Catheter Fig. 45-6 Peritoneal Dialysis Dialysis Solutions and Cycles • Three phases of the PD cycle Inflow (fill) Dwell (equilibration) Drain Peritoneal Dialysis Complications • • • • • • • • • • • • Exit site infection Peritonitis/Infection: cloudy dialysate Hypotension Abdominal pain (may be bowel perforation): brownish dialysate Bladder perforation: amber dialysate Outflow problems Hernias Lower back problems Bleeding Pulmonary complications Protein loss CHO and lipid abnormalities Peritoneal Dialysis Types • Automated peritoneal dialysis (APD) • Continuous ambulatory peritoneal dialysis (CAPD) Peritoneal Dialysis Advantages • • • • • Short training program Independence Ease of traveling Fewer dietary restrictions Greater mobility than with HD Hemodialysis Vascular Access Sites • Shunts • Internal arteriovenous fistulas and grafts • Temporary vascular access Vascular Access for Hemodialysis Fig. 45-11 Hemodialysis Dialyzers • Long plastic cartridge that contains thousands of parallel hollow tubes or fibers Hemodialysis System Fig. 45-14 Hemodialysis Complications • • • • • • Hypotension Muscle cramps Loss of blood Hepatitis Sepsis Disequilibrium syndrome Hemodialysis Effectiveness and Adaptation • Cannot fully replace the metabolic and hormonal functions of the kidneys • Can ease many of the symptoms • Can prevent certain complications Kidney Transplantation • Over 54,000 patients currently awaiting cadaveric kidney transplants • Over 5200 living donor transplants done in 2002 • Extremely successful • 1-year graft survival rate 90% for cadaver transplants 95% for live donor transplants Kidney Transplantation Advantages of kidney transplant compared with dialysis: Reverses many of the pathophysiologic changes associated with renal failure Eliminates the dependence on dialysis Less expensive than dialysis after the 1st year Kidney Transplantation Recipient Selection • Candidacy determined by a variety of medical and psychosocial factors that vary among transplant centers Contraindications to transplantation: Disseminated malignancies Cardiac disease Chronic respiratory failure Extensive vascular disease Chronic infection Unresolved psychological disorders Kidney Transplantation Histocompatability Studies • Purpose of testing is to identify the HLA antigens for both donors and potential recipients Kidney Transplantation Donor Sources • • • • Compatible blood type cadaver donors Blood relatives Emotionally related living donors Altruistic living donors Kidney Transplantation Surgical Procedure • Donor nephrectomy performed by a urologist or transplant surgeon • Begins an hour or two before the recipient’s surgery is started Kidney Transplantation Kidney Transplant Recipient Transplanted kidney Usually placed extraperitoneally in the iliac fossa Right iliac fossa is preferred Before incision: Urinary catheter placed into bladder Antibiotic solution instilled • Distends the bladder • Decreases risk of infection Kidney Transplantation Nursing Management Preoperative Care • • • • • Emotional and physical preparation Immunosuppressive drugs ECG Chest x-ray Laboratory studies Kidney Transplantation Nursing Management Postoperative Care Live donor Care is similar to laparoscopic nephrectomy Close monitoring of renal function Recipient Maintenance of fluid and electrolyte balance is 1st priority Kidney Transplantation Immunosuppressive Therapy Goals: Adequately suppress the immune response Maintain sufficient immunity to prevent overwhelming infection Medications: Cyclosporin Predisone Prografin FK 506 (Tacrolimus) Mycophenolate Mofetil (CellCept) Kidney Transplantation Complications Rejection Hyperacute (antibody-mediated, humoral) rejection • Occurs minutes to hours after transplantation Kidney Transplantation Complications Rejection Acute rejection • Occurs days to months after transplantation Acute Rejection Fig. 45-19 Kidney Transplantation Complications Rejection Chronic rejection • Process that occurs over months or years and is irreversible Kidney Transplantation Complications Infection Most common infections observed in the 1st month: • Pneumonia • Wound infections • IV line and drain infections Fungal infections Viral infections • CMV • Epstein-Barr virus • Herpes simplex virus Kidney Transplantation Complications Cardiovascular disease Transplant recipients have incidence of atherosclerotic vascular disease Malignancies Primary cause is immunosuppressive therapy Kidney Transplantation Complications Recurrence of original renal disease Glomerulonephritis IgA nephropathy Diabetes mellitus Focal segmental sclerosis Kidney Transplantation Complications Corticosteroid-related complications Aseptic necrosis of the hips, knees, and other joints Peptic ulcer disease Glucose intolerance and diabetes Hyperlipidemia Cataracts Increased incidence of infections and malignancies