* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download thyroid scintigraphy new 2011
Survey
Document related concepts
Transcript
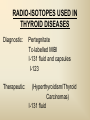
DIAGNOSTIC IMAGING THYROID SCINTIGRAPHY Dr M G Nel(Riana) INDEX • • • • • Anatomy and cell structure Physiology en Hormone production The thyroid’s handling of iodine Radionuclide imaging of the thyroid Thyroid diseases to be imaged hyper- en hypothyroidism thyroid nodules goiters thyroiditis thyroid ca • Radio-active I-131 therapy for Grave’s Thyroid Ca THYROID SCINTIGAPHY: KNOWLEDGE, UNDERSTANDING and APPLICATION (LEVELS 1-3) MUST KNOW the previously acquired knowledge of the anatomy and physiology of the organs OUTCOMES ASSESSMENT CRITERIA ASSESSMENT TASKS Cell and Cell function imaging Name and discuss basic principles of the imagings (Technesium as well as Iodine) Basic Interpretation and usage of the RN procedures The Basic information that you can get from the thyroid imaging Name and discuss the information Basic Interpretation and usage of the RN procedures Normal thyroid scintigraphy Interpretation of the normal images in order to recognise any abnormalities Basic Interpretation and usage of the RN procedures Radio nuclides in use for thyroid imaging Name, discuss and explain the usage of TcO4¯, Tc-99m MIBI, I-123 and I131 Basic Interpretation and usage of the RN procedures Factors influencing the RN uptake and distribution Name, discuss and explain the development of abnormalities Basic Interpretation and usage of the RN procedures Abnormal thyroid images Name, discuss and explain the development of abnormalities Interpretation of procedures and study rapporting Indications for thyroid scintigraphy Name and discuss the indications Apply to patients and their thyroid disease Thyroid abnormalities to be imaged Name and discuss the imaging of the thyroid abnormalities Apply to patients and their thyroid disease Hyperthyroid diseases Explain the abnormality and name the causes Apply to patients and their thyroid disease Hypothyroid diseases Explain the abnormality and name the causes Apply to patients and their thyroid disease THYROID SCINTIGAPHY: KNOWLEDGE, UNDERSTANDING and APPLICATION (LEVELS 1-3) MUST KNOW the previously acquired knowledge of the anatomy and physiology of the organs OUTCOMES ASSESSMENT CRITERIA ASSESSMENT TASKS Basic principles of the Technesium thyroid scintigram Explain the use of this procedure and all the important precautions and preparations Apply to patients and their thyroid disease Basic principles of the 24h00 I-131 uptake procedure Explain the use of this procedure and all the important precautions and preparations Apply to patients and their thyroid disease Basic principles of the I-123 whole body imaging Explain the use of this procedure and all the important precautions and preparations Apply to patients and their thyroid disease Role of Tc-99m labelled MIBI in thyroid imaging Explain the use of this procedure Apply to patients and their thyroid disease Non visualizing of the thyroid Name and discuss the causes Apply to patients and their thyroid disease Cold nodules in the thyroid Describe how the lesions developes and name the causes, what is the significance of this type of lesions? Basic Interpretation and usage of the RN procedures and handling of patients Hot nodules in the thyroid Name the causes and discuss the further handling Basic Interpretation and usage of the RN procedures Grave’s as a thyroid disease Discuss the role of NM in the handling of Grave’s patients (diagnostic/therapeutic) Basic Interpretation and usage of the RN procedures Thyroiditis = acute and chronic Discuss the role of NM in the handling of the patients Basic Interpretation and usage of the RN procedures Thyroid Cancers Discuss the role of NM in the handling of this patients (Diagnostic/therapeutic/follow up) Apply to patients and their thyroid disease THYROID SCINTIGAPHY: KNOWLEDGE, UNDERSTANDING and APPLICATION (LEVELS 1-3) MUST KNOW the previously acquired knowledge of the anatomy and physiology of the organs OUTCOMES ASSESSMENT CRITERIA ASSESSMENT TASKS Goiters Discuss the role of NM in the handling of the patients Apply to patients and their thyroid disease Multinodular thyroid /goiter Explain the scintigraphic changes and the importance of it Apply to patients and their thyroid disease Role of pertechnitate in thyroid scintigraphy Name, discuss and explain the usage of TcO4¯ in thyroid disease Basic Interpretation and usage of the RN procedures Role of I-123 in thyroid imaging Name, discuss and explain the usage of I-123 in thyroid disease Basic Interpretation and usage of the RN procedures Role of I-131 in thyroid imaging and uptake countings Name, discuss and explain the usage of I-131 in thyroid disease Basic Interpretation and usage of the RN procedures Role of I-131 in the therapeutic role of NM Name, discuss and explain the therapeutic usage of I-131 Apply to patients and their thyroid disease The role of t ½ (half life time)in the handling of thyroid patients Discuss and explain how it influences the booking of radionuclide studies Apply to patients and their thyroid disease RAI treatment for hyperthyroidism Discuss and explain the significance of RAI treatment Apply to patients and their thyroid disease Follow up of thyroid Cancer patients in NM Department Discuss NM role in the handling of the patients Apply to patients and their thyroid disease MACROSCOPIC ANATOMY • 2 symmetrical lobes, united by an isthmus of glandular tissue • Placed in front of the 2-4th tracheal rings • Pre-tracheal fascia also present in this region and are responsible for the thyroid movement during swollowing process • PYRAMIDAL LOBE:a small portion of gland tissue, projecting upwards from the isthmus (just left to the midline), representing a developmental residue of the thyroglossal duct MICROSCOPIC ANATOMY • • • • • • • The thyroid consists of a mass of follicular cells (98%) Forms a mass of rounded follicels/vesicels full with colloid A single layer of epithelial cells/follicular cells forms the walls of the follicles The thyroid uses this iodine containing product to store its secretions The sectretions contains the Iodine hormone T3 en T4 Only 2% of the cells are parafollicular or C-cells which secrete calcitonin. C cells are present on the outer aspects of the follicles PHYSIOLOGY THYROID HORMONE PRODUCTION AND EXCRETION IODINE HORMONE PRODUCTION (FOLLICULAR CELL FUNCTION) Two phases are involved for iodine uptake in the thyroid to produce thyroxin a)Iodine is TRAPPED in the thyroid b)Iodine is ORGANIFIED in the hormone Pathology can affect one or both of the above Nuclear Medicine helps to differentiate between the two IODINE HORMONE PRODUCTION: • GIT : uptake and absorption of dietary iodine (thyrosine) • BLOOD dietary intake of iodine as IODIDE = how much iodide is there in the blood plasma? Active iodine pump meganism for active uptake of I¯ in the cell in • FOLLICULAR CELL EPITHELIAL WALL : oxidation to Iodine • FOLLICULAR LUMEN*: Iodine + tyrosine = thyroid Hormones MIT + DIT = T3 DIT + DIT = T4 T3 and T4 in thyroglobulin substans • FOLLIKULERE EPITEEL WAND: pinocytosis, and secretion of the thyroid hormones = T3 (free and bounded) T4 (pro H) bounded to TBG, into the blood. • T4 (inactive) T3(active H): in liver, muscles and kidneys • Active/free hormones diffuses into tissue and exerts its metabolic action T3 --------- 5%------ T4 ----- 95% ---- T3 = free /active H + TBG T4 nonactive pro-H + TBG T4 T3 in the liver /muscles and kidneys THYROID HORMONE REGULATING THE LEVELS T3 5% Free T3 + TBG = active hormone T4 95% inactive T4 +TBG = pro H (mostly secreted) T4 T3 (85%) in liver, muscles and kidneys (CALCITONIN FROM the C CELLS) NEGATIVE FEEDBACK MEGANISM HYPOTALAMUS ↓ TRH ↓ PITUITARY GLAND ↓ TSH ↓ THYROID ↓ T4 (T3) + TBG T3 CIRCULATING THYROID HORMONES ↓ 99% are bound to the plasma proteien (TBG) thyroxine binding globulin + free hormones BIOCHEMICAL MEASURING OF THE THYIROID HORMONES Measure both the free hormone levels as well as the total concentration of the bounded plasma hormone levels LEVELS of BOUNDED HORMONES DEPEND ON THE LEVELS OF THE BINDING PROTEIN/GLOBULINN (TBG) INCREASED • • • • • Pregnancy Contraceptive pills Estrogen therapy Liver disease Hyperthyroidism DECREASED Androgen Nephrosis THYROID’S HANDLING OF IODINE PLASMA IODIDE POOL FOLLICULAR CELL WALLS COLLOID IN LUMEN SIZE How much iodide is there in the blood plasma? I)Uptake of iodine from GIT as iodide I¯ iodided salt UPTAKE/CONCENTRA ORGANIFICATION -TION/TRAPPING Building into the thyroid # the trapping hormones function does not #organification defects necessarily correlates Present with increased with the biochemical uptake with decreased thyroid functions # biochemical TF medications like Corderone X Kelp products, lugols Contrast medium (CT) Technesium is handled in the same way. (Iodine and Tc-O4-) Iodine on it’s own like in I-131 uptake study 2) Endemic geographic regions with decreased levels of iodine in the water and ground ELTROXIN is blocking this function Neomercazole is block ing this function IODINE UPTAKE *** INCREASED Hashimoto Thyroiditis DECREASED Virus thyroiditis Hyperthyroidism Due to Grave’s or Plummers Hypothyroidism primary or secondary to Iodine contamination Iodine deficiency due to increased/ rapid turnover and Iodine setback T4 administration Like Eltroxin therapy Nephrotic syndrome Contras medium administration during radiology examinations + goiterogenic substances Enzyme deficiency Administration of Lugols or Neomercazole THYROID HORMONE FUNCTIONS Metabolism of all body cells Secondary to this metabolism Protein catabolism increased milk production Carbohydrate absorpsion Accelerate heart rate Glucose combustion acceleration Lowers the pheripheral resistance, hyperdynamic blood circulation Accelerate lipid synthesis Stimulates the central nerve systen, causing irritability Stimulates growth and development of the brain function Accelerate the need for vitamins RADIO-ISOTOPES USED IN THYROID DISEASES Diagnostic: Pertegnitate Tc-labelled MIBI I-131 fluid and capsules I-123 Therapeutic: (Hyperthyroidism/Thyroid Carcinomas) I-131 fluid TECHNESIUM - 99M Tc-99M PERTECHNETATE • • • • • • • • • • • Used in Nuclear Medicine (NM) since1957 when the 99Mo-Tc-99M GENERATOR was developed 86% off ALL THE NM studies are carried out with it! Is the most widely used radionuclide for routine scanning Cannot do more than one Tc-99m labelled studie/patient/day! Overlapping of images take place. Is constantly produced by the GENERATOR and is 24 hourly available! IS CONCENTRATED/TAKEN UP or TRAPPED BUT NOT organified by the thyroid follicle The images is a reflection of the trapping properties/function of the thyroid Very good physical character for imaging T ½ = 6 h, with 140 KeV PHOTON ENERGY Very good tissue penetration and imaging possibilities with the Gamma Contains only GAMMA rays (no Beta rays) Low absorbed radiation dosages Distribution of plain Technesium: *thyroid *salivary glands *stomach epithelium TECHNESIUM THYROID SCINTIGRAM INDICATIONS: Taken up, trapped or concentrated by the follicular cell of the thyroid! 1. Evaluation of the – Thyroid’s Morphology and position --Thyroid’s function in comparison to the salivary glands (HYPER/HYPO) 2. Looking for ectopic thyroid tissue 3. Looking for residual thyroid tissue after thyroidectomy 4. Diagnosing the presence of thyroid nodules PREPARATION: • STOP Thyroid blocking MEDICATIONS like ELTROXIN and NEOMERCAZOLE at least 3 weeks prior to the study IODINE containing medications like the CORDERONE X , LUGOLS, KELP PRODUCTS, BETADINE • Get the history of CT SCANNING with the administration of CONTRAS MEDIUM OR ARTERIOGRAMMES IN the past 3 MONTHS • PREVIOUS RAI Rx, CHIR/ HEAD + NECK XST • STOP INGESTION of GOITEROGENIC FOODS like cabbage . NORMAL THYROID SCAN 1. The presence of functioning thyroid tissue 2. Position of the thyroid 3. Size of the thyroid 4. Total uptake of RA (in comparison to the salivary glands) 5. Presence of any nodules on the pinhole image REQUIRE MOST RESENT BIOCHEMICAL THYROID FUNCTIONS THE EFFECT OF DISEASE ON CELLFUNCTIONS COLD NODULES HOT NODULES NON-VISUALIZING of the THYROID – REASONS? EFFECT of CORDERONE X MIBI THYROID SCAN in patient using Corderone X THE ROLE OF Tc-99M LABELLED MIBI IN THYROID IMAGING • MIBI is beter known as the MIOCARDIAL PERFUSION agent (show similarities with 201 Tl) • Meganisms of uptake into the thyroid cells are bloodflow cell membrane potential mitochondrial contents and function • Used to image cold nodules in the thyroid, to confirm THE PRESENCE OF THYROID TISSUE! • Also used for Parathyroid adenoma imaging, due to the better and lower background activity in comparison to that of 201 Tl • RN mammography, detection of tumours of the brongus, thyroid and brain. • The delayed uptake after 2-3 hours increase the sensitivity of the MIBI studies. MIBI Wholebody scan Technesium thyroid scan 23/10/07 Technesium thyroid scan 15/11/07 Normal R lobe Probably enlarged L lobe Total uptake to low to evaluate the thyroid’s Fx MIBI thyroid = ONLY confirms the Presence of thyrois tissue NO Fx information Massively enlarged Left lobe with irregular upake on the lat aspect (confirmed with the sonar) 31 Pertechnetate THYROID scan THYROID IS ?? BLOCKED non visualization of the thyroid MIBI THYROID CONFIRMS THE UPTAKE MIBI IN THE THYROID NODULE 32 Painfull thyroid mass, patient with possible hyperthyroidism Pertechnetate thyrois scan No thyroid tissue present in the cold region 33 TECHNESIUM THYROID MIBI THYROID 34 IODINE RADIO-ISOTOPES eg I-131(reactor) and I-123(cyclotron) IODINE 131: • • • • • • • • Halflife = 8.02 days, physical halflife long enough for therapy the agent of choice for radio-active treatment of hyperthyroidism and thyroid ca patients Cheap radio-activity, readily available Both gamma and B radiation that is being emitted Medium energy BETA emission (0.61 MeV) Beta particles causes ionizing effects by a path length of 1-2mm, allowing local irradiation of eg thyroid gland tissue alone. Practically no effects on the surrounding tissues Also High energy GAMMA radiation , that results in poor images contributes to whole body radiation burden adds to radiation dose of staff and patient relatives Is a Halogen that vapourates and contamination of the atmosphere takes place during dispensing of the liquid form (can be minimized by using the I-131 capsule) THE ROLE OF I-131 IN THYROID IMAGING AND TREATMENT (A) 24H00 I-131 UPTAKE : for the workout of BIOCHEMICALLY HYPERTIROIDISM PATIENTS • NORMAL UPTAKE = 15-45% • INCREASED I-131 UPTAKE = Iodine deficiency • = Hyperthyroidism • = Hashimoto Thyroiditis • = Nephrotic syndrome • = Enzyme deficiency • DECREASED I-131 UPTAKE = Hypothyroidism • = Eltroxin en Lugols Rx • =Neomercazole Rx • = Contras medium administration during radiology examinations + goiterogenic substances = IS BEING USED IN THE CALCULATIONS OF THE RAI Rx DOSAGES • NEGATIVE PREGNANCY TESTS REQUIRED PRIOR TO STATRING GRAVE’S PATIENT’S WORKOUT BEFORE RAI TREATMENT FIRST: RA I-131 UPTAKE THEN: TECHNESIUM THYROID SCAN ALSO: THYROID FUNCTION RESULTS NEG PREGNANCY TEST FINALLY: RAI RX WITH I-131 37 Tiroied teller / Thyroid counter (B) RAI THERAPY: 2 TIPES a) HYPERTHYROIDISM TREATMENT: 10-20 mCi orally MAX EFFECT after 8-12 WEEKS CAN ONLY REPEAT THIS Rx AGTER 3 MONTHS COMPLICATIONS: RADIATION THYRODITIS HYPERTHYROIDITIS DIRECTLY POST TREATMENT (treated with INDERAL) HYPOTHYROIDISM AFTER A FEW WEEKS (treated with Eltroxin) NO EVIDANCE OF THYROID CANCER DANGER AFTER RAI Rx b)THYROID CA PATIENTS = ABLATION DOSAGE 100-200 mCi ISOLATION TREATMENT FOR 1 WEEK RADIATION THYRODITIS BEEN DONE AT RADIOTHERAPY AT NATIONAL HOSP (C) I-131 WHOLEBODY IMAGING: FOLLOW UP OF THE THYROID Ca PATIENTS if the I-123 IS NOT AVAILABLE DONE POST THYROIDECTOMY, STOP ELTROXIN 3 WEEKS PRIOR TO IMAGING, RELATIVELY POOR IMAGES. 2mCi ORALLY ADMINISTRATED IMAGING TAKES PLACE ON 24H AND 72H POST ADMINISTRATION 20 mCi RAI THERAPY 5 DAYS PRIOR TO THIS IMAGING WAIT 8-12 WEEKS (3 MONTHS) IODINE I-131 WHOLE BODY RESIDUAL THYROID TISSUE • IODINE 123: • • • • • • • • • • • • Iodine-123 (123I or I-123) is a radioactive isotope of iodine used in nuclear medicine imaging (Best for imaging) Iodine-123 is produced in a cyclotron by proton irradiation of enriched xenon. (Very expensive), (Only Wednesdays available) Its half-life is 13.22 hours; the decay emits gamma radiation with predominant energies of 159 keV and 27 keV. In medical applications, this radiation can be detected by a gamma camera. 123I is the most suitable isotope of iodine for the diagnostic study of thyroid diseases. 123I has other advantages for diagnostic imaging thyroid tissue and thyroid cancer metastasis.[1] T Stop Eltroxin 3 weeks prior To investigation it block’s thyroid and mets! ROLE OF I-123 IN THE THYROID A. NON VISUALIZING OF THE THYROID B. FOLLOW UP OF THYROID CA PATIENTS POST SURGERY AND POST ABLATION TREATMENT RESIDUAL THYROID TISSUE PRESENT LUNGMETS THYROID DISEASES • EUTHYROIDISM: GOITERS • HYPERTHYROIDISM • HYPOTHYROIDSM • THYROID NODULES • THYROID CANCERS • THYROIDITIS (akuut/chron) • ECTOPIC THYROID TISSUE EUTHYROIDISM and THYROID DISEASES • GOITERS ( = enlarged thyroid with NORMAL blood levels of TF) CAUSES : ENDEMIC GOITERS: IODINE DEFICIENCY in ground and water Especially the mountain regions of the EASTERN FS and LESOTHO ENOUGH DIETARY IODINE, BUT THYROID’S UPTAKE OF IODINE IS BLOCKED BY CERTAIN MEDICATIONS LIKE Metronidasool, tiosianaat, tio-urasiel YOUNG WOMEN: (15-25years) assosiated with pregnancy OLDER WOMEN: NODULAR GOITERS ( retro sternal ) BIOCHEMICALLY HYPOTHYRIODISM OR EVEN EUTHYRIODISM ORGANIFICATION DEFECT MULTI-NODULAR GOITER HYPERTHYROIDISM • GRAVE’S (outo-immuun/antibody condition) • NODULAR GOITERS single nodule Plummer syndrome multi-nodular • THYROIDITIS sub acute viral/De Quervain chronic OI thyroiditis/Hashimoto thyroiditis Radiation thyroiditis • EXOGENE IODINE CONTAMINATION • TSH TYPE OF STIMULATION chorio ca pituatary tumour testis tumour TOXIC NODULES PLUMMER’S GRAVE’S DISEASE CAUSES FOR HYPERTHYROIDISM : • GRAVE’S DISEASE • PLUMMER DISEASE autonomous functioning thyroid lobes or nodules • MULTI-NODULAR GOITERS • VIRUS THYROIDITIS • POST XST /RADIATION THYROIDITIS • HASHIMOTO THYROIDITIS (only the early stages) • Exogene I- contamination (drinking iodine containing medications bv corderone X) • TSH STIMULATION by pituatary tumors / ovarian chorio ca HYPOTHYRIODISM CAUSES • PRIMARY: • SEKONDARY: • THYROIDITIS: Cretinism Primary hypothyroidism idiopathic miksedoema outo-immune failure genetic enzyme defects intake of goiterogenic substances lithium, contras medium, corderone X post surgery + post radiation + post RAI therapy TSH deficiency post partum Hashimoto thyroiditis (chron) • ENDEMIC IODINE DEFICIENCY: geografic/endemic HYPOTHYROIDISM: COLD NODULES SINGLE COLD NODULES: ADENOMATEUS HYPERPLASIA COLLOID CYSTS HEMATOMA EXTERNAL PRESSURE ON THYROID ???THYROIDITIS THYROID CA: 10 – 20% COULD BE MALIGNANT 3-4% DON’T TAKE UP Tc - 99M CAN DO A I-123 SCINTIGRAM OR A MIBI SCAN**** NON-HOMOGENOUS UPTAKE: MULTI-NODULAR THYROID 70% due to ADENOMATEUS HYPERPLASIA FOLLICULAR ADENOMA COLLOID CYSTS, THYROI DITIS, MULTI-NODULAR GOITER due to Iodine deficiency 30% due to THYROID CA after HEAD and NECK Radiation at RADIOTHERAPY HASHIMOTO THYROIDITIS (OI DISEASE, TOTAL BURN OUT TAKE S PLACE ) PLUMMER ‘S DISEASE POST SURGERY HYPERTHYROIDISM THYROID CANCER THYROID CARCINOMAS • 95% FOLLICULER HEMATOGEN PAPILLARY (80-90%) LYMPHATIC spread , usually young men, very good survival rate • <5% MEDULLARY (C-CELLS) ANAPLASTIC highly malignant, older people, LOCAL PRESSURE Sx. DO NOT TAKE UP IODINE PAPILLARY THYROID CA FOLLICULAR THYROID CA LONGMETS ANAPLASTIC THYROID CA MEDULARY THYROID CA • Are not discussed in this lecture • Develop from the C - cells • Imaging Radionuclides are: I-123 MIBG Pentavalente DMSA PET scans “CSL” ACTIVITIES: ( PLAIN Tc-thyroid scintigram) WHAT IS IMPORTANT ON GP LEVEL • • • • • • • • • • • Technesium Thyroid Scintigram/Scan is a RN procedure without any side effects, can easily been organized and done on an outpatient base Call Nuclear Medicine Dept and make the booking to ensure availability of the radioactivities and functionality of the gamma cameras. (051-4053487/8) PATIENT IS THE SOURCE OF RADIATION BEWARE of patient contacts in Hospital Commuter busses ( pregnant women and small children ) especially when going back home after the thyroid scan and tests were done. They can drive with other people after diagnostic scan, but make sure that they do not book a seat next to a pregnant woman or near small children. Correct bookings is very important Prepare the patients for the waiting periods for the RN scintigrams. The waiting period for plain thyroid scan is 20 min with imaging time of half an hour, total duration of at least one hour after getting the RA injection. After receiving the report of the thyroid scan patient can leave for specialist clinic or go wait for rest of the patients at the Commuter transport busses No need to keep patients without food or water from the previous evening. Can eat and drink normally. Important to stop all medications that can block the thyroids uptake of the radioactivity at least 3 weeks prior to the scans. STOP Eltroxin, Celp products, Neomercazole, Corderone X, AND report any contrasmedium investigation being done in previous 3 weeks. Patient will be radio active for at least 24h00 after the thyroid scan Don’t bring along any small children or pregnant family members Don’t refer pregnant patient’s, make sure patient’s is not pregnant. Send along a most recent negative pregnancy test and biochemical thyroid functions In case of a lactating patient, the patient must milk out prior to the thyroid scans and arrange for alternative feeding for the baby for the next 24 hours. Only one RN study can be done on the same patient per day. THERAPEUTIC FUNCTION RAI THERAPY IODINE RADIO-ISOTOPES FOR THERAPEUTIC USE • I-131 is the agent of choice, with both beta and gamma rays that are being emitted. The beta rays are responsible for the irradiation of the thyroid tissue alone. • With a half life of 8.02 days, the physical half life is long enough for uptake and organification by the follicular cells of the thyroid. • It’s a relatively cheap radionuclide, readily available and in the liquid form, oral administration is easy. It is unfortunately a halogen that vapourises, and can cause atmospheric and staff contamination. The capsule form can minimize this risk. HOW DOES THIS WORK?? • The RAI is administrated orally, and is absorbed rapidly from the stomach. It quickly accumulates in the overactive thyroid and is used in the synthesis of the thyroid hormones (in the place of stable dietary iodine). • It provokes an acute inflammatory response in the thyroid, followed by cellular necrosis, atrophy and fibrosis with a chronic inflammatory response. • Loss of active thyroid gland tissue results in release of less thyroid hormones. • The thyroid size is reduced and hyperthyroidism is cured. • The extent of this reaction depends on • amount of RAI taken up by the thyroid • the radio-sensitivity of the thyroid. FACTORS THAT INFLUENCE THE EFFICACY OF THE RA I-131 DOSE 1) Functioning mass of overactive thyroid tissue 2) The presence of uniform or multi-nodular thyroid tissue 3) % Uptake of I-131 as being calculated during the diagnostic uptake study 4) Tempo of Iodine clearance from the thyroid ( influenced by exogenous factors such as intake of iodine containing drugs, food and contrast medium investigations 5)Radio-sensitivity of the thyroid • All this must be taken in consideration when the treatment dosage is determined. AIM OF THE TREATMENT • 1)To induce cellular hypofunction of the overactive thyroid cells • 2) To reduce hypersecretion of thyroid hormones • 3) To achieve rapid improvement of the hyperthyroidism • 4) To restore the euthyroid state of the patient is difficult ---it can be temporary, and be followed by either hypo-or hyperthyroidism • 5) Hypothyroidism remains the most likely result and is considered to be the desired consequence. COMPLICATIONS AND RISK FACTORS • Radiation thyroiditis • Sialo-adenitis like parotitis • Transient exacerbation of the hyperthyroiditis symptoms, this can precipitate a thyroid crisis/storm in the elderly and patients with co-existing cardiac or other medical illnesses • Transient/Permanent Hypothyroidism that develops progressively over 2-6 months. It is easily treated with eltroxin. Regular S-TSH levels must be done. • Hypo-parathyroidism, after treatment of post thyroidectomy recurrence • Worsening of the opthalmopathy • Osteoperosis due to elevated levels of thyroid hormones and calcitonin dysfunction after the RAI treatment • Risk of residual/recurrent hyperthyroidism DOSAGE AND MEASUREMENT UNITS • • • • • • • • • • • 1mCi radio-activity = 37 MBq (mega bequerals) 5mCi I-131 gives a radiation dose of the same magnitude as a common radiological procedure similar to an IVP or Ba enema 1Gy = 100rads 1μCi deliveres 1 Rad of radiation to the thyroid 5mCi I-131 delivers 4000 Rads to the thyroid The usual sufficient intra-thyroid absorbed dose of 150Gy (10mCi) is syfficient to treat the hyperthyroid patient, but with relativly high recurrence rates e.g. 46% after 60Gy and 14% after 150Gy. In high risk patients a higher ablative dose of 300-400Gy (± 20mCi) is necessary to establish an euthyroid state without the need for a second RAI dose. For this ablative regime the incidence of hypothyroidism is 86% after 3 months, and 93% after 18 months RISKS OF THE RAI TREATMENT • THE PATIENT • • • Teratogenicity: Verify that the patient is NOT PREGNANT at the time of treatment. A negative pregnancy test must be obtained before starting the diagnostic procedures. Ensure adequate contraception usage before patient is discharged after the treatment. Beware of large radiation exposure after 10-12 weeks of pregnancy, because the fetus thyroid starts to concentrate iodine and the thyroid can be damaged. Genetic damage: If treated with RAI, it is recommended that the patient DELAY any pregnancies for at least 6 months. Carcinogenesis: No evidence was found that I-131 induced any cancer, RAI treatment for Grave’s does not cause thyroid cancer. Only patients who undergo head and neck irradiation have an increased incidence of thyroid ca. A higher rate of thyroid adenomas is found after RAI treatment to younger children. • Cell dysfunction: RAI treatment induces follicular thyroid cell hypofunction after the initial radiation thyroiditis phase. ONLY the hyperthyroidism is treated in Grave’s disease, NOT the immunological disorder. There is then an increased risk for Grave’s opthalmopathic effect and pre-tibial myxedoema. Anti thyroid drugs with their immuno-suppressive effect could theoretically protect against opthalmopathy. • THE FAMILY AND GENERAL PUBLIC • • • THE PATIENT IS THE RADIATION SOURCE !!!! AND CAN CAUSE A RADIATION HAZARD . The patient and his/her excretions (urine) is the source of radiation after the RAI treatment. The radio active urine must be treated carefully, and patients must not spill any urine. The tiolet must be flushed 2 times and hands washed afterwards. Patients must be informed beforehand of the radiation risk/hazard they can cause after the treatment, and measures must be put in place to reduce the radiation dose to healthy members of the public and their families. Especially pregnant women and small children must be avoided during the first 2 days post therapy THERAPY PROCEDURE AND INFORMED CONSENT • Dietary Iodine is important in the synthesis of thyroid hormones • RA I-131 is administrated orally as therapy, and the follicular thyroid cells incorporates this Iodine into it’s hormones. The amount of Iodine in the RAI is very low and there is seldom any adverse effects or complications. Patients can complain of headache, sore throat or nausea after drinking the RAI fluid, but it is only the probability of vomiting that causes concern, due to the RA contamination hazard. • • The RAI dosage is prescribed by the Radiation Therapist. The Medical Physicist assists the medical doctor to obtain the correct dosage. The Iodine fluid must be handled carefully, and due to its ability to vapourise, athmospheric contamination can be prevented by using the I-131 capsules. • Before administration, the patientmust be informed orally and in writing of all the precautions and radiation safety measurements . The informed consent must be signed by the patient or by the legal guardian of under aged children. Written information are also given to ward personel and families . • Patients are asked to drink the RA fluid through a straw, after which the physicist will measure the radio-activity radiating from the patient to make sure he/she is within the legal limits before discharge. WHAT HAPPENS TO THE PATIENT AFTER THE THERAPY WAS GIVEN?? • FOLLOW- UP AND ADJUVANT TREATMENT e.g. BBLOCKERS, ANTI-THYROID MEDICATION – The maximum effect will only be seen 8-12 weeks posttreatment – Follow–up blood investigation must be done 5 weeks posttreatment. Before 5 weeks the effect of the radiation thyroiditis can be confusing due to worsening of the hyperthyroid status. – That’s why patients must continue to use their B-Blocker therapy in this period. – Hypothyroidism must be detected and treated. – If the patient is still hyperthyroid 3 months post-treatment, follow- up diagnostic procedures can only start after the 812 week waiting period. • NB NB The follow up of these patients are done by the referring doctors and NOT by the Nuclear Medicine Clinic