* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Appendicular Skeletal Markings
Survey
Document related concepts
Transcript
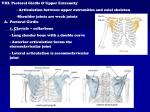
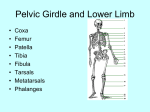
Appendicular Skeletal Markings AAIMT© Appendicular Skeletal Markings Document 0 Revised: October 11, 2006 Appendicular Skeletal Markings I. Pectoral girdle – also known as the shoulder girdle is made up of four bones: two clavicles and two scapulae. It supports the arms and serves as a place of attachment for muscles that move them. These bones are only loosely held together by ligaments and muscles. This is an incomplete ring – not attached at the posterior aspect. This arrangement allows for great flexibility, but it also means that the shoulder is the weakest joint in the body and very easily dislocated. A. Function 1. Attaches the bones of the upper extremities to the axial skeleton. 2. Gives a place of attachment for the muscles that move arms. 3. The clavicle serves as a brace for the scapula and helps stabilize the shoulder but it is structurally weak, and if force is applied to the shoulder, it will fracture. B. Structure 1. Clavicles (2) – also known as collarbones, these are slender S-shaped bones. Each articulates with the manubrium of the sternum medially. This joint is the only attachment of the pectoral girdle to the axial skeleton. Each also articulates with a scapula. (Figure 1) Figure 1 2. Scapulae (2) – also known as shoulder blades, these are broad, flat bones that resemble a triangle. The fact that these are not joined together is what gives the pectoral girdle its flexibility. The following are markings on the scapulae (Figure 2): AAIMT© Appendicular Skeletal Markings Document 1 Revised: October 11, 2006 a. Spine of the scapula – a boney ridge on the posterior/superior area of the scapula running diagonally across it. It serves as an attachment site for muscles. b. Acromion process – this articulates with a clavicle and provides a place of attachment for arm and chest muscles. This is the end of the spine that projects as a flattened, expanded process. c. Glenoid cavity –inferior to the acromion is a depression, this articulates with the head of the humerus. This cavity is smaller than the head of the humerus which allows for a large amount of flexibility. d. Medial border – this is the medial border of the scapula, the area more toward the spinous processes. It is the thin edge of the scapula and also known as the vertebral border. e. Lateral border – this is the lateral border of the scapula, the area more toward the sides of the body. It is also the thick edge of the scapula and also known as the axillary border. f. Inferior angle – this is the lower angle of the scapula, the point closer to the feet where the medial and lateral borders meet. g. Superior border/scapular notch – this joins the vertebral border at the superior angle. The scapular notch is a prominent indentation along the superior border near the coracoid process; it allows passage of the suprascapular nerve. h. Superior angle – This is where the superior border joins the vertebral border. i. Coracoid process – This is a projection of the anterior surface of the scapula at the lateral end of the superior border to which muscles attach. j. Supraspinous fossa – This is above the spine of the scapula on the dorsal surface and serves as an attachment site for one of the rotator cuff muscles. k. Infraspinous fossa – This is below the spine of the scapula on the dorsal surface and serves as an attachment site for several muscles. l. Subscapular fossa – This is on the ventral surface of the scapula and serves as an attachment site for one of the rotator cuff muscles. Figure 2 AAIMT© Appendicular Skeletal Markings Document 2 Revised: October 11, 2006 II. Upper Extremities – consists of 60 bones. Each upper extremity includes the bones of the upper arm (humerus), the forearm (radius and ulna), and wrist and hand (carpals, metacarpals, and phalanges). A. Function 1. Along with the muscles of the shoulder and arms these serve as levers to move the upper limbs. 2. Attachment sites for muscles. B. Structure 1. Humerus (2) – this is also called the arm bone. It is the longest bone in the upper extremity. It articulates proximally with the scapula and distally at the elbow with both the ulna and radius. Following is a list of prominent features (Figure 3): a. Head – this is at the proximal end of the humerus. The head fits into the glenoid cavity of the scapula. b. Anatomical Neck – this is an oblique groove just distal to the head. c. Greater Tubercle – this is a lateral projection distal to the neck and serves as an attachment site for muscles. d. Lesser Tubercle – this is an anterior projection and serves as an attachment site for muscles. e. Intertubercular groove – also known as the bicipital groove or the intertubercular sulcus, it is a groove that runs between the two tubercles. One of the biceps brachii tendons lays in this groove. f. Surgical Neck – This is a constricted portion just distal to the tubercles. It is named this because it is the site most often fractured. g. Body – also known as the shaft, this is the length of the bone. h. Deltoid Tuberosity – this is a roughened, V-shaped area along the middle portion of the shaft. This serves as an attachment site for the deltoid muscle. i. Capitulum – This is a rounded knob that articulates with the head of the radius. j. Trochlea – this is a pulley-like surface that articulates with the ulna k. Coronoid Fossa – this is an anterior depression that receives part of the ulna when the forearm is flexed. l. Olecranon Fossa – this is a posterior depression that receives the olecranon of the ulna when the forearm is extended. m. Medial Epicondyle – This is a rough projection on the medial, distal end and serves as an attachment site for muscles. n. Lateral Epicondyle – This is a rough projection on the lateral, distal end and serves as an attachment site for muscles. AAIMT© Appendicular Skeletal Markings Document 3 Revised: October 11, 2006 Figure 3 2. Ulna (2) – The ulna is the longer bone of the forearm on the medial side (little finger) and has the following features (Figure 4): a. Olecranon Process – this articulates with the olecranon fossa of the humerus when the elbow is extended. b. Coronoid Process – this articulates with the coronoid fossa of the humerus when the elbow is bent. c. Ulna Tuberosity – this serves as an attachment site for muscles d. Trochlea notch – this is a curved area between the olecranon and the coronoid process. The Trochlea of the humerus fits into this notch. e. Radial notch – this is a depression located laterally and inferiorly to the trochlear notch. The head of the radius fits into this notch. f. Head – this is the distal end of the ulna. g. Styloid process – this is on the posterior side of the distal end. AAIMT© Appendicular Skeletal Markings Document 4 Revised: October 11, 2006 3. Radius (2) – this is the lateral bone of the forearm (on the thumb side) and has the following features (Figure 4): a. Head – this is on the proximal end and is disc-shaped to articulate with the capitulum of the humerus and the radial notch of the ulna. b. Radial tuberosity – this is a raised, roughened area on the medial side where the biceps brachii tendon attaches. c. Neck – This is directly beneath the head of the radius. d. Styloid process – this is at the distal end on the lateral side. e. Ulnar notch – this is on the distal end and is a medial, concavity for articulation with the distal end of the ulna. Figure 4 4. Hand (27 bones) – Hands typically have a wrist, a palm, and five fingers with the following features (Figure 5): AAIMT© Appendicular Skeletal Markings Document 5 Revised: October 11, 2006 a. Carpal bones (8) – these are small bones tightly bound by ligaments in two transverse rows of four each. In the anatomical position, the proximal row, from lateral to medial, consists of the scaphoid, lunate, triquetrum, and pisiform. Usually, in cases involving carpal fractures, only the scaphoid is involved. The distal row, from lateral to medial, consists of the trapezium, trapezoid, capitate, and hamate. (A good acronym to remember the order of the carpals: Sally Left The Party To Take Cathy Home) b. Carpal tunnel – this is the space on the anterior (palmar) surface of the wrist between the carpal bones and a broad, thick piece of fascia (connective tissue) called the flexor retinaculum. The purpose of this “tunnel” is to hold various tendons, blood and nerve vessels as they pass from the forearm to the hand. c. Metacarpals (5) – these form the knuckles when a fist is made. This is what makes up the palm of the hand. Each metacarpal bone consists of a proximal base, a shaft, land a distal head. They are numbered one through five with the thumb being number one. The bases articulate with the distal row of carpal bones and with one another. The heads articulate with the proximal phalanges of the fingers. d. Phalanges (14) – these are the bones of the fingers. A single bone in any finger is called a phalanx (FA-lanks). Each phalanx consists of a proximal base, a shaft, and a distal head. There are only two phalanges in the first digit, or thumb (pollex), and three in each of the remaining four digits. The first row of phalanges, or the proximal row, articulate with the metacarpal bones and the second row of phalanges. The second row, or the middle row, articulate with the proximal row and the third row. The third, distal row articulate with the middle row. The thumb has no middle phalanx. AAIMT© Appendicular Skeletal Markings Document 6 Revised: October 11, 2006 Figure 5 AAIMT© Appendicular Skeletal Markings Document 7 Revised: October 11, 2006 III. Pelvic girdle or pelvis (2 coxal, or hip bones, sacrum, coccyx) - These strong bones are firmly attached to one another and bear the weight of the body. (Figures 6, 7 & 8) A. Function 1. Serves as a place of attachment for the legs 2. Protects the urinary bladder, the internal reproductive organs, and a portion of the large intestine B. Structure (3 portions that are fused at the acetabulum) 1. Ilium – this is the largest part of the coxal bone land flares outward to give the hip prominence. a. Iliac crest – this is the superior border b. Anterior superior iliac spine (ASIS) – the place where the iliac crest ends anteriorly. c. Anterior inferior iliac spine (AIIS) – this is just below and medial to the ASIS and serves as an attachment site for muscles. d. Posterior superior iliac spine (PSIS) – the place where the iliac crest ends posteriorly. e. Posterior inferior iliac spine (PIIS) – this is an area just below the PSIS and serves as an attachment site for muscles. f. Greater sciatic notch – this is the site where blood vessels and the sciatic nerve pass posteriorly into the lower leg. It is just inferior to the PSIS. g. Iliac fossa – this is the concavity of the ilium and is an attachment site for the iliacus muscle. h. Articular surface – This is the surface on the posterior side of the ilium where the sacrum articulates with the ilium at the sacroiliac joint. i. Sacroiliac joint – the articulation of the ilium and sacrum. 2. Pubis – this is the anterior and inferior part of the coxal bone. It consists of the following: a. Superior ramus – the superior angle of the pubis that serves as attachment sites for muscles. b. Inferior ramus – the inferior angle of the pubis that serves as attachment sites for adductor muscles. c. Body – the major portion of the pubis. d. Pubic Symphysis – this is the joint between the two coxal bones. It consists of fibrocartilage. e. Pubic crest – the most superior portion of the pubis that serves as an attachment site for adductor muscles. f. Pubic tubercle – this is just below the superior ramus and serves as attachment sites for muscles. g. Obturator foramen – this is posterior to the place where the pubis and the ischium join together – it is a large opening through which blood vessels and nerves pass anteriorly into the lower leg. AAIMT© Appendicular Skeletal Markings Document 8 Revised: October 11, 2006 3. Ischium –this is the most inferior part of the coxal bone and consists of the following: a. Ischial spine – this is near the junction of the ilium and ischium and projects into the pelvic cavity and serves as a site for muscle attachment. The distance between the two ischial spines gives the size of the pelvic cavity which is important for childbearing purposes. b. Lesser sciatic notch – this is an area of the ischium where nerves pass through c. Ischial tuberosity – often called our sitting bones, is what we sit upon. This is also a major site for muscle attachment. d. Ramus – this is what joins with the pubis and together they surround the obturator foramen. Figure 6 Figure 7 AAIMT© Appendicular Skeletal Markings Document 9 Revised: October 11, 2006 Figure 8 IV. Lower Limbs (a total of 60 bones) – each limb consists of a femur which makes up the thigh, a patella which is the knee cap, a tibia and fibula which make up the lower leg, tarsals which are the ankle, metatarsals which make up the foot, and phalanges which make the toes. A. Function 1. Levers to move the legs 2. Muscle attachment sites so movement can take place 3. Support of the trunk and movement in space for the entire body B. Structure AAIMT© Appendicular Skeletal Markings Document 10 Revised: October 11, 2006 1. Femur – this is the longest and heaviest bone in the body and includes the following features (Figure 9): a. Body or shaft – this bows medially so that it is closer to the other femur at the distal end than it is at the proximal end. b. Head – this is the rounded projection that fits into the acetabulum of the coxal bone to form the actual hip joint. c. Neck – this is the area just distal to the head and is where the tendons and ligaments wrap around as they connect the femur to the coxal bone. A common fracture in the elderly happens here. With the loss of calcium the neck becomes weak so that it can no longer support the weight of the body. d. Greater trochanter – a projection laterally that serves as a point of attachment for many muscles of the hip and thigh. e. Lesser trochanter – a projection medially and inferiorly that serves as an attachment site for two of the hip flexor muscles. f. Intertrochanteric line or crest – this is the area between the two trochanters and serves as a site of muscle attachment. g. Linea aspera – this is a rough vertical ridge on the posterior surface of the femur and serves as an attachment site for several thigh muscles. h. Medial condyle – this is at the medial distal end of the femur and is an expanded area. This, along with the lateral condyle, is what articulates with the tibia of the lower leg (knee joint). i. Lateral condyle – this is the other expanded area at the distal end of the femur, but on the lateral side. Both condyles are attachment sites for muscles. j. Medial epicondyle – epi means above or upon. This is the area just superior to the condyle and serves as an attachment site for muscles. k. Lateral epicondyle – this is the same as the medial epicondyle, but on the lateral side of the femur. AAIMT© Appendicular Skeletal Markings Document 11 Revised: October 11, 2006 Figure 9 2. Patella – this is commonly called the kneecap. It is a small, triangular bone anterior to the knee joint. It is a sesamoids bone that develops in the tendon of the quadriceps femoris muscle group. (Figure 10) a. Base – this is the broad superior end of the patella. b. Apex – this is the pointed, inferior end of the patella. c. Articular facets – there are two of these and are located on the posterior surface of the patella. This is where the medial and lateral condyles articulate with the patella. 3. Tibia – this is commonly called the shinbone and is the larger of the two lower leg bones. The tibia is in the medial side of the lower leg and bears the major portion of the weight of the leg. The following features are included (Figure 10): AAIMT© Appendicular Skeletal Markings Document 12 Revised: October 11, 2006 a. Lateral condyle – this is at the proximal end of the tibia. It is an expanded area to articulate with the lateral condyle of the femur. Also the inferior surface articulates with the head of the fibula. b. Medial condyle – also at the proximal end of the tibia and is an expanded area to articulate with the medial condyle of the femur. c. Intercondylar eminence – This separates the slightly concave condyles and is an upward projection. d. Tibial tuberosity – this is on the anterior surface of the tibia at the proximal end. It serves as a point of attachment for the patellar ligament and therefore the quadriceps group of muscles. e. Medial malleolus – this is on the medial surface of the distal end of the tibia and articulates with the talus bone of the ankle forming the prominence that can be felt on the medial side of an ankle. f. Fibular notch – this is the area on the lateral surface of the distal end of the fibula. This is what articulates with the fibula. 4. Fibula – this runs parallel and lateral to the tibia and is quite a bit smaller. This is not a weight bearing bone. (Figure 10) a. Head – this is at the proximal end of the fibula and articulates with the inferior surface of the lateral condyle of the tibia just below the level of the knee joint. b. Lateral malleolus – this is at the distal end of the fibula and is a projection which articulates with the talus bone of the ankle forming a prominence on the lateral surface of the ankle. A fracture of the lower end of the fibula with injury to the tibial articulation is called Pott’s fracture. AAIMT© Appendicular Skeletal Markings Document 13 Revised: October 11, 2006 Figure 10 5. Foot, ankle, arch and toes (26 bones). These bones are found in the ankle, instep, and five toes. (Figure 11) a. Tarsals – this is a collection of seven bones of the ankle. The term tarsos (Latin) means a broad, flat surface. 1) Talus – located on the posterior portion of the foot, directly under the tibia and fibula. This is the only ankle bone that articulates with the two lower leg bones. It is bordered by the medial and lateral malleoli for support. During walking, it initially bears the entire weight of the body, then half of this weight is transmitted to the other tarsal bones. AAIMT© Appendicular Skeletal Markings Document 14 Revised: October 11, 2006 2) Calcaneus – also located on the posterior part of the foot, it is also known as the heel bone serving as a place of attachment for the Achilles tendon. It is the strongest and largest of the tarsal bones. 3) Cuboid – One of the anterior ankle bones on the lateral side of the ankle. 4) Navicular – Also on the anterior surface, but medially placed in the ankle. 5) Lateral, Intermediate and Medial cuneiforms – these are also on the anterior surface, distal to the navicular on the medial side of the ankle. They are also known as the first, second and third cuneiforms. b. Metatarsals (5 bones numbered 1 through 5) – these make up what’s called the instep of the foot. The distal ends, or heads, form what’s called the ball of the foot. Along with the tarsals, these bones form the arches of the foot (longitudinal and transverse). It is this arch area that gives a person “spring to their step.” c. Phalanges (14 bones total, 3 per each toe except the great toe which has only 2) – these bones make up the toes of each foot. d. Arches of the foot - these are what allow the foot to support the entire weight of the body and be able to move it through space. 1) There are two parts that make up the longitudinal arch. Both have tarsal and metatarsal bones within them arranged to form an arch from the anterior to the posterior part of the foot. The medial longitudinal arch originates at the calcaneus. From there it goes to the talus and navicular, the three cuneiforms, and the three medial metatarsals. The talus is the keystone of this arch. The lateral longitudinal arch also begins at the calcaneus and continues on to the cuboid and then the two lateral metatarsals. The cuboid is the keystone of this arch. 2) The transverse arch is formed by the calcaneus, navicular, cuboid, and the posterior parts of the five metatarsals. AAIMT© Appendicular Skeletal Markings Document 15 Revised: October 11, 2006 Figure 11 AAIMT© Appendicular Skeletal Markings Document 16 Revised: October 11, 2006 Clinical Information for the Above Outline Foot • • • • • • The bones composing the arches are held in position by ligaments and tendons. If these ligaments and tendons holding the bones together weaken, fallen arches, flat feet, and/or plantar fasciitis can result. Clawfoot is a condition in which the medial longitudinal arch is abnormally elevated. It is frequently caused by muscle imbalance or a condition called poliomyelitis. Hallux Valgus, commonly called bunions, (Hallux= referring to the great toe, Valgus=bent outward) is a deformity of the great toe. Although the cond9ition may be inherited, it is typically caused by wearing tightly fitting, pointed toed shoes along with hyperpronation and is characterized by lateral deviation of the great toe, with partial dislocation at its junction with metatarsal #1. As a result, the head of metatarsal #1 is displaced medially. The condition produces inflammation of bursae, bone spurs, and calluses. Polydactyly – this is a minor defect of the extremities (both hands and feet) and are relatively common. This is extra digits, usually it is incompletely formed and does not function. It is inherited and can be surgically corrected. Syndactyly – this is webbed digits (could be either feet or hands) and is also quite common. This is inherited and can be surgically corrected. Talipes – this is commonly called clubfoot and is a congenital malformation in which the sole of the foot is twisted medially. It is not certain if abnormal positioning or restricted movement in utero causes this condition, but both genetics and environmental factors are involved in most cases. It is usually effectively treated surgically if the procedure is done at a very early age. Lower Leg • Shinsplints (tibia stress syndrome) is soreness and pain along the tibia, usually caused by inflammation of the periosteum (periostitis) brought about by the repeated pulling of the muscles and tendons attached to the periosteum. The condition may occur due to walking or running up and down hills, or by vigorous activity of the legs following a period of relative inactivity. Rest may alleviate the pain. Cryotherapy and massage therapy should be considered as treatment here. Often a person with this condition will be given local injections of cortisone-like steroid drugs of undergo surgery to release pressure in the soft tissues. Both of these are extremely invasive and a person would be better off utilizing the ice and massage. • Fractures of the lateral and medial malleolus are common in skiers. These are commonly called Pott’s fractures and result from a shearing force occurring at a vulnerable spot on the leg. • Stress Fractures – these are very common in the leg and occurs due to repetitive mechanical stress on the bone caused by jarring impact. Areas commonly affected are the metatarsals, fibula and tibia. Running on hard surfaces, high impact aerobic exercises, osteoporosis and obesity are some of the predisposing factors. AAIMT© Appendicular Skeletal Markings Document 17 Revised: October 11, 2006 Knee - Thigh • Patellar Tendonitis – this is also known as jumper’s knee. This is an overuse injury characterized by pathological changes in the quadriceps and the patellar tendon. It is more common in of volleyball, basketball and sports that involve jumping. It presents as pain and tenderness in the anterior aspect of the knee. • Chondromalasia spelling!! Explain Here • Patella Fractures – this can happen by a direct blow. It usually does not fragment due to it being confined within the tendon. • Patella Dislocations – may result from an injury or may be congenital due to the underdevelopment of the lateral condyle of the femur. • Hip Fractures – there are two different groups of people having hip fractures: those over 60 years of age when their bones have been weakened by osteoporosis along with young, healthy professional athletes who subject their hips to extreme forces. Usually the blood supply to the femur and pelvis is compromised with bone cell death or the articular cartilage is damaged beyond repair. One treatment option is joint replacement surgery. Often, if left to repair, there is a need for a titanium rod to be placed in the surgical neck of the femur. Pelvis • The structure of the human pelvis in its attachment to the vertebral column, permits an upright posture and locomotion on two legs (bipedalism) rather than on four legs like other mammals. Although this structural arrangement is well adapted for bipedal locomotion, an upright posture may cause problems. The sacroiliac joint may weaken with age, causing low back pain. The weight of the viscera may weaken the walls of the lower abdominal area and cause hernias. Some of the problems of childbirth are related to the structure of the mother’s pelvis. Finally, the hip joint tends to deteriorate with age. • Pelvimetry is the measurement of the size of the inlet and outlet of the birth canal. Measurement of the pelvic cavity is important due the fetus passing through the opening at birth. Hand • The hand is a marvel of structural organization that, despite its complexity, can withstand considerable abuse. Other than sprained fingers and dislocation, the most common skeletal injury is a fracture to the scaphoid bone of the wrist (about 70% of carpal fractures occur here). Wrist • Dorsal Radiocarpal Impingement Syndrome – this occurs due to repetitive wrist dorsiflexion, especially when performed with an extra load or force as in gymnastics during beam exercises, floor exercises or jumping. Impingement occurs in the dorsal aspect of the radiocarpal joint in this condition and there is pain over the wrist. • Carpal Tunnel Syndrome – this is due to inflammation, swelling, etc. of the structures passing through the carpal tunnel and then compression occurs of the median nerve. This results in sensations in the skin and control of muscles supplied by this nerve being affected. Pain, tingling and loss of wrist mobility are some of the common symptoms. AAIMT© Appendicular Skeletal Markings Document 18 Revised: October 11, 2006 Arm • • When a person falls on an outstretched arm, the radius bears the brunt of forces transmitted through the hand. If a fracture occurs due to a fall like this, it is usually going to be a transverse break about one inch from the distal end of the bone (either the radius or ulna). This is called a Colles’ fracture – the hand is displaced backward and upward. Another common fracture due to this type of fall is a fracture to the head of the radius as it is driven forcefully against the capitulum. The medical term for tennis elbow is lateral epicondylitis, which means an inflammation of the tissues surrounding the lateral epicondyle of the humerus. Six muscles that control backward movement of the hand and fingers, or extension, all originate on the lateral epicondyle. Repeated strenuous contractions of these muscles, as in striking a ball with a tennis racket, may cause a strain on the periosteum and tendinous attachments, resulting in tenderness and pain around the epicondyle. Binding may ease the pain, but only rest can eliminate the causative factor involved. Massage therapy also helps the condition heal properly. Clavicle • Because of the position of the clavicle, it transmits forces from the upper extremity to the trunk. If these forces are excessive such as when falling on an outstretched arm, a fracture in the clavicle may happen. This is the most frequently broken bone in the body. • A shoulder separation is a dislocation of the acromioclavicular joint. Scapula • The anatomy of the scapula is important to know because there are 15 muscles that attach to it. Clinically, the pectoral girdle is significant because the clavicle and acromion of the scapula are frequently fractured in trying to break a fall. • Impingement Syndromes – The rotator cuff muscles pass through a bony tunnel bounded by ligaments and parts of the scapula before inserting into the humerus. Any condition that reduces this space compromises the rotator cuff and produces symptoms of impingement. Usually, impingement syndromes present as a painful arc between 70 and 140 degrees of abduction. Usually there will be pain on resisted external rotation of the arm in abduction. Ribs • • Fractures to ribs usually result from a direct blow. Most commonly this is from a steering wheel impact, falling onto stairs or something similar or a crushing injury to the chest. Ribs usually break at the weakest point, the area of greatest curvature anterior to the costal angle. With children, the ribs are highly elastic and fractures are less frequent then with adults. The first two ribs are protected by the clavicle and the very large pectoralis major muscle. The last two ribs are mobile. These four ribs are the least commonly injured. It is the ribs in between that are most commonly fractured. If the fracture is bad, the injury may extend to the heart, great vessels of the heart, longs, trachea, bronchi, esophagus, spleen, and liver. Surgical access to the lungs or structures in the mediastinum is commonly undertaken through an intercostals space. Tools such as rib retractors are used to widen the AAIMT© Appendicular Skeletal Markings Document 19 Revised: October 11, 2006 separation between ribs. The costal cartilages are quite elastic and will permit quite a bit of bending. Sternum • As the sternum is rich in red bone marrow throughout life and is readily accessible, it is a common site for marrow biopsy. Under local anesthetic, a wide-bore needle is placed into the marrow cavity of the sternum for aspiration of a sample of red bone marrow. This is called a sternal puncture. • The sternum can also be split in the midsagittal plane to allow a surgeon to access the mediastinal structures such as the thymus, heart, and great vessels of the heart. Coccyx • When a person sits, the coccyx flexes anteriorly acting as a shock absorber. A fall on the coccyx may cause a painful subperiosteal bruising, fracture, or fracture/dislocation of the sacrococcygeal joint. • A difficult childbirth can injure the coccyx of the mother. • Coccygeal trauma is painful and may require months to heal. Vertebrae • Whiplash – this occurs at the neck area and is a general term for injury to the cervical region. Muscle, bone, or ligament injury in this portion of the spinal column is relatively common in individuals involved in automobile and sports-related accidents. Joint dislocation without vertebral fracture occurs commonly between the fourth and fifth or fifth and sixth cervical vertebrae, where mobility is greatest. Bilateral dislocations are particularly dangerous because of the probability of spinal cord injury. Compression fractures of the bodies of the first three cervical vertebrae are common and follow abrupt forced flexion of the neck. These fractures may be extremely painful because of compresses spinal nerves. • Cervical Rib – on occasion there may be a rib from the lower cervical vertebrae present. This may press on the nerves of the brachial plexus and produce pain, numbness or loss of control of muscles supplied by the nerves. • Abnormal Spinal Curvatures – on occasion the spinal curvatures are abnormal. An exaggerated thoracic curvature is called kyphosis (hump back). An abnormal lumbar curvature is termed lordosis. If the vertebrae have abnormal lateral curves it is called scoliosis. • In children, the fusion between the dens and the axis is incomplete. Severe shaping or impact can cause the dens to dislocate and damage the spinal cord. AAIMT© Appendicular Skeletal Markings Document 20 Revised: October 11, 2006