* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Stroke
Survey
Document related concepts
Transcript
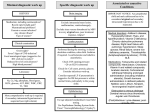
Clinical Program for Cerebrovascular Disorders Mount Sinai Medical Center Stroke Associated with Intracranial Vascular Disease and A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial) Clinical Case Presentation Clara Raquel Epstein, MD Fellow Stroke Associated with Intracranial Vascular Disease - Pathogenesis • Occlusion – Atheromatous/Thrombotic • Large Vessel Occlusion or Stenosis (ie. Carotid A.) • Branch Vessel Occlusion or Stenosis (ie. Middle Cerebral A.) • Perforating Vessel Occlusions (ie. Lacunar infarction) – Non-atheromatous Diseases of the Vessel Wall • • • • Collagen Disease (ie. Rheumatoid arthritis, SLE) Vasculitis (ie. Polyarteritis Nodosa, Temporal Arteritis) Granulomatous Vasculitis (ie. Wegener’s granulomatosis Miscellaneous (ie. Syphilitic vasculitis, fibromuscular dysplasi, sarcoidosis, trauma) Stroke Associated with Intracranial Vascular Disease - Pathogenesis • Embolization – Atheromatous plaque in the intracranial or extracranial or extracranial arteries or from the aortic arch. – The heart • • • • • • • valvular heart disease arrhythmias ischemic heart disease bacterial endocarditis atrial myxoma prosthetic valves patent foramen ovale – Miscellaneous- fat, air, or tumor emboli Stroke Associated with Intracranial Vascular Disease - Vasculitis and Collagen Vascular Diseases • Collagen Vascular Diseases – Systemic lupus erythematosus – Rheumatoid arthritis • Vasculitis – – – – – – Associated with connective tissue disease Polyarteritis nodosa (PAN) Takayasu’s arteritis Isolated angiitis of the central nervous system Giant cell arteritis/Temporal arteritis Churg-Strauss angiitis • Granulomatous vasculitis (ie. Wegener’s Stroke Associated with Intracranial Vascular Disease - Pathogenesis • Coagulopathies • Venous Thrombosis (ie. Infection and dehydration) • Decreased Cerebral Perfusion (ie. Cardiac dysrythmia, GI blood loss) • Hemorrhage Stroke Associated with Intracranial Vascular Disease Clinical Case Presentation • A 68 year old right handed Haitian male with a history of hypertension presented to the Mount Sinai Medical Center Emergency Department with complaints of left sided weakness (leg greater than arm) which had been present on awakening four days prior to admission. Per history the patient was previously taking Vasotec for 15 years but had self discontinued his medications approximately one year prior to admission. Stroke Associated with Intracranial Vascular Disease Clinical Case Presentation Hospital Course On initial examination the patient was found to have a left facial droop, a mild left upper extremity pronator drift, decreased rapid arm movement on the left and proximal left lower extremity weakness of 4/5. Pinprick and proprioceptive sensory deficits were evident in a stocking glove distribution. The patient demonstrated a left hemiparetic gait. Stroke Associated with Intracranial Vascular Disease Clinical Case Presentation Hospital Course The patient was admitted to the Stroke Unit for further diagnostic evaluation and intervention. A non-contrast head CT was obtained on admission which revealed hypodensities in the left internal capsule and in the right Globus Pallidus compatible with ischemia. It was suggested that this could represent lacunar strokes. He was initially started on aspirin, lisinopril, simvistatin and glyburide. On hospital day #3 the patient was then started on heparin per protocol and the aspirin was discontinued. Coumadin was then started on hospital day #7. Stroke Associated with Intracranial Vascular Disease Clinical Case Presentation Hospital Course Further evaluation included MRI and MRA with diffusion and cerebral angiography. The MRI/A revealed increased signal on flair and diffusion in the right basis pontis indicating acute infarction. This area corresponds to the right posterior cerebral artery narrowing which was visualized on the MRA. There also appeared to be narrowing of the distal vertebral artery at its junction with the basilar artery. In addition, some stenosis of the basilar artery appeared to be present. Stroke Associated with Intracranial Vascular Disease Clinical Case Presentation Hospital Course The cerebral angiography showed evidence of atherosclerotic narrowing of the distal left vertebral intradural segment. The luminal caliber is less than what would be expected for normal anatomic tapering. The degree of stenosis is approximately 60% as compared with the normal intradural vertebral artery proximally. Mild atherosclerotic narrowing of the distal right vertebral artery intradural portion. The degree of stenosis is mild and approximately 40% as compared with the vessel proximally. A small focal smooth atherosclerotic plaque within the midbasilar artery at the right lateral wall producing no significant narrowing of the vessel lumen was also seen. Mild atherosclerotic change within the bilateral posterior cerebral arteries without significant focal stenosis was seen. Minimal atherosclerotic change of the right internal carotid artery origin was also seen. Adam Davis, MD Interventional Neuroradiology CT Head 12/29/99 CT Head 12/29/99 MRI Sagittal T1 12/30/99 MRI Axial Flair 12/30/99 MRI Axial Flair 12/30/99 MRI Axial T2 12/30/99 MRI Axial T2 12/30/99 MRI Diffusion 12/30/99 MRA Posterior Circulation 12/30/99 MRA Right PCA 12/30/99 MRA Posterior Circulation 12/30/99 A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial) A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial Funding Source: National Institute of Neurological Disorders and Stroke Coordinating Center: Emory University Principal Investigator: Marc I. Chimowitz, MBChB Associate Professor of Neurology Emory University Hospital A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • The major goal of this 5 year multi-center trial is to determine optimal antithrombotic for symptomatic atherosclerotic intracranial arterial stenosis. Atherosclerotic stenosis of the major intracranial arteries (carotid siphon, middle cerebral artery, vertebral artery, basilar artery) is an important cause of ischemic stroke, especially in Blacks, Asians, and Hispanics. In the USA, intracranial stenosis causes approximately 40,000 ischemic strokes annually ie. 10% of ischemic strokes. Moreover, the risk of recurrent strokes in these patients 4%-15% per year. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Despite the importance of intracranial stenosis as a cause of ischemic stroke, the treatment of this disease remains empirical. Antiplatelet agents (aspirin or ticlopidine) are frequently used in this setting based on studies that have shown a benefit of these agents for lowering the risk of stroke in patients with non-cardioembolic TIA or minor stroke. However, the efficacy of antiplatelet agents has not been established in patients with symptomatic intracranial large artery disease. In fact, the high rate of stroke in patients with carotid siphon or middle cerebral artery stenosis who were treated with aspirin in the medical arm of the Extracranial-Intracranial (EC_IC) Bypass Study (approximately 10% per patient year) raises a question about the efficacy of aspirin in this setting. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Warfarin is also frequently used for the treatment of symptomatic intracranial large artery disease based on retrospective data that suggests warfarin may lower the risk of stroke in patients with carotid or vertebro-basilar TIAs. In a retrospective, nonrandomized, multicenter pilot study performed by our study group, warfarin was compared with aspirin for prevention of major ischemic vascular events (stroke, myocardial infarction (MI) or vascular death) in 151 patients with TIA or stroke attributed to stenosis (50-99%) of a major intracranial artery. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Overall, the relative risk of a major ischemic event in patients treated with warfarin was 0.45 compared with patients treated with aspirin. A Kaplan Meier analysis that included hemorrhagic deaths as a primary end point (ie. In addition to ischemic stroke, MI or sudden death) showed that a significantly higher proportion of patients treated with warfarin survived free of these end points compared with patiens treated with aspirin. Patients with moderate intracranial stenosis (50%-69%) had a lower risk of stroke in the same vascular territory than patients with severe intracranial stenosis (70-99%). Of 62 patients with 50-69% intracranial , five patients (8%) had a stroke in the same territory as the stenotic artery during a median followup of 20 months (4 of 28 (14%) on aspirin, 1 of 34 (3%) on warfarin). In comparison, of 89 patients with 70-99% intracraninal stenosis, nine patients (10%) had a stroke in the same territory as the stenotic artery during a median followup of 14 months (5 of 35 (14%) on aspirin, 4 of 54(7%) on warfarin). A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Transluminal angioplasty is another therapeutic option for the treatment of intracranial stenosis. Early experience suggested that intracranial angioplasty was associated with an unacceptably high risk of stroke or death and the procedure was largely abandoned. However, recent advances in microcatheter and balloon technology have led to renewed interest in intracranial angioplasy. Several recent studies of small series of patients have shown that intracranial angioplasy is technically feasible and may be performed relatively safely. In these studies, the risk of stroke during angioplasy was 0%-11.7% and the risk of stroke during followup was 2%-4% per year. These recent studies suggest that angioplasy is a promising therapy that is increasingly being used to treat symptomatic intracranialstenosis A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • The Primary Specific Aim of this randomized, doubleblind, multi-center clinical trial is to compare the efficacy and safety of warfarin (INR 2-3) with high dose aspirin (1300 mg per day) for preventing stroke (ischemic and hemorrhagic) and vascular death in patients with transient ischemic attack (TIA) or non-severe stroke caused by symptomatic stenosis of a major intracranial artery. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • The Secondary Specific Aim is to identify patients whose rate of ischemic stroke in the territory of the stenotic intracranial artery on best medical therapy is sufficiently high (ie. >6% per year) to justify a subsequent trial comparing intracranial angioplasty with best medical therapy in these patients. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Primary Hypothesis: Warfarin (INR 2-3) reduces the rate of stroke (ischemic and hemorrhagic) and vascular death by 33% over three years compared with high dose aspirin (1300 mg per day) in patients with TIA or non-severe stroke caused by >50% stenosis of a major intracranial artery (intracranial carotid artery, MCA, intracranial vertebral artery, basilar artery). A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Secondary Hypothesis: In the best medical therapy group, the rate of ischemic stroke in the territory of the stenotic intracranial artery will be 3% per year in patient with 50%69% intracranial stenosis and .6% per year in patients with 70%-99% intracranial stenosis. A Discussion of WASID (The Warfarin-Aspirin Symptomatic Intracranial Disease Trial • Criteria for measuring percent stenosis of the major intracranial arteries were adapted from the NASCET method for measuring percent diameter stenosis of the extracranial internal carotid artery. The diameter of the extracranial internal carotid artery at the site of stenosis (D stenosis) is compared with the normal diameter of the artery just distal to the stenosis (D distal) using the following formula: % stenosis = (1-(D stenosis/ D distal)) x 100%