* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download months
Survey
Document related concepts
Transcript
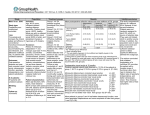
Posterior Capsule Opacification After Implantation of Hydrophilic or Hydrophobic Acrylic IOL Takeshi Iwase, MD, PhD Wilmer Eye Institute Johns Hopkins Hospital The author has no financial or proprietary interest. Introduction Posterior capsule opacification (PCO) is still the most common complication of primary cataract surgery. Many kinds of IOLs composed of various different optic materials have been developed to prevent PCO. The one of hydrophilic IOLs currently available worldwide is Hydroview IOL (H60M and HP60M, Bausch & Lomb) and several studies reported that patients with hydrophilic IOLs developed greater PCO than with other optic materials. However, there is an important limitation in those studies, most of them compared between hydrophilic IOLs with round optic edge and hydrophobic with sharp optic edge or the observation period is relatively short (under 2years). Purpose Recently, a new developed Hydroview IOL HP60M is introduced to prevent PCO by having sharp optic edge, double square-edge. To our best knowledge, there is no report to compare hydrophilic double square-edged Hydroview IOL HP60M with other IOL. The objective of this prospective study was to evaluate the influence of hydrophilic single-piece foldable acrylic square-edged IOLs on the development of PCO, compared with hydrophobic IOL (AcrySofョ SA60AT, Alcon Laboratories, Inc.) for 2 years after surgery. Patients 126 eyes of 63 patients with bilateral senile cataract and no other ocular diseases were prospectively randomized to receive a hydrophobic acrylic (SA60AT) or hydrophilic acrylic single piece IOL (HP60M). All patients were followed for twenty-four months after the surgery. Exclusion criteria were ocular pathology other than senile cataract, history of intraocular surgery, a pupillary diameter less than 6.0 mm after full dilation, uveitis, retinitis pigmentosa, pseudoexfoliation syndrome glaucoma, and axial length longer than 25 mm or shorter than 21 mm. Incomplete CCC included anterior capsular crack formation and incomplete overlap of the IOL optic. Surgery A 3.0 mm wide self-sealing temporal sclerocorneal tunnel was created. The anterior chamber was filled with a viscoelastic material, and a 5.0 mm to 5.25 mm CCC, slightly smaller than the IOL optics diameter, was made to attain circumferential 360-degree capsulorhexis-IOL overlap. Thorough hydrodissection, phacoemulsification of the nucleus, and aspiration of the residual cortex was performed. The wound was not enlarged and the SA60AT and HP60M IOLs were inserted in the capsular bag using the Monarch II injector. Postoperatively, all patients received similar routine medication, comprising topical application of diclofenac sodium, 0.1 % fluorometholone and ofloxacin administered four times daily for 1 month. Methods 1. Changes in mean posterior PCO value in the HP60M and SA60AT groups. The PCO density value was measured using Scheimpflug video photography (EAS-1000, NIDEK) at 1, 6, 12, 18, and 24 months after surgery. 2. Kaplan-Meier survival plots of the two groups for eyes not requiring Nd:YAG laser posterior capsulotomy. The number of eyes that required capsulotomy were also examined.. 3. Changes in mean (SD) visual acuity in the HP60M and SA60AT groups. Best corrected visual acuity on decimal charts was recorded at each visit and this acuity was converted to logMAR for statistical analysis. PCO Value 1. Changes in mean (SD) posterior PCO value in the hydrogel and acrylic IOL groups. (CCT) 40 35 30 25 20 15 10 5 0 SA60AT * P<0.01 HP60M * 1 week * 1 3 6 12 18 24 month months months months months months Time after surgery The PCO value in the hydrogel group increased significantly(p<0.01), while the change in the PCO value was not significant in the acrylic group. The mean PCO value in the hydrogel IOL group was significantly greater than that in the acrylic group 18 and 24 month after surgery. 2. Kaplan-Meier survival plots of the two groups for eyes not requiring Nd:YAG laser posterior capsulotomy. (%) 63 eyes 1 eye Survival rate 100 8 eyes 80 60 SA60AT 40 HP60M 20 0 5 10 15 20 25 (months) Time after surgery The survival curve in the hydrogel group was significantly worse than that in the acrylic group (p<0.01, Mantel-Cox log rank test). 3. Changes in mean (SD) visual acuity in the hydrogel and acrylic IOL groups. Time after surgery Visual Acuity 20/15 1 week 1 6 12 18 24 month months months months months SA60AT HP60M 20/20 20/25 * * *P<0.01 20/40 Mean visual acuity in the hydrogel group was worse than that in the acrylic group; this difference was significant at 18 and 24 months after surgery. Discussion Because the IOLs were implanted using same surgical technique and have similar IOL optic design such as sharp edge and diameter of 6 mm, the degree of PCO in the both groups was mainly related to the different IOL materials. Both the sharpness of the bend and the speed of its formation are important factors for PCO and the differences in speed may be influenced by the IOL material. In hydrophilic IOL, there is less epithelial–mesenchymal transition in LECs with this more biocompatible material. As a result, there may be less contraction-induced reduction in the size of the residual capsular bag, which would leave space and allow cells to migrate onto the inner surface of the posterior capsule before the posterior capsule adheres to the posterior surface of the IOL. Furthermore, it was reported that histopathologic and TEM evaluations of hydrogel IOLs showed the hydrophilic surface properties provide an optimum matrix for LECs and cortical proliferation and migration from the equatorial region toward the center of the visual axis, leading to the higher degree of PCO. Conclusion The hydrophilic IOL HP60M resulted in significantly more PCO 2 years after surgery compared with the hydrophobic acrylic IOL SA60AT. The results of previous and current studies suggest that hydrophilic material may allow active proliferation of lens epithelial cells, possibly because of its hydrophilicity, and therefore may not be appropriate for use as an optic material. Further study is needed to examine the extent of PCO with the other types of IOL that have hydrophilic properties.