* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
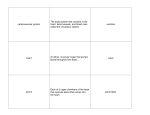
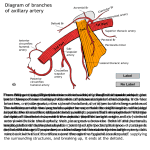
Pamela BL Description Contents Clinical application The axilla(armpit, underarm) is the pyramidal space inferior to the scapulohumeral joint and superior to the axillary fascia at the junction of the arm and thorax. It provides passageway for vessels and nerves to reach the upper limb. The shape and size of the axilla vary depending on the position of the arm. It almost disappears when the arm is fully abducted. The 1. 2. 3. axilla has: An apex A base Four walls Apex of axilla (the entrance from the neck) lies btwn the 1st rib, clavicle and superior edge of subscapularis. The arteries, veins, lymphatics and nerves pass from the neck to the axilla through the cervicoaxillary canal-the superior opening to the axilla, to reach the arm. Base of the axilla is formed by the concave skin, subcutaneous tissue and axillary(deep) fascia extending from the arm to the thoracic wall. Anterior wall of axilla is formed by pectoralis major and pectoralis minor muscles, and pectoral and clavipectoral fascia associated with them. Posterior wall of axilla is formed by scapula and subscapularis on its anterior surface and inferiorly by teres major and latissimus dorsi. Medial wall is formed by the thoracic wall(1st-4th rib and intercostal muscles) and the overlying serratus anterior. Lateral wall of axilla is a narrow bony wall formed by the intertubercular groove of humerus. The 1. 2. 3. 4. 5. 6. axilla contains: Axillary artery and its branches Axillary vein and its tributaries A network of interjoining nerves(brachial plexus) that pass from the neck to the upper limb Several groups of axillary lymph nodes Lymphatic vessels. Proximally these neurovascular structures are ensheathed in a fascial sleeve, axillary sheath. Axillary artery begins at the lateral border of the 1st rib as the continuation of the subclavian artery and ends at the inferior border of the teres major. It passes posterior to the pectoralis minor into the arm and becomes the brachial artery when it passes distal to the inferior border of the teres major. For descriptive purposes, the axillary artery is divided into three parts by the pectoralis minor. First part of the axillary artery-located btwn the lateral border of the 1st rib and the medial border of the pectoralis minor, is enclosed in the axillary sheath and has one branch-the superior thoracic artery. The superior thoracic artery(highest thoracic artery) arise from the first part of axillary artery just inferior to the subclavius. It runs inferomedially posterior to the axillary vein and supplies muscles in the 1st and 2nd intercostal spaces and the serratus anterior. It anastomoses with the intercostal arteries. Second part of the axillary artery lies posterior to pectoralis minor and has two branches, the thoracoacromial and lateral thoracic arteries, which pass medial and lateral to the muscle respectively. Thoracoacromial artery, a short wide trunk, deep to pectoralis minor, pierces the costocoracoid membrane(part of clavipectoral fascia) and then divides into 4 branches-acromial, deltoid, pectoral and clavicular deep to the clavicular head of pectoralis major. The lateral thoracic artery has a variable origin. It usually arises from the second part of the axillary artery, but it may arise from the thoracoacromial, suprascapular or subscapular arteries. It supplies the pectoral muscles, the axillary lymph nodes and the breast. It is an important source of blood to the lateral part of the mammary glands in women. Third part of axillary artery extends from lateral border of pectoralis minor to the inferior border of teres major. It has three branches, the subscapular-the largest branch of the axillary artery, anterior circumflex humeral and posterior circumflex humeral arteries. The subscapular artery, the largest branch of the axillary artery descends along the lateral border of the subscapularis on the posterior axillary wall. It then divided into the circumflex scapular and thoracodorsal arteries and supplies the subscapularis, teres major, serratus anterior and latissimus dorsi muscles. The circumflex scapular artery, the larger branch of the subscapular curves posteriorly around the axillary border of the scapula passing btwn the subscapularis and teres major to supply muscles on the dorsum of the scapula. It participates in anastomoses around the scapula. The thoracodorsal artery continues the general course of the subscapular to the inferior angle of the scapula and supplies adjacent muscles principally latissimus dorsi. It also participates in the arterial anastomoses around the scapula. The circumflex humeral arteries usually arise from the third part of the axillary artery opposite the subscapular artery and pass around the surgical neck of the humerus to anastomose with each other. The smaller anterior circumflex humeral artery passes laterally deep to coracobrachialis and biceps brachii, it gives off an ascending branch that supplies the shoulder. The larger posterior circumflex humeral artery passes through the posterior wall of the axilla via the quadrangular space with the axillary nerve to supply surrounding muscles(deltoid, teres major and minor and long head of triceps). Lies on the medial side of the axillary artery. Formed by the union of the brachial vein and the basilic vein at the inferior border of the teres major. It ends at the lateral border of the 1st rib where it becomes the subclavian vein. The axillary vein receives tributaries that generally correspond to branches of the axillary artery with a few exceptions: The veins corresponding to the branches of the thoracoacromial artery do not merge to enter by a common tributary, some enter independently into the axillary vein but others empty into the cephalic vein which superior to pectoralis minor also enters the axillary vein close to its transition to the subclavian vein. The axillary vein receives directly or indirectly the thoracoepigastric vein(s), which is formed by anastomoses of superficial veins from the inguinal region with tributaries of the axillary vein usually the long thoracic vein-constituting a collateral route that enables venous return in the presence of obstruction of the inferior vena cava. The axillary artery can be palpated in the inferior part of the lateral wall of the axilla. Compression of the 3rd part of axillary artery against the humerus may be necessary when there is profuse bleeding(trauma). If compression is required at a amore proximal site, the axillary artery can be compressed at its origin by exerting downward pressure in the angle btwn the clavicle and attachment of sternocleidomastoid. 2.Arterial anastomoses around the scapula Many arterial anastomoses occur around the scapula. Several vessels join to form networks on the anterior and posterior surfaces of the scapula-he dorsal scapular, suprascapular and subscapular(via the circumflex scapular). Slow occlusion of axillary artery(disease/trauma) often enables sufficient collateral circulation to develop, preventing ischemia. Sudden occlusion usually does not allow sufficient time for a good collateral circulation to develop, resulting into an inadequate supply of blood flow to the arm, forearm and hand. Injury to the axillary vein Because of its large size and exposed position the axillary vein is often injured. When the arm is fully abducted, the axillary vein overlaps the axillary artery anteriorly. Its more dangerous when the wound is in the proximal part of the axillary vein not only because of profuse bleeding but also because of the risk of emboli formation. Are found in the fibro fatty connective tissue of the axilla. They are arranged in five principal groups: 1. Apical 2. Pectoral 3. Subscapular 4. Humeral 5. Central Apical lymph nodes- located at the apex of the axilla along the medial side of the axillary vein and the first part of the axillary artery. Receives lymph from all other groups of the axillary lymph nodes as well as from lymphatics accompanying the proximal cephalic vein. The pectoral(anterior) lymph nodes consists of 3-5 lymph nodes that lie along the medial wall of the axilla, around the lateral thoracic vein and the inferior border of the pectoralis minor. They receive lymph mainly from the anterior thoracic all including the breast. Efferent lymphatic vessels from these nodes pass to the central and apical groups of axillary nodes. The subscapular(posterior) axillary lymph nodes consist of 6-7 lymph nodes that lie along the posterior axillary fold and subscapular blood vessels. Receive lymph from the posterior aspect of the thoracic wall and scapular region. Efferent lymphatic vessels pass from these nodes to the central and apical groups of axillary lymph nodes. The humeral(lateral) axillary lymph nodes consist of 4-6 lymph nodes that lie along the lateral wall of the axilla, medial and posterior to the axillary vein. Receive nearly all the lymph from the upper limb except that carried by lymphatic vessels accompanying the cephalic vein which drains to the central and apical axillary lymph nodes. The central axillary lymph nodes consist of 34 lymph nodes situated deep to the pectoralis minor near the base of the axilla in association with the 2nd part of the axillary artery. Receive lymph from the pectoral, subscapular and humeral lymph nodes. Efferent vessels from these nodes pass to apical lymph nodes. The axillary lymph nodes may enlarge(lymphadenopathy) and become tender following infections of the upper limb. Infections in the pectoral region and breast, and the superior part of the abdomen can also produce enlargement of axillary lymph nodes. In carcinoma(cancer) involving the apical lymph nodes, the lymph nodes often adhere to the axillary vein which may necessitate excision of part of this vessel. Enlargement of apical lymph nodes may obstruct the cephalic vein superior to the pectoralis minor. Excision and pathologic analysis of axillary lymph nodes is often necessary for staging and treatment of malignancy e.g. breast cancer. During surgery care is taken not to injure the long thoracic nerve, which is identified and maintained against the thoracic wall. Injury to this nerve causes a winged scapula. Injury to the thoracodorsal nerve results into weakened medial rotation and adduction of the arm, but no deformity forms. The arm extends from the shoulder to the elbow. Two types of movements occur btwn the arm and forearm at the elbow joint: flexionextension, and pronation-supination. The muscles performing these movements are divided into anterior and posterior groups. Three flexors(biceps brachii, brachialis and coracobrachialis) are in the anterior compartment. They are supplied by musculocutaneous nerve. One extensor(triceps brachii) is in the posterior compartment, supplied by the radial nerve. The anconeus at the posterior aspect of the elbow is essentially a distally placed continuation of the triceps brachii. Biceps brachii, located in the anterior compartment of the arm. Has two heads and its two muscle bellies unite just distal to the middle of the arm. When the elbow is extended, the biceps brachii is a simple flexor of the forearm. When the elbow is flexed, and more power is needed against resistance, the biceps is the primary(most powerful) supinator of the forearm. The biceps barely operates during flexion of the prone forearm. The rounded tendon of the longhead of biceps brachii crosses the head of the humerus within the cavity of the glenohumeral joint. The tendon surrounded by synovial membrane, descends in the intertubercular groove of the humerus. A broad band, the transverse humeral ligament passes from the lesser to the greater tubercle of the humerus and converts the intertubercular groove into a canal. The ligament holds the tendon of the long head of biceps brachii in the groove. Distally, the tendon attaches to the tuberosity of the radius. The biceps brachii continues distally as the bicipital aponeurosis, a triangular membranous band that runs from the biceps tendon across the cubital fossa and merges with the antebrachial(deep) fascia covering the flexor muscles in the medial side of the forearm. Approximately 10% of people have a 3rd head to the biceps arising at the superomedial part of the brachialis(with which it is blended). In most, the 3rd head lies posterior to the brachial artery. To test the biceps, the elbow joint is flexed against resistance when the forearm is supinated. If acting normally, the muscle forms a prominent bulge on the anterior aspect of the arm which is easily palpated. Brachialis is a flattened fusiform muscle that lies posterior(deep) to the biceps brachii. The brachialis is the main flexor of the forearm. It flexes the forearm in all positions and during slow and quick movements. Because of its many functions, it is regarded as the workhorse of the elbow flexors. Coracobrachialis is an elongated muscle in the superomedial part of the arm. It is a useful a landmark as the musculocutaneous nerve pierces it, and the distal part of its attachment indicates the location of the nutrient foramen of the humerus. Biceps tendinitis, inflammation of the tendon usually from repetitive microtrauma. Common in sports involving throwing(baseball, cricket). A tight, narrow and/or rough intertubercular groove may irritate and inflame the tendon producing tenderness and crepitus(crackling sound). Triceps brachii, a fusiform muscle locates in the posterior compartment of the arm. It has three heads: long, lateral and medial. it is the main extensor of the elbow joint. Because its long head crosses the shoulder joint, the triceps helps stabilize the adducted glenohumeral joint by serving as a shunt muscle resisting inferior displacement of the head of the humerus. The triceps also aids in extension and adduction of the arm. To test the triceps, the arm is abducted 90 degrees and then the flexed forearm is extended against resistance provided by the examiner. If acting normally the triceps can be seen and palpated. Is an axillary space in the arm of clinical importance. In the quadrangular space, the axillary nerve and posterior circumflex humeral artery can be compresse or damaged due to space occupying lesion or trauma disrupting its normal anatomy. Symptoms include axillary nerve related weakness of the deltoid muscle(in case of significant mass lesions in the quadrangular space). Boundaries: Bounded superiorly by teres minor Inferiorly: teres major Medially: long head of triceps trachii Laterally: surgical neck of humerus. It transmits the axillary nerve and posterior circumflex humeral artery.