* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download document 3066482
Survey
Document related concepts
Transcript
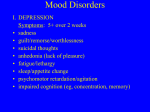
Rockland County Depression and Bipolar Support Alliance Volume 1, Issue 4 December, 2014 UP CLOSE AND PERSONAL or Ten Questions I have for My Depression by Ralph Inglese President’s Message by Leslie Davis Year in Review and What’s Up For the Future of DBSA Q1: Why Me? Greetings to all. This is my first President’s Message in this newsletter. This has been quite a year for Rockland DBSA. We continue to grow and provide more services for all of our members. January brought us the first issue of our quarterly newsletter. This was met with accolades from many areas of the mental health community. It has kept our members informed, given them an avenue for their expressions through writings such as poetry, and lets the mental health community know who we are. In April we hosted our first facilitator training which was presented by DBSA national. Our two day program had attendees from New York, Connecticut, New Jersey and Pennsylvania. We had 2 great speakers during the year. In March, Venkatesh T. Sawkar, M.D. spoke about Electroconvulsive Therapy (ECT) Continued on Page 5 INSIDE THIS ISSUE 1 Message from the President 1 10 Questions for Depression 2 Advisor’s Column: PTSD 6 Writings From Our Members 7 Blood Test for Depression 11 Mistakes When Depressed or Having Panic 13 Treating Depression to Prevent Suicide 15 Ask the Doc A: My pat answer is…why not you? But actually, in case you didn’t notice you didn’t win the genetic lottery. Your mom is classically depressed...your father’s mother was anxiety ridden…and even your step-grandmother (no relation) had a nervous breakdown in the 1940’s. Q2: So I inherited you? A: Yes. You were also brought up in a bubble…leading to a lack of confidence and low self-esteem. I also gave you a nervous stomach. Q3: I remember. Why did I feel so anxious all the time? A: We are a package deal, anxiety and I. The chemical imbalance in your brain lead to a life of confusion. I made sure you were self-absorbed and isolated. Q4: Why was I so uncomfortable in my own skin, even when I tried to be normal? Was that you? A: You got it. I made sure that everything was difficult…like making friends. And at school, I added a touch of perfectionism, so that you had to get the highest grades or suffer the guilt and shame. Continued on page 14 Newsletter 1 Post-Traumatic Stress Disorder by Lois Kroplick, DO, DFAPA Distinguished Fellow American Psychiatric Society WHAT IS PTSD? ANXIETY ORDER After exposure to traumatic events: Actual or threatened death Serious injury Threat to physical integrity self or others Invokes fear, helplessness, or horror CORE PTSD SYMPTOMS Re-Experiencing Avoidance Hyperarousal CRITERIA FOR PTSD REXPERIENCING TRAUMA Flashbacks Nightmares Exaggerated reactions to triggers AVOIDANCE/NUMBING Loss of interest Detached feelings from others Restricted Emotions HYPERAROUSAL Difficulty sleeping or concentration Irritability or bursts of anger Hypervigilance TIME Symptoms last greater than one month FUNCTIONING Impairment in functioning Significant distress RISK FACTORS FOR PTSD Female gender – 20% (Male 8%) War Veterans Previous trauma-childhood trauma Severity of trauma History of anxiety or mood disorder Family history of psychiatric disorders – 30% Genetic vulnerability Very young and very old – increase risk PTSD IN CHILDREN CHANGES IN THE BRAIN STRUCTURAL CHANGES Decreased volume in these areas: Prefrontal Cortex Amygdala Hypothalamus HOW COMMOM IS PTSD Prevalence – 8% Most people who experience trauma don’t get PTSD Occurs at any age Occurs in families Specific traumas associated with PTSD Rape Combat Physical abuse Threat with a weapon BRAIN CHEMISTRY CHANGES Increase in level of stress hormones Low serotonin levels Low dopamine levels High levels of norepinephrine DIFFERENT SYMPTOMS Behavioral symptoms, can’t function at school Cutting, suicide attempts Compulsive risk taking, aggressive, runs away Nightmares, fear of sleeping along Somatic complaints (stomach ache) COMORBIDITY ADHD Depression, Anxiety Substance Abuse Eating Disorders Continued on page3 Newsletter 2 UNDERDIAGNOSIS REASONS Lack of Awareness Denial Shame Complex Comorbid Illness Atypical presentations-Somatic complaints SCREENING FOR PTSD TREATMENTS OF PTSD COGNITIVE BEHAVIORAL THERAPY GOALS Identify distorted thoughts Change thinking patters Often people feel guilt or shame about what isn’t their fault EXAMPLE: Patient has nightmares after trauma ELICIT A TRAUMA HISTORY Ask if the patient has experienced trauma Physical abuse Sexual abuse CAPS (Clinician-Administered PTSD Scale) PCL (Patient self-rating-PTSD checklist COMORBIDTY OF PTSD Alcohol abuse Depression Social Anxiety Disorder Generalized Anxiety Disorder Panic Disorder Irrational Thought: I will never sleep again Rational Thought: I am struggling with sleeping right now, but this is a normal reaction to stress Irrational Thought: I will die from this stress. Rational Though: I will continue to seek help. IMPACT of COMORBIDITY 80% PTSD sufferers have on comorbid disorder PTSD often develops with prior psychiatric disorder PTSD is associated with onset of other disorders EXPOSURE THERAPY TYPES OF PTSD ACUTE PTSD Symptoms begin 1st month Last up to 3 months CHRONIC PTSD Symptoms persist > 3 months DELAYED PTSD Months of years before all symptoms appear TREATMENT OF PTSD Therapy Medications Combined Approach is Best GOALS OF TREATMENT Reduce symptoms Improve resilience Improve quality of life Reduce Disability Reduce Comorbidity CBT-identify distorted thoughts Exposure Therapy-Imagine and real life Anxiety Management Debriefing-directly after the event EMDR-eye movement desensitization & reprocessing GOALS Help people face and control their fears. Exposes them to trauma they experienced safely Uses mental imagery, writing, visiting place of trauma RULES OF DESENSITIZATION Don’t jump into exposure therapy Always prepare before the therapy Pair the negative thoughts with positive emotions ANXIETY MANAGEMENT (STRESS INOCULATION TRAINING) Relaxation exercises Yoga Meditation Learn to identify triggers of you anxiety GOALS Reduce PTSD symptoms Reduce anxiety Look at trauma in a healthy way Continued on page 4 Newsletter 3 DEBRIEFING DEFINITION Highly aroused trauma patients express feelings directly after the incident One session only RESULT Doesn’t reduce PTSD symptoms Can exacerbate the symptoms of PTSD Recommendations: not to do single sessions EMDR EYE MOVEMENT DESENSITIZATION AND REPROCESSING PROCEDURE Move your eyes back & forth rapidly while concentrating on a distressing memory Patient articulate a negative cognition and replaces it with a positive cognition Ex: Replace “I feel ashamed.” “I am proud.” Rate the distress and strength of belief in positive cognition and repeat this procedure. SELF CARE ESSENTIAL TO RECOVERY Sleep Eating Habits Exercise Structure Your Day & Set Daily Goals Have a Support System MEDICATIONS SSRI’s Zoloft Paxil ADJUNCT MEDICATIONS –For SLEEP Remeron Topamax Prazosin Atypical Antipsychotics Research: Namenda, D-Cycloserine CHALLENGES TO EFFECTIVE MEDICATION TREATMENT Self-medicating with alcohol/drugs Feeling that meds are a crutch or weakness Fear of addiction CONCLUSION Taking it only when symptoms are sever Under/Misdiagnosed Not remembering to take the meds High comorbidity-substance abuse/depression POST TRAUMATIC GROWTH HOW DO PEOPLE RECOVER? Resiliency Mission/Purpose Social Supports Frequently seen in Primary Care Remission is attainable Therapy and medications (SSRI’s) best approach Rockland County Depression and Bipolar Support Alliance 4 President’s Message Continued and in September Lois Kroplick, DO spoke about Post Traumatic Stress Disorder (PTSD). Parts of Dr. Kroplick’s talk are on pages 2-4 of this newsletter under Advisor’s Column. We co-sponsored two programs with NAMI: the Mental Health Coalition Public Forum on Schizophrenia. We also co-sponsored, with NAMI a program entitled The Ups and Downs of Mood Disorders where our medical advisor, Dr. Lois Kroplick spoke on the symptoms, risks and treatment of mood disorders, Dr. Stephen Levy spoke about dual diagnosis, and I shared my story of my personal journey to mental health. I was recognized by DBSA National for outstanding leadership for the work done with our Rockland Chapter. New York State Chapter also was recognized by National. We currently have thirteen facilitators as our list of facilitators continues to grow. This year five additional people went through training, either the one that we sponsored or through the New Jersey State DBSA. We currently have 13 facilitators. In addition to a training program, our facilitators are part of an ongoing facilitator development program which was developed by our member Victoria who also heads the facilitator support group. Kudos to all of them. Rockland DBSA is going through a growth spurt, along with growing pains. These are all good things, but we need to figure out where the future of R-DBSA lies. We regularly have fifty people attend our weekly meetings for which we have expanded to five mood disorder share groups as well as a friends and family share group. The DBSA board also grew in numbers. Each of the twelve board members bring a different set of skills to help us move the group forward. A change in officers includes Victoria and Leonard sharing the treasurer position and myself resuming the presidency. Laurie-Jean is continuing as secretary and Eric as Vice-President. Our new board members are Eileen, now serving as co-president, Lydia, Brian and Barbara. However as we continue to grow we must consider how to effectively provide services to everyone who attends our groups. For example we are moving to a larger venue for our weekly meetings, but should we meet more than once a week? Should we have more than one venue for our meetings? How will we find enough volunteers to meet the demands of our membership? What kinds of programming does the membership want? All of these questions and more have taken a substantial amount of discussion time by the Board. To this end, the Board, at its last meeting, voted to develop a survey to get input from those we are serving, our membership. We want to know where you see the group going and how we can accomplish that mission. Attached to this newsletter is a copy of the survey which we encourage everyone to complete. Remember this is your group and we want to do everything in our power to provide you with the best group possible. A special thanks to Steve who developed the survey for us and to all of the members of the Board who provided their input. Rockland DBSA also participated in a focus group with the Rockland County Executive’s Commission on Community Behavioral Health. DBSA members had the opportunity to express their views about the mental health system in Rockland County and to provide input as to where improvements could be made. Finally to all of you, I wish a healthy and enjoyable holiday season. We look forward to another great year for Rockland DBSA. Rockland County Depression and Bipolar Support Alliance 5 Writing From Our Members STANDING OUT IN THE RAIN Feline Oh my, how things have changed. Black cat jumps from sill, > > Chastising red car rounding > The road in surprise. Yes, I was the hippie-era-ish Stone cold sober, a rinsing rain in the summer, fully clothed, we’d just stand there and suck it up. Drenching. Better than a chlorinated pool or even a lawn sprinkler. Such unjudgemental peace…awash of our troubles. I’m 59. In the dark hours before the dawn, I saw the same rain. I took the chance no one was awake to see me do it again. It felt wondrous and healing. A brave thing to do considering my diagnosis. “oh, that crazy woman…she’s standing out in the rain” Barbara Marsel (Out to Dinner Christmas Eve) victoria 2014 I wish things like that wouldn’t happen, I can’t stop myself, I jump into action. Before I realize I’m out of my chair To help the man on the floor get some air. My life is depressing at time, I can’t get the dying out of my mind. It’s hard sometime to let good thoughts through My mind races about people turning blue. My CPR is great My ABC’s top rate But my mind is broken, my spirit crushed Because my heart breaks, I’ve seen too much The sun declines; its few remaining rays Color the lake from shore to farthest shore; The loons cry out; their mournful notes implore An answer from the hills around; deer graze Among the pines; the sun-kissed flowers blaze Their reds and purples out, as though a door To Heaven opened; hummingbirds explore Each blossom avidly as light decays. By Bobbi C., Retired RN Cat Growing Older As Warrior rests on my belly And rises and falls with each of my breaths, He seems an old masted ship on the sea, Rocking and Rolling To some ceaseless rhythm Of eternity. And I, who bear a darkness in my soul, Muse on the world around me, and rejoice That as night grows, there yet is life and light. So, too, when my world spins out of control And darkness comes, I still can make the choice To seek out light even in the darkest night When Warrior dies A piece of his hide Will I save in velvet tin. As the Natives maintained the cords of their mothers, So I will sustain this slice of my life Though it grew not from within. Evening in the Mountains -Steven C. Hohn Barbara Marsel Continued on page 16 Rockland County Depression and Bipolar Support Alliance 6 First blood test to diagnose depression developed Health - September 17, 2014 12:54PM Scientists at Northwestern University have developed the first objective, measurable way to diagnose depression. Who Is Your Board Co-Presidents Leslie Davis [email protected] Eileen Warmbrand [email protected] Vice President Eric Balzer [email protected] Co-Treasurers Victoria Leonard Davis [email protected] Laurie-Jean Secretary Board Members Brian Christgau [email protected] The test analyzes RNA, the molecules that carry out instructions from DNA. By observing how RNA changed after a patient was diagnosed with depression, researchers say they were also able to identify the biological effects of cognitive behavioral therapy. Denny Hirsch [email protected] "Mental health has been where medicine was 100 years ago when physicians diagnosed illnesses or disorders based on symptoms. This study brings us much closer to having laboratory tests that can be used in diagnosis and treatment selection." David Mohr, Northwestern University Feinberg School of Ralph Inglese [email protected] Steven Hohn [email protected] Barbara Marsel [email protected] Medicine Currently depression is diagnosed using subjective, non-specific symptoms such as mood, fatigue and change in appetite. According to the researchers, depressed patients are often unable to adequately describe their symptoms. In 2012, co-lead study author Eva Redei developed a similar test for adolescents. However, most of the RNA blood markers identified in adults are different than those found in young people. First Blood Test to Diagnose Depression in Teens: Northwestern University News http://www.northwestern.edu/newscenter/stories/2012/04 /redei-blood-test.html First Blood Test to Diagnose Depression in Adults: Northwestern University News http://www.northwestern.edu/newscenter/stories/2014/09 /first-blood-test-to-diagnose-depression-in-adults.html First Blood Test to Diagnose Depression in Adults: Northwestern University News http://www.northwestern.edu/newscenter/stories/2014/09 /first-blood-test-to-diagnose-depression Lydia Milbury [email protected] Founder Leslie Davis Newsletter Editor Leslie Davis Advisors Lois Kroplick, DO Mona Begum, MD www.dbsarockland@org [email protected] 845-837-1182 DBSA National: www.dbsalliance.org DBSA New York: www.dbsanystate.org Rockland County Depression and Bipolar Support Alliance 7 If only money grew on trees…we wouldn’t have to ask. We are sending you this letter to ask that you please pledge your continuing support to The Rockland County Depression and Bipolar Support Alliance. In order for our chapter to continue to provide weekly support groups for persons with mood disorders and their friends & families we must again ask for your monetary support. Rockland DBSA is a self-supporting chapter and we do not charge membership fees for our support groups. We must again ask you to send what you are able, so that our chapter can continue to offer its services of support to those in need. Rockland County DBSA is a 501(c) 3 not-for-profit organization and all donations are tax deductible to the extent allowed by law. Operating costs to run our support groups continue to increase. We share a portion of our weekly ‘pass the can’ contributions with St. John’s Church where we meet, which average between $60 – 80 a month. Annual expenses include insurance costs of $1500, National DBSA re-affiliation fees of $125, New York State DBSA fees of $225, and a web page fee of $150. In addition, our mailing fees to publicize our weekly support groups and advertise our semi-annual Speaker Series run in the hundreds of dollars. Our participation in numerous health fairs additionally cost hundreds of dollars for brochures and public awareness. Attendance at our weekly support meetings continues to increase with over forty regular attendees in our Mood Disorder and Friends and Family share groups. To better accommodate the larger membership we have focused on communication and facilitator training this year. Through your past generous contributions we have been able to: Publish a quarterly newsletter; Host a two-day facilitator training event; Institute a Facilitator Support group; Formalize a facilitator training protocol; Increase public awareness In the coming year we hope to further increase our services to the community. To do so we need and appreciate your continued support. Rockland County Depression and Bipolar Support Alliance 8 Please do not wait to send us your donation. With your monetary contribution, Rockland County DBSA can continue with our mission to improve the lives of people living with mood disorders. Sincerely, Rockland County DBSA Leslie Davis, Co-president Eileen Warmbrand, Co-president Tear Off Contribution Card My Rockland DBSA Donation: Your Name: Address: We ask that you make your checks out to ‘Rockland County DBSA’. You may either bring your tear off contribution card and check to a meeting or mail it to: Leslie Davis Rockland County DBSA 13 Case Court Monroe, NY 10950 If you wish to make your donation with a credit card, you may make your contribution through Paypal by simply going to our website www.dbsarockland.org and click the donation tab. Rockland County Depression and Bipolar Support Alliance 9 ROCKLAND COUNTY DEPRESSION and BIPOLAR SUPPORT ALLIANCE IS MOVING TO LARGER, BETTER SPACES Starting with the Thursday Meeting February 12, 2015 we will move to Jawonio, located at 775 North Main Street, New Hempstead, NY 10977 The group will continue to meet from 6:30 – 8:30 pm Here at Jawonio we have at least 9 share group rooms, with additional space to add on. We have a large room that will hold at least 60 people. We have a closet to hold our personal items. We have rooms to have private conversations…and Jawonio is asking for no money from us, and yes there is a kitchen. Rockland County Depression and Bipolar Support Alliance 10 6 Mistakes We Make When Depressed or Having a Panic Attack By Nikolay Perov 1. Resisting. the results if you like. Would it be true to say that it’s not all as terrifying and dreadful as it seemed at first? When we feel a bad mood, depression, or panic coming on, our first wish is to get rid of it as quickly as possible, to change the “bad” mood into a “good” one. This is natural; it’s how we’re made. But all too often our attempts just make everything worse. When you stop feeding your depression with fears and thoughts it becomes much easier to shake off. Resistance forces us to think constantly about our condition, to focus all of our attention on it, to feel bad because it won’t go away, to wait tensely for relief. But the simple truth is that you can’t control everything. Attempting to get your condition “under control” often leads to extra stress and unwanted bad feelings. It’s sometimes best just to relinquish control and cease resistance. If we relax and let our depression or panic come without trying to control anything, accepting that they’re only temporary feelings which will pass in due course, things become much easier. 2. Feeling bad about feeling bad. We start to have thoughts such as “I’m going to die or go crazy,” “This’ll never end,” and “I hate that I can’t enjoy life like other people; I feel utterly miserable.” Our mind starts to add new fears and negative emotions to the depression we already have. And, as I saw for myself, these fears and feelings end up constituting the main part of our condition. It’s actually your mind, not the depression and panic themselves, which makes each episode so unbearable. If you don’t believe me, try this experiment: The next time you’re overwhelmed by an attack, try to simply observe it without getting caught up in or assessing it in any way. Just watch it in its pure form, without any thoughts. Try to notice which parts of your body you feel it in and how it comes and goes. In this way, you’ll remove your mind from the formula of your distress. You’ll notice how much weaker the attacks become when they’re no longer supported by your thought processes. Give it a try, making notes of 3. Comparing. “Everything was so good when I wasn’t depressed! What an amazing time it was, and how awful it is now. Why can’t I go back?!” These are the kinds of things many people think, me included, but such thoughts bring nothing but harm. If you want to beat depression or panic, you have to stop comparing. Forget that there’s a past and future. What’s happened has happened. Don’t dwell on it, and instead live in the here and now. Start with what you have, and don’t think about how it all was before. Learning how to live in the present moment will make your depression or panic much more bearable. 4. Asking pointless questions. Many people spend hours asking themselves all kinds of questions: “When will this end?” “Why me?” and “What have I done to deserve this?” To make use of a well-known Buddhist parable, these questions are as much use as trying to figure out the source of the arrow which blinded you: it’s just not that important. What you need to know is how to pull the arrow out. Questions of the “Why me?” ilk just make your condition worse, forcing you as they do to complain and be upset about something that’s already happened. Focus on what will help you get past your depression and don’t bother with questions which don’t serve this purpose. 5. Believing your fears. We think that because we experience such fear at the idea of going outside, meeting people, or going on the underground, it means that something bad is going to happen. There’s nothing surprising in this, because Rockland County Depression and Bipolar Support Alliance 11 nature has made fear in order to warn us of danger. We’re made in such a way that we instinctively believe this fear and respond to it. But our fear hardly ever arises due to a real threat. For example, the fear of losing your mind or suffocating during a panic attack is simply fallacious. Stop believing this fear. Whatever it is you’re afraid of at these times isn’t going to happen. Fear is nothing more than a feeling, a chemical reaction in your head. If you’re overcome with terror when you go down into the underground, it doesn’t mean that something horrific is laying in wait there. It’s like a malfunctioning fire alarm—just because it’s going off doesn’t mean there’s actually a fire. So stop listening to your “inner alarm” every time it goes off. Don’t pay it any heed: go out, meet your friends, get on a plane, and let the alarm keep ringing. Nor should you try to “switch it off,” as this doesn’t always work. Just ignore it. In other words, stop taking your fear as something real. 6. Seeking reasons for your depression in the outside world. This is another mistake I made myself. I thought that my malaise was linked solely to the way my life and work were going. I believed that if I could just change that, I’d be happy. But then, with meditation, I realized that everything I needed to be happy was inside me, and likewise what was causing me to suffer! I was so edgy, anxious, feeble, caught up in bad habits, undisciplined, and irresponsible that even if I’d succeeded in changing the external circumstances of my life, the traits that had given rise to my depression would still be there. In order to get rid of my depression, I had to get rid of the internal reasons that had caused it. So don’t keep telling yourself, “If I get a new job, everything’ll be smooth sailing,” or “If I get rid of everything I’m scared of, there won’t be anything to be afraid of anymore.” Your depression and fears reside inside you, so wherever you are, they will be too, projected onto the outside world. Of course, this doesn’t mean that you shouldn’t strive to improve your life. First of all, though, you need to direct your efforts inwards. CONCLUSION: ACTING AGAINST WHAT FEELS LIKE COMMON SENSE Now, when I look at these mistakes and remember making them myself, I can see the one thing that unites them. The reason we make them is that when depression or panic pounces on us, we start to think and act in the way our instincts and gut feelings tell to us. “Be afraid, run away, resist, danger awaits you everywhere, you’re trapped,” they whisper. Tuning in to this during a bout of depression aggravates our situation. This is because our mind, emotions, and instincts are strongly conditioned by depression, so listening to them is like listening to the voice of a malicious, invisible demon intent on leading you to ruin. To free yourself from depression once and for all you have to drop all your notions of common sense; abandoning your sense of reason, you must act against them. Don’t resist your depression, accept your fears and allow them to simply pass; don’t get caught up in them and don’t believe them; don’t compare your current situation to how it was before—all things that feel illogical when you’re in a state of terror or intense depression. What I’m advising may seem to be the polar opposite of what your gut encourages you to do. But it’s precisely because people continue to give credence to and obey these feelings that depression is such a widespread complaint. You need to act somewhat paradoxically to get rid of it. My own experience has convinced me of this. The understanding I reached allowed me to come through my difficult situation and continues to help me cope with challenges I encounter on my journey. Man breathing deeply image via Shutterstock Rockland County Depression and Bipolar Support Alliance 12 Treating Depression to Prevent Suicide AUG. 24, 2014 Inside Photo Credit Caroline Gamon To the Editor: What Dr. Jamison clarifies by using her own experience with suicidal depression is the need for combined treatment with psychotherapy and medications like lithium and electroconvulsive therapy if medications fail. This is a valuable and necessary addition to understanding that severe mental illness can be treated. illness generally is isolation. The mind is powerful, fragile and all too alone. We must ground ourselves in relationship to one another. Otherwise, our mind thinks that it knows what reality is, and it never knows the whole story. It can’t. None of us can contain reality on our own; we have only our perspectives and perceptions. Her example as someone who has been helped to live a productive life because of combined treatment should serve to inform all of us — psychiatrists, mental health professionals and ordinary citizens — of the existence of effective treatment for severe, suicidal depression. Thus, relationship is critical, and empathy is not optional or in any way secondary to professional competence. RAVI CHANDRA San Francisco, Aug. 16, 2014 The writer is a psychiatrist. To the Editor: Re “To Know Suicide” (Op-Ed, Aug. 16): As a psychiatrist trained in psychoanalysis, I find that my clinical experience meshes with Kay Redfield Jamison’s article. In the aftermath of the public’s response to Robin Williams’s suicide, her observations about the importance of differentiating types of depression, particularly bipolar from other types of depressive disorders, is particularly important. Furthermore, her effort to describe the painful and inexorable feeling state that a person suffering from bipolar depression experiences comes as close as is possible to explaining why a person with an otherwise successful life might be driven to suicide. HENRY J. FRIEDMAN Boston, Aug. 16, 2014 The writer is an associate clinical professor of psychiatry at Harvard Medical School. To the Editor: Kay Redfield Jamison provides insight into suicide and the struggles of mental illness, valuable after Robin Williams’s suicide. I applaud her emphasis on competent care, but I take issue with her drawing a distinction between competence and compassion. You can’t have one without the other, and both are trainable and must be cultivated at all levels of health care and society if we are to prevent suicide and ease the burdens of mental illness. One of the chief problems of a likelihood of suicide and mental Regarding Kay Redfield Jamison’s commentary on suicide: What can we really do to help? As a journalist and a survivor of suicide attempts who has interviewed dozens of “out” survivors, I would like to offer a few ideas rooted in social justice, a concept missing from the conversation. Stop discriminating against people who have been suicidal. It takes guts to open up about this, and yet some people are fired for it or are expelled from universities. It’s illegal, but the fear is enough to keep a suicidal person silent until it’s too late. Educate. Just two states, Kentucky and Washington, require that mental health continued on page 14 Rockland County Depression and Bipolar Support Alliance 13 Continued from page 13 professionals be trained in suicide prevention. Get to know the emerging movement of suicide-attempt survivors, who this year got the country’s top suicide prevention group, the American Association of Suicidology, to create a division for people who have been suicidal; released the federally funded report “The Way Forward” with demands for change; and put us front and center in a field that acknowledges that it has long neglected us. founder of Attemptsurvivors.com. Finally, take a good look at us at Livethroughthis.org, and try to tell yourself that people who have been suicidal are really some nameless “them.” A version of this letter appears in print on August 25, 2014, on page A18 of the New York edition with the headline: Treating Depression to Prevent Suicide. Order Reprints|Today's Paper|Subscribe CARA ANNA New York, Aug. 16, 2014 The writer is a member of the Attempt Survivor Task Force of the National Action Alliance for Suicide Prevention and the Up Close and Personal…continued from page 1 Q5: That wasn’t very nice. Were you the reason for the drugs and alcohol? A: Absolutely. You had to self-medicate or literally bust. Q6: But Igave up the stuff up for 15 years and seemed to be okay. Graduating with honors, bodybuilding, marriage, and all that comes with career building. Where were you? A: Waiting. I knew all that over compensation would lead you back to me. I knew you would crash and burn, and return to selfmedicating. Q7: Ouch. Was I in denial of you and your power? A: Oh, so in denial. I knew you could give up the substances, so I made sure you were miserable when you were sober. Q8: I see that now. But did you have to put me in that hole, that awful dark pit of hopelessness? A: That’s how it works. Remember…I kill. Q9: What pisses you off? A: Awareness…treatment…medication…DBSA…AA…and that damn internal spirit to rise above me. Q10: Will I ever be free of you? I doubt it. But I’m feeling pretty weak these days…but…I’ll be ready if you drop the ball. Not a chance…I’m sticking to my wellness program…all the things that piss you off Rockland County Depression and Bipolar Support Alliance 14 Ask the Doc Q: A relative of mine, recently diagnosed with bipolar disorder, has been displaying disorganized thinking, exercising poor judgment without knowing it, overstepping boundaries, with hyper-religiosity. She does not see these things, but her loved ones do. I want to let her know our observations so she can get the right help. How do I gently tell her this without upsetting or alienating her? A: These conversations can certainly be challenging. Despite what you see on television, dramatic Greg Simon, MD, MPH confrontations or “interventions” are often not at all helpful. It’s usually best to start with a calm and nonconfrontational one-on-one conversation. Some general advice about how to make those conversations more effective: Pick the right time. You may feel the most urgent need to have this conversation right after something upsetting has happened, like an argument or confrontation. But those can be the most difficult times for people to feel safe and understood. Try to pick a calmer time when things are going relatively well— when you are feeling more connected or in agreement about things. It’s natural to want to fix the roof when it’s raining, but it’s safer and easier when the sun is out. Describe, rather than label. Try to express your concern about specific things you notice without using diagnostic labels (like “manic”) or inflammatory terms (like “out of control”). Instead, try using “I” statements to describe what you see: “I notice that you’re talking faster than usual” OR “I notice that you’re only sleeping a few hours at night.” If you use any labels, be sure to allow that you might be wrong: “Last time you were talking fast like this, it turned out that you were getting manic. Could that be happening again?” Find common ground. Is something happening that both of you can identify as a problem? You may be most concerned about your relative’s over-spending, but she may care most about not being able to sleep. Try to understand what she is most bothered by, even if it is not your highest priority. Avoid threats and “I told you so.” If you are upset or frightened, it’s natural to want to say things like “If you don’t get help, then (fill in terrible disaster of your choice)!” The only thing less helpful is to say, “Didn’t I tell you this would happen if you didn’t get help?” If your relative is not seeing some problems that you are seeing, then fear or humiliation will not make it easier for her to see them. Offer to help. Instead of saying, “You’d better get in to see your doctor right away!” it’s usually more helpful to say something like “How could I help you to check in with your doctor?” Offering and asking often works better than telling. Greg Simon, MD, MPH, is a psychiatrist and researcher at Group Health Cooperative at the Center for Health Studies in Seattle. His research focuses on improving the quality and availability of mental health services for people living with mood disorders, and he has a specific interest in activating consumers to expect and demand more effective mental health care. Reprinted from DBSA National Website Rockland County Depression and Bipolar Support Alliance 15 Writings From Our Members Continued Easy It would be so easy But I’m well now Still it would be so easy It’s logical There is no logic Ironic I still think about it often But I’m well now I think about it About why I think about it It really would be easy It feels right I’m well now I don’t feel anything Sad And that’s why It would be so easy Sad Not depressed I can think I’m well I can think Well It would be so easy Thaw Winter vines carve dark Red arcs through crystal air and Hover there on snow. My fog breath whines at You in icy woods but still My heart unfreezes. Barbara Marsel When I wrote this I didn’t realize how easy. But it wasn’t easy, me, it was thoughtless, as in devoid of thought. I wasn’t thinking, I’d stopped thinking. I just moved; no senses, no feelings, no mw. I didn’t know that the disease could strip me so bare. I didn’t think I would succumb again. I’d been through the rigors, I thought, enough times; inpatient, outpatient, DBT, CBT. ACT, therapy, meds, support groups, friends. I’d learned; to control, to let go, to ask, to tell. I was well. I have learned. I don’t know if it is due to the critical impact of the last attempt, or because it was the right time, or, or, or…it doesn’t matter. There is a shift in my thinking, a movement in my being. I am here, I am grateful, I am supposed to be here, amongst people, friends, to use my body, my brain to whatever capacity is allowed me, to have an impact upon my world, however large or small. To not squander my days in despondency and laziness, to take one step at a time, to forgive myself and not give cause for others to forgive me. The most precious lesson of all..It is so easy. When the Dis Order has crept in and I am not paying attention, I can get lost. It may just be so again one day. But, without pressure, rather with diligence, I move through each day aware, unafraid and I work to maintain the order. Maybe that is my purpose, simply to survive from day to day and that is fine. I just choose to do it in the very best way I can. Eileen Warmbrand Rockland County Depression and Bipolar Support Alliance 16