* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Antibiotic Use: The Fluoroquinolones
Acute pancreatitis wikipedia , lookup
Gastroenteritis wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Neonatal infection wikipedia , lookup
Urinary tract infection wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Infection control wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
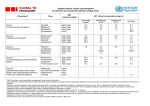
Antibiotic Use in the ED: The Fluoroquinolones (FQ) Hannah Allegretto University of Pittsburgh School of Pharmacy PharmD Candidate 2013 S Objectives S Identify the structure, mechanism of action, and significant drug interactions of FQs S List resistance mechanisms for the FQs S Identify common infections seen in emergency departments and provide treatment recommendations utilizing proper use of the FQs S Describe the role of nursing in enforcing CMS core measures FQ Background S Synthetic broad spectrum antibacterial activity S Same skeleton as quinolones, but fluorine atom attached at C6 or C7 position S MOA: inhibit bacterial replication by blocking their DNA replication pathway S Concentration-dependent bacterial killing S Should be reserved for severe infections or when other regimens have failed Generations S First (quinolones) S Rarely used S Nalidixic acid S Second S Divided into Class I and Class II Class I: Norfloxacin S Class II: Ofloxacin, ciprofloxacin S S Third S Levofloxacin S Fourth S Gatifloxacin, moxifloxacin, gemifloxacin FQ Adverse Effects S Gastrointestinal (2-20%) S Nausea S Anorexia and dyspepsia S Diarrhea S Musculoskeletal S Central Nervous System (1-11%) S Headaches S Dizziness and drowsiness S Restlessness/insomnia S Convulsions/seizures S Cardiovascular S Dermatologic (0.5-3%) S Phototoxicity S Ciprofloxacin > norfloxacin, ofloxacin, levofloxacin > moxifloxacin, gatifloxacn S Arthropathy (1%) S Tendonitis/Tendon Rupture S QTc interval prolongation S Tachycardia Drug Interactions S Antacids, Minerals, Sucralfate, Food S Significant reduction of oral absorption of the FQ S 98% decreased bioavailability of FQ when administered with sulcralfate S When administered with food, peak concentration times delayed, maximum plasma concentrations are decreased 8-16% S Deemed not clinically significant S Recommend: Antacids/sucralfate should be taken at least 2 hours before or 4-6 hours after FQ S Probenecid S Inhibits renal tubular secretion of the FQ S Recommend: Patients receiving renally eliminated FQ + probenecid should be monitored for AEs. Drug Interactions S Theophylline/Caffeine S Dependent on the affinity for FQ to CYP 1A2 S ciprofloxacin > norfloxacin > ofloxacin > levo/gati/moxifloxacin S Recommend: all patients receiving FQ + theophylline must be monitored for theophylline toxicity S Warfarin FQ can inhibit hepatic CYP enzymes responsible for metabolizing warfarin S Recommend: when possible, avoid FQ. If not possible, monitor INR more frequently, especially upon initiation and discontinuation of FQ S Renal Dosing Adjustments S FQ’s requiring renal dosage adjustments: S Ciprofloxacin S Levofloxacin S Norfloxacin S Ofloxacin S Gemifloxacin S Both decreased dosages and decreased dosing frequency required Resistance Mechanisms S Increased use of FQ in 1990s led to doubling rate of resistance to ciprofloxacin from gram-negative bacilli in hospitals S Mechanisms: S Mutations altering drug targets (DNA gyrase, topoisomerase IV) S Mutations reducing drug accumulation S Plasmids blocking quinolone effects qnr gene FQ Indications in the ED S Acute Uncomplicated Cystitis and Pyelonephritis S Intra-abdominal Infections S Community Acquired Pneumonia Acute Uncomplicated Cystitis S One of most common reasons for otherwise healthy women to get prescribed antimicrobials S Fluoroquinolones should only be considered after previous recommended treatment regimens are ruled out S Preferred agents: Nitrofurantoin, SMX/TMP, Fosfomycin S Ofloxacin, ciprofloxacin, and levofloxacin highly effective in 3 day regimens, but “have a propensity for damage and should be reserved” Acute Pyelonephritis S Non-hospitalized patients with prevalence of resistance of community uropathogens <10% S SMX/TMP 800/160mg PO BID x 14 days if uropathogen known to be susceptible S If susceptibility not known, 1g ceftriaxone IV recommended S Ciprofloxacin 500mg PO BID x 7 days S Optional loading dose of Ciprofloxacin 400mg IV S Once daily FQ S Ciprofloxacin 1000mg ER PO QD x 7 days S Levofloxacin 750mg PO QD x 5 days Intra-abdominal Infections S Empiric treatment should be active against enteric gram- negative aerobic and facultative bacilli and enteric grampositive streptococci S Obligate anaerobic bacilli coverage recommended if distal small bowel, appendiceal, and colon-derived infection present S For high risk patients (APACHE II scores > 15), combination therapies with metronidazole are recommended S Quinolone-resistant E. coli common quinolones should be avoided unless >90% susceptibility is known Intra-abdominal Infections Regimen Mild-to-Moderate severity High risk or severity Single Agent Cefoxitin, ertapenem, moxifloxacin, tigecycline, ticarcillin-clavulanate acid Imipenem-cilastin, meropenem, doripenem, piperacillin-tazobactam Combination Therapy Metronidazole + one of the following agents: Cefazolin, cefuroxime, cefriaxone, cefotaxime, ciprofloxacin/levofloxacin Metronidazole + one of the following agents: Cefepime, ceftazidime, ciprofloxain/levofloxacin Community Acquired Pneumonia (CAP) S One of the leading causes of hospital admissions S Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis account for 85% CAP cases S >$17 billion annual US costs due to CAP CMS Core Measures: CAP S Core Measures: S Blood cultures performed within 24 hours prior to or 24 hours after hospital arrival for patients transferred/admitted to the ICU within 24 hours of hospital arrival S Blood cultures performed in ED prior to initial antibiotic received in hospital S Nursing plays role S Always DOCUMENT! S Selection of most appropriate antibiotic based on patient characteristics Nursing Role S Verify documentation of time when blood cultures taken S Review recent antibiotic use through chart review/patient interview S Verify susceptibility of pathogen to antibiotic being administered S Ensure proper documentation of admission times, time to culture, and time to antibiotic administration to comply with CMS core values. CAP Tx Recommendations Non-ICU patients: S Primary Regimen: S Ampicillin/sulbactam IV PLUS azithromycin IV/PO S Non-severe PCN allergy rxn S Cefriaxone IV PLUS azithromycin IV/PO S Severe PCN allergy rxn S Moxifloxacin monotherapy ICU Patients: S Primary: Ampicillin/Sulbactam IV + Azithromycin IV S Secondary: Azithromycin IV + Ceftriaxone IV CAP Tx Recommendations Non-ICU pts w/ Pseudomonal Risk S Cefepime IV + tobramycin IV + azithromycin IV/PO S Second Line: Cefepime IV + Ciprofloxacin IV/PO S With SEVERE B-Lactam allergy: Aztreonam IV + Moxifloxacin IV + Tobramycin IV ICU pts w/ Pseudomonal Risk S Cefepime IV + Tobramycin IV + azithromycin IV S Second Line: Cefepime IV + Ciprofloxacin IV CAP Tx Recommendations S ICU Pts with SUSPECTED Francisella tularensis or Yersinia pestis S Doxycycline + ampicillin/sulbactam IV or cefepime IV Summary S The FQs exhibit powerful antimicrobial activity against several organisms, but should be reserved in use due to high risk of resistance S Hospital nurses involvement imperative in ensuring the CMS core measures for community acquired pneumonia are being abided by in order to ensure reimbursement References Hooper, DC. Mode of action of fluoroquinolones. Drugs 1999; 58 Suppl. 2; 6-10. Hooper, DC. Mechanisms of action of antimicrobials: focus on fluoroquinolones. Clin Infect Dis. 2001; 32: s9-15. Oliphant CM, Green GM. Quinolones: A comprehensive review. Am Fam Physician. 2002; 65: 455-65. Fish DN. Fluoroquinolone adverse effects and drug interactions. Pharmacotherapy. 2001; 21: 10s. Jacoby GE. Mechanisms of resistance to quinolones. Clin Infect Dis. 2005; 41: s120-6. Solomkin JS, Mazuski JE, Bradley JS et al. diagnosis and management of complicated intra-abdominal infection in audlts and children: The Guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:133-64. References Gupta K, Hooton TM, Naber KG et al. Internation clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 updated by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Idis. 2011;52:e103-120. File TM, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010; 122:130-41 Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007; 44:s27-72.