* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chemotherapy Basics
Citric acid cycle wikipedia , lookup
Peptide synthesis wikipedia , lookup
Fatty acid synthesis wikipedia , lookup
Biochemistry wikipedia , lookup
Enzyme inhibitor wikipedia , lookup
Biosynthesis wikipedia , lookup
Artificial gene synthesis wikipedia , lookup
Amino acid synthesis wikipedia , lookup
Butyric acid wikipedia , lookup
15-Hydroxyeicosatetraenoic acid wikipedia , lookup
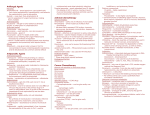
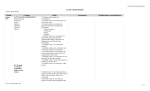
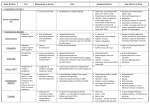
Chemotherapy Basics Sites of Exclusion: CSF Ocular fluid (duh) Synovial fluid Pleural fluid cysts Necrotic tissue Sites of Concentration: Liver & bile Kidney & urine Bone Fat RBCs Skin Antibiotics Cell wall Synthesis Inhibitors Penicillins: Penicillin G (benzylpenicillin) -- against Gm + Benzathine penicillin G -- depo preparation Nafcillin -- -lactamase resistance Oxacillin -- -lactamase resistance Cloxacillin -- -lactamase resistance Carbenicillin -- Proteus & Pseudomonas Ticarcillin -- Proteus & Pseudomonas Piperacillin -- Pseudomonas & Klebsiella Ampicillin -- increased Gm - activity Amoxacillin -- increased Gm - activity * Penicillins also activate murein hydrolases Cephalosporins: 1st Gen. = Cephalothin Cephalexin -- can be given orally Cefadroxil -- can be given orally 2nd Gen. = Cefoxitin Cefaclor -- can be given orally 3rd Gen. = Ceftriaxone Ceftazidime Cefixime -- can be given orally Moxalactam Monobactams: Aztreonam -- not inactivated by -lactamases; mostly used for Gm - organisms, not effective vs. Gm + Carbapenems: Imipenem -- given IV; broad spectrum Non--lactams: Vancomycin -- oral for GI superinfections, IV for most other uses; does not cross the blood-brain barrier (BBB) Bacitracin -- Gm + only; used as a topical antibiotic because of its nephrotoxicity -Lactamase inhibitors: Sulbactam Clavulanic acid Inhibitors of Protein Synthesis Aminoglycosides: -- bind irreversibly to the 30S subunit of bacterial ribosomes; particularly useful vs. Gm Streptomycin – given IM, not orally Kanamycin -- mainly reserved for topical applications Neomycin -- mainly reserved for topical applications Gentamicin Tobramycin -- slightly less nephrotoxic than gentamicin Amikacin Netilmicin * since the aminoglycosides are poorly absorbed orally, they are usually given IM or IV * Ototoxicity, nephrotoxicity, and neuromuscular blockade (very rare) are among their adverse effects Tetracyclines: -- broad spectrum; bind reversibly to the 30S subunit of bacterial ribosomes (bacteriostatic) Chlortetracycline -- <30% absorbed orally Oxytetracycline -- 60-80% absorbed orally Tetracycline -- 60-80% absorbed orally Doxycycline -- complete oral absorption Minocycline -- complete oral absorption * all are potent chelators of metal cations * do not cross the BBB in significant concentrations * DO cross the placenta...contraindicated in pregnancy * Frequently used for: Mycoplasma, chlamydia, rickettsiae and Lyme disease Macrolides: Erythromycin -- bind reversibly to the 50S subunit; primarily cleared in the bile; Erythromycin esters * potent inhibitor of certain P-450 enzymes * frequently used for: Mycoplasma, chlamydia, corynebacteria, and legionnaire’s disease Others: Chloramphenicol -- broad spectrum; will get into the CNS; entirely excreted in urine; binds reversibly to the 50S subunit; can (rarely) induce aplastic anemia which is usually irreversible; use is limited to anaerobic and mixed CNS infections, sensitive Salmonella and H. flu Spectinomycin -- simialr to aminoglycosides; only given IM Clindamycin -- given orally or IV; inhibits the 50S subunit; resistance is chromosomal, and C. difficile is one of the most common ones that has developed resistance Drugs that alter cell membrane function: Polymixins Nystatin Gramicidin Amphotericin B Inhibitors of Nucleic Acid Synthesis Sulfonamides: -- broad spectrum; great for UTIs; will get Into the CNS readily Sulfisoxazole Sulfacytine Sulfamethoxazole Sulfasalazine Silver sulfadiazine Sodium sulfacetamide Co-trimoxazole (sulfamethoxazole+trimethoprim) * Sulfas are similar to p-aminobenzoic acid (PABA); in this way they competitively inhibit the formation of dihydrofolic acid (the enzyme is dihydropteroate synthase) * Trimethoprim is a substrate analogue for dihydrofolate reductase...inhibits formation of folic acid; although it is much more specific for bacterial forms, it does act on human isoforms of the same enzyme -- and those effects can lead to those seen with folate deficiency! * Must remember to hydrate the patient well to avoid crystallization of sulfas in the urinary tract DNA Gyrase inhibitors: Nalidixic acid -- is a quinolone; used mostly against Gm organisms; excretion is too fast to be an effective agent Ciprofloxacin -- is a fluroquinolone; used for both Gm and Gm + bugs Norfloxacin -- is a fluroquinolone; used for both Gm and Gm + bugs * Fluroquinolones inhibit theophylline clearance; they can also cause abnormal liver function tests and skin rashes. Antimycobacterial Agents First-line drugs: Isoniazid (INH) -- blocks mycolic acid synthesis...key components of their cell wall; hepatotoxicity occurs in fast acetylators Ethambutol -- RBCs concentrate this one...so they can act as a depo source; can cause a reversible(usually) optic neuritis...dose dependent Rifampin -- also effective vs. GM + and Gm - cocci; inhibits bacterial RNA synthesis; potent inducer of P-450s Pyrazinamide -- resistance develops quickly; can cause hyperuricemia and hepatotoxicity Second-line drugs: Para-aminosalicylic acid -- rapidly excreted in urine; it blocks the folate pathway in mycobacteria Ethionamide -- causes intence gastric pain, and may be neurotoxic as well Cycloserine -- inhibits alanine racemase; CNS toxicity and drug-induced psychoses limits its use Antileprosy drugs: Dapsone -- gets into skin better than rifampin; also good against Pneumocystis carinii;frequently causes a hemolytic anemia, and it also induces a methemoglobinemia; GI disturbances and skin rashes are also encountered