* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Circulatory ppt
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
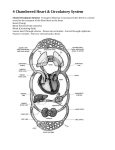
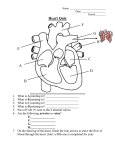
Circulatory and Respiratory System Circulatory System Heart Anatomy Heart Location Fun Fact • If all arteries, veins, and capillaries of the human circulatory system were laid end to end, the total length would be 60,000 miles. That's nearly 2 ½ times around the Earth! • Your body has about 5.6 liters and circulates through the body 3 times/min. In one day, the blood travels a total of 12,000 miles- that's four times the distance across the U.S. from coast to coast. Circulatory System • Structures: o Heart, Blood vessels, blood • Functions: o Brings oxygen, nutrients and hormones to cells o Fights infection o Regulates body temperature. Heart • Made of cardiac muscle • Beats on average 6585 beats per minute • Pumps to circulate blood throughout the body Take your Pulse Locating Pulse Points :The pulse is actually the arteries expanding in rhythm with the contraction of the heart. The pulse can be taken at a variety of locations on the body. There are seven common pulse points • Radial pulse (thumb side of the wrist) • Brachial pulse (inner elbow) • Carotid pulse (neck) • Popliteal pulse (behind the knee) • Posterior tibial pulse (behind the ankle bone) • Dorsalis pedis pulse (top of the foot) Blood Vessels: • • • Carry blood to cells Lined with smooth muscle tissue and epithelial cells Simplest and most common route: Heart arteries arterioles capillaries venules veins Arteries (carries blood away from heart) • Carry oxygenated blood from the heart to the rest of the body. • Strong, thick, elastic walls adapted for high pressure • Arteries become smaller as they divide and give rise to arterioles. Arteries • Arteries are capable of vasoconstriction as directed by the sympathetic impulses; when impulses are inhibited, vasodilation results; used to regulate blood flow and blood pressure. • Walls of arterioles get thinner as they approach the capillaries. Fig 13.17 12 Aspirin Aneurysm • Aneurysm—weak point in an artery or the heart wall o Forms a thin-walled, bulging sac that pulsates with each heartbeat and may rupture o Dissecting aneurysm: blood accumulates between the tunics of the artery and separates them o Most common sites: abdominal aorta, renal arteries, and arterial circle at base of brain 20-14 Aneurysm • Aneurysm (cont.) o Can cause pain by putting pressure on other structures o Can rupture causing hemorrhage o Result from congenital weakness of the blood vessels or result of trauma or bacterial infections such as syphilis • Most common cause is atherosclerosis and hypertension 20-15 Arterial stent Capillaries • Branch off of the Arterioles • The smallest of the blood vessels o some have diameters as small as 1 red blood cell • Takes blood to cells where nutrients/gases exchanged Fig 13.19 18 Capillaries o Capillary permeability varies from one tissue to the next (generally with more permeability in the liver, intestines, and certain glands, and less in muscle) o Areas with a great deal of metabolic activity (leg muscles, for example) have higher densities of capillaries. o Precapillary sphincters can regulate the amount of blood entering a capillary bed and are controlled by oxygen concentration in the area; if blood is needed elsewhere in the body, the capillary beds in less important areas are shut down. Fig 13.18 20 Capillary Beds Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Precapillary sphincters Thoroughfare channel Metarteriole Capillaries Arteriole Venule Figure 20.3a (a) Sphincters open When sphincters are open, the capillaries are well perfused and engage in exchanges with the tissue 20-21 fluid Capillary Beds Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Figure 20.3b Arteriole (b) Sphincters closed Venule • When the sphincters are closed, little to no blood flow occurs (skeletal muscles at rest) • ¾ of body’s capillaries are shut down at a given20-22 time Exchange in Capillaries • Hydrostatic pressure drives the passage of fluids and very small molecules out of the capillary at the arteriole end by diffusion. • At the venule end, osmosis, due to the osmotic pressure of the blood, causes much of the tissue fluid to return to the bloodstream. • Lymphatic vessels collect excess tissue fluid and return it to circulation. Veins (and venules) • Venules leading from capillaries merge to form veins that return blood (deoxygenated) to the heart. Veins • Veins have the same three layers as arteries have, except that the muscle layer is thinner, and have a flap-like valve inside to prevent backflow of blood. • The lumen of a vein is larger than an artery • Veins do not carry high-pressure blood. • Veins also function as blood reservoirs. • Greater capacity for blood containment than arteries • Thinner walls, flaccid, less muscular and elastic tissue • Collapse when empty, expand easily • Have steady blood flow • Merge to form larger veins • Subjected to relatively low blood pressure o Remains 10 mm Hg with little fluctuation Veins Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Distribution of Blood Pulmonary circuit 18% Veins 54% Heart 12% Systemic circuit 70% Arteries 11% Capillaries 5% Figure 20.8 20-26 Blood Flow Comparison Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. At rest Total cardiac output 5 L/min Moderate exercise Total cardiac output 17.5 L/min Other Coronary 350 mL/min 200 mL/min (7.0%) (4.0%) Cutaneous 300 mL/min (6.0%) Other Coronary 400 mL/min 750 mL/min (2.3%) Cutaneous (4.3%) 1,900 mL/min (10.9%) Muscular 1,000 mL/min (20.0%) Cerebral 700 mL/min (14.0%) Renal 1,100 mL/min (22.0%) Cerebral 750 mL/min (4.3%) Digestive 1,350 mL/min (27.0%) • During exercise Renal 600 mL/min (3.4%) Digestive 600 mL/min (3.4%) Muscular 12,500 mL/min (71.4%) Figure 20.15 o Increased perfusion of lungs, myocardium, and skeletal muscles o Decreased perfusion of kidneys and digestive tract 20-27 Fig 13.23 28 The Skeletal Muscle Pump Muscles help pump blood back to heart through the veins To heart Valve open Venous blood Valve closed (a) Contracted skeletal muscles (b) Relaxed skeletal muscles Figure 20.19a,b Copyright © The McGraw-Hill Companies, Inc. Permissio required for reproduction or display. 20-29 Comparing arteries and veins Fig 13.20 34 Varicose veins Varicose Veins • Blood pools in the lower legs in people who stand for long periods stretching the veins o Cusps of the valves pull apart in enlarged superficial veins further weakening vessels o Blood backflows and further distends the vessels, their walls grow weak and develop into varicose veins • Hereditary weakness, obesity, and pregnancy also promote problems • Hemorrhoids are varicose veins of the anal canal Treatment for varicose/spider veins • Sclerotherapy. doctor injects the veins with a solution that scars and closes those veins, causing the blood to reroute through healthier veins. • Vein ligation/vein striping • Laser surgery. Laser surgery works by sending strong bursts of light into the vein that make the vein slowly fade and disappear. No incisions or needles are used. The treatment is often less effective than sclerotherapy. Fig 13.1 39 The Heart • The human heart has four chambers oLeft and right atrium (above) oLeft and right Ventricles (make a V) • The right side of the heart pumps deoxygenated blood to the lungs • The left side of the heart pumps oxygenated blood to the body Left Atrium Right Atrium Right Ventricle Left Ventricle Fig 13.4 43 Upper body Blood Flow in the Heart Cool Facts about the circulatory system Valves of the Heart Operation of the Heart Valves Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Atrium Atrioventricular valve Ventricle Atrioventricular valves open Atrioventricular valves closed (a) Figure 19.19 Aorta Pulmonary artery Semilunar valve Semilunar valves open (b) Semilunar valves closed 19-49 Fig 13.6 50 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. The Valves Left AV (bicuspid) valve Right AV (tricuspid) valve Fibrous skeleton Openings to coronary arteries Aortic valve Pulmonary valve (a) Figure 19.8a 19-51 The Valves: Endoscopic View Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. (b) © Manfred Kage/Peter Arnold, Inc. Figure 19.8b 19-52 Heart Sounds • Heart sounds are due to vibrations in heart tissues as the valves close. • Heart sounds can be described as a "lubb-dupp" sound. o The first sound (lubb) occurs as ventricles contract and AV valves are closing. o The second sound (dupp) occurs as ventricles relax and aortic and pulmonary valves are closing. • An abnormal heart sound is called a murmur which is due to valve damage. 53 Heart Murmurs • Aortic Valve Replacement Fig 13.8 55 Coronary Arteries Intraventricular Septum 1) The right atrium receives deoxygenated blood from the body through the superior and inferior vena cava. 2) The right atrium pumps blood through the tricuspid (AV) valve and into the right ventricle 3) Right Ventricle Contracts and pushes blood through pulmonary valve towards lungs 4) Blood is pushed through the pulmonary arteries to the lungs to receive oxygen 5) Oxygenated blood returns to the left atrium from the lungs through the pulmonary veins 6) Blood passes through the bicuspid (mitral) valve into the left ventricle. 7) Contraction of Left ventricle pumps blood through aortic valve to the aorta 8)Blood travels through aorta and then to all regions of the body where it feeds cells with oxygen picked up from the lungs and nutrients from the digestive tract. Blood Pressure • A measure of the force exerted by the blood on the wall of the arteries. (using sphygmomanometer) o An example is 120/80 (systolic pressure/diastolic pressure. • Systolic pressure is the result of the contraction of the ventricles (normal 110140) • Diastolic pressure is during the ventricle relaxation (normal 70-90) o Pressure decreases as distance from the left ventricle increases. Blood Pressure • Hypertension—high blood pressure o Chronic is resting BP > 140/90 o Consequences • Can weaken small arteries and cause aneurysms • atherosclerosis • Hypotension—chronic low resting BP o Caused by blood loss, dehydration, anemia 20-68 Blood Pressure • BP rises with age o Arteries less distensible and absorb less systolic force • BP determined by cardiac output, blood volume, and peripheral resistance o Resistance hinges on blood viscosity, vessel length, and vessel radius 20-69 Cardiac output • Cardiac output = stroke volume x heart rate. • Stroke volume is the amount of blood discharged from the ventricles with a contraction (about 70 mL). • Heart rate is the beats per minute (average is 72 beats/min). Peripheral Resistance • Peripheral resistance—the opposition to flow that blood encounters in vessels away from the heart • Resistance hinges on three variables 1. Blood viscosity (“thickness”) • RBC count and albumin concentration elevate viscosity the most • Decreased viscosity with anemia • Increased viscosity with dehydration 20-71 Peripheral Resistance • Resistance hinges on three variables (cont.) 2. Vessel length • The farther liquid travels through a tube, the more cumulative friction it encounters • Pressure and flow decline with distance o Vessel radius: most powerful influence over flow • Vasomotion—change in vessel radius oVasoconstriction: increases resistance=increases bp oVasodilation: by relaxation of the smooth muscle, decreases resistance=decreased pressure 20-72 Fig 13.24 73 Peripheral Resistance Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. (a) (b) Figure 20.11 20-74 Blood Volume • Blood pressure is normally directly proportional to the volume of blood within the cardiovascular system. • Blood volume varies with age, body size, and gender. Fig 13.25 76 Control of Blood Pressure 1.Blood pressure is determined by cardiac output times peripheral resistance; BP = CO x PR 1.The body maintains normal blood pressure by adjusting cardiac output and peripheral resistance. 77 Control of Blood Pressure • Frank-Starling law of the heart is the relationship between fiber length and force of contraction. a. As blood enters the heart, the walls are stretched, giving a stronger contraction. b. The stronger contraction increases stroke volume and cardiac output. 78 Control of Blood Pressure • Baroreceptors sense change in BP a. The volume of blood that enters the right atrium is normally equal to the volume leaving the left ventricle. b. If arterial pressure increases, the cardiac center of the medulla oblongata sends parasympathetic impulses to slow heart rate (cardioinhibitor reflex). c. If arterial pressure drops, the medulla oblongata sends sympathetic impulses to increase heart rate to adjust blood pressure (cardioaccelerator reflex). 79 Baroreceptors 80 Fig 13.26 81 Control of Blood Pressure • Other factors, such as emotional upset, exercise, and a rise in temperature can result in increased cardiac output and increased blood pressure. • Peripheral resistance also controls blood pressure a. Sympathetic nerves change the diameter of arterioles in response to blood pressure changes. b. Vasodilation will decrease PR and BP. c. Vasoconstriction will increase PR and BP. 82 Control of Blood Pressure • The vasomotor center of the medulla oblongata can adjust the sympathetic impulses to smooth muscles in arteriole walls, adjusting blood pressure. • Certain chemicals can also affect peripheral resistance by affecting precapillary sphincters and smooth muscle of arteriole walls. a. Increased CO2, decreased O2, and decreased pH cause vasodilation into tissues with high metabolic needs. b. Epinephrine and norepinephrine cause vasoconstriction. 83 Hormonal Control of Blood Pressure • Hormones influence blood pressure o Some through their vasoactive effects o Some by regulating water balance • Angiotensin II—potent vasoconstrictor o Raises blood pressure o Promotes Na+ and water retention by kidneys o Increases blood volume and pressure • Atrial natriuretic peptide—increases urinary sodium excretion o Reduces blood volume and promotes vasodilation o Lowers blood pressure 20-84 Hormonal Control of Blood Pressure • ADH promotes water retention and raises BP o Pathologically high concentrations; also a vasoconstrictor • Epinephrine and norepinephrine effects o Most blood vessels • Bind to -adrenergic receptors—vasoconstriction o Skeletal and cardiac muscle blood vessels • Bind to -adrenergic receptors—vasodilation 20-85 Disorders of the Circulatory System: Coronary artery disease – Atherosclerosis • Plaque buildup blocks arteries, reducing, or even stopping blood flow • Plaques can break off, causing heart attack or stroke Coronary Artery disease Cause: Damaged arteries are ‘invaded’ by bad LDL cholesterol. White blood cells try to digest the LDL. Ultimately, a jumble of cholesterol and whilte blood cells is accumulated. Risk Factors: Smoking, high blood pressure, high LDL cholesterol, diabetes Treatments • Lifestyle changes: Follow healthy diet, maintain healthy weight, exercise, quit smoking, manage stress • Medicine: lowers cholesterol, helps prevent platelets from sticking and clotting (aspirin), helps harden plaque so lowers chance of breaking off • Surgeries: o Angioplasty (Coronary Stent) o Coronary artery bypass o Carotoid endartectomy Coronary Bipass Surgery The Cardiac Conduction System 1 SA node fires. Right atrium 2 Excitation spreads through atrial myocardium. 2 1 Sinoatrial node (pacemaker) Left atrium 2 Atrioventricular node Atrioventricular bundle Purkinje fibers 3 Bundle branches 4 5 3 AV node fires. 4 Excitation spreads down AV bundle. 5 Purkinje fibers distribute excitation through ventricular myocardium. Purkinje fibers Figure 19.12 19-92 Cardiac Conduction System 1.Specialized cardiac muscle tissue conducts impulses throughout the myocardium and comprises the cardiac conduction system. 2.A self-exciting mass of specialized cardiac muscle called the sinoatrial node (SA node or pacemaker), located on the posterior right atrium, generates the impulses for the heartbeat. 93 Fig 13.11 94 Pacemaker Physiology • SA node does not have a stable resting membrane potential o Starts at −60 mV and drifts upward from a slow inflow of Na+ • When it reaches threshold of −40 mV, voltage-gated fast Ca2+ and Na+ channels open o Faster depolarization occurs peaking at 0 mV o K+ channels then open and K+ leaves the cell • Causing repolarization • Once K+ channels close, pacemaker potential starts over 19-95 Pacemaker Physiology • Each depolarization of the SA node sets off one heartbeat o At rest, fires every 0.8 second or 75 bpm • SA node is the system’s pacemaker 19-96 Pacemaker Physiology Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Membrane potential (mV) +10 0 –10 Fast K+ outflow Fast Ca2+–Na+ inflow –20 Action potential Threshold –30 –40 Pacemaker potential –50 –60 Slow Na+ inflow –70 0 .4 .8 1.2 1.6 Time (sec) Figure 19.13 19-97 Cardiac Conduction System 3.Impulses spread next to the atrial syncytium, it contracts, and impulses travel to the junctional fibers leading to the atrioventricular node (AV node) located in the septum. a. Junctional fibers are small, allowing the atria to contract before the impulse spreads rapidly over the ventricles. b. The delay through these fibers allows both atria to contract together. 98 Cardiac Conduction System 4.From the AV node, the impulse passes to branches of the AV bundle and travel down the interventricular septum. 5.Purkinje fibers branch off the bundle branches and lead into the ventricular wall and papillary muscles. 6.These fibers stimulate contraction of the papillary muscles at the same time as the ventricles contract in a twisting, upward motion. 99 Fig 13.11 10 0 Fig 13.12 10 1 Fig 13.13 10 2 Electrocardiogram (ECG) Electrocardiogram (ECG) Electrocardiogram 1.An electrocardiogram (ECG) is a recording of the electrical changes that occur during a cardiac cycle. 2.The first wave, the P wave, corresponds to the depolarization of the atria which leads to the contraction of the atria. 3.The QRS complex corresponds to the depolarization of ventricles that leads to contraction of the ventricles and hides the repolarization of atria. 10 6 Electrocardiogram 4.The T waves ends the ECG pattern and corresponds to ventricular repolarization and relaxation. 5.The intervals between the waves as well as the size of the waves give information about the heart’s ability to conduct impulses. 10 8 Fig 13.14 10 9 Fig 13.15 11 0 Electrocardiogram 1. The amount of blood pumped at any one time must adjust to the current needs of the body (more is needed during strenuous exercise). 2. The SA node, AV node, and the myocardium are innervated by branches of the sympathetic and parasympathetic divisions of the autonomic nervous system. a. Sympathetic impulses increase the speed and strength of heart contractions. b. Heart rate is decreased by parasympathetic impulses. 11 1 Regulation of the cardiac cycle 3.The cardiac control center of the medulla oblongata maintains a balance between the sympathetic and parasympathetic divisions of the nervous system in response to messages from baroreceptors which detect changes in blood pressure. 4.Impulses from the cerebrum or hypothalamus may also influence heart rate through emotions. 5.Increased body temperature will increase heart rate. 11 2 Regulation of the cardiac cycle 6.Hyperkalemia (excess K+) will decrease rate and force of contraction; hypokalemia may cause life-threatening arrhythmias. 7.Hypercalcemia (excess Ca2+) increases heart action while hypocalcemia depresses heart action. 8.Tachycardia – more that 100 beats/min 9.Bradycardia – less than 60 beats/min 11 3 Fig 13.16 11 4 Disorders of the Circulatory System • Arrhythmia= Irregular / skipped heart beat Cause: The heart uses electrical signals created in the SA node in the right atria, to begin a heartbeat. The conduction of these signals, or irregular firing of the SA node, can cause arrhythmias. Atrial arrhythmias are less dangerous than ventricular arrhythmias. Risk Factors: Generally random, but factors are stimulants (such as caffeine), fevers, stress, or genetic disorders. AFIB Oblation Disorders of the Circulatory System • High blood pressure - Hypertension Diastolic pressure over 90 Why it is dangerous: Excessive pressure can cause the arteries to thicken, and blood vessels to weaken and rupture. This can lead to heart failure, stroke, kidney failure, loss of sight when vessels in eyes burst. Risk Factors: Genetics, overweight, limited physical activity, smoking, alcohol consumption, certain medications Virtual Cardiology Lab Disorders of the Circulatory System • Heart Attack– Myocardial Infarction (MI) = Death of cardiac muscle cells Cause: Plaque dislodges, blocking an artery to the heart muscle. Cardiac muscle cells are starved for oxygen and die. After, scar tissue forms where cells died, reducing function of heart. Severity of a heart attack depends on size and area supplied by the artery. Risk Factors: Smoking, high blood pressure, high LDL cholesterol, diabetes Bypass surgery Disorders of the Circulatory System • Stroke=Death of cells in the brain. Cause: A blood vessel in the brain is blocked (by dislodged plaque, or bursts, starving the cells of oxygen) A stroke can have many different symptoms, including: numbness, vision changes, speech changes, or confusion. Risk Factors: Smoking, high blood pressure, high LDL cholesterol, diabetes