* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download System and method of AV interval selection in an implantable
Heart failure wikipedia , lookup
Myocardial infarction wikipedia , lookup
Cardiac surgery wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Electrocardiography wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Atrial septal defect wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
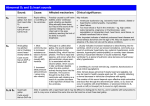
USOO8498705B2 (12) United States Patent (10) Patent N0.: Chirife et a]. (54) (45) Date of Patent: SYSTEM AND METHOD OF AV INTERVAL (56) U.S. PATENT DOCUMENTS (75) Inventors: Raul Chirife, Acassuso (AR); William - ~ ~ 4 485 813 A 12/1984 And 5,154,171 A 5,179,949 A 5,267,560 A 10/1992 Chirife 1/1993 Chirife 12/1993 Cohen 5,330,511 A 7/1994 Boute 437193921 A J. Combs, Mlnnetonka, MN (US); Russell R. Lundstrom, Coon Rapids, MN (US) . *Jul. 30, 2013 References Cited SELECTION IN AN IMPLANTABLE MEDICAL DEVICE ~ US 8,498,705 B2 t l. M988 Chirfgon e a 5,334,222 A 8/1994 Salo et al. (73) Ass1gnee. Medtronlc, Inc., MInneapohs, MN (US) 2002/0151938 A1 (*) 2003/0028222 A1 200% Stahmann FOREIGN PATENT DOCUMENTS Notice: Subject to any disclaimer, the term of this patent is extended or adjusted under 35 This patent is subject to a terminal dis- EP 10/2002 Corbucci 607951 Clalmer' 7/1994 OTHER PUBLICATIONS (21) Appl- NO-I 13/037,780 International Search Report, PCT?JSZOO6/041247, Sep. 2, 2007, 7 (22) p g a cs. Filed: Mar. 1, 2011 (65) Prior Publication Data Us 2011/0152964 A1 J Primary Examiner * Kennedy Schaetzle 23 2011 un' ’ Assistant Examiner * Erica Lee (74) Attorney, Agent, or Firm * Reed A. Duthler Related US. Application Data (62) Division of application No. 11/257,643, ?led on Oct. 25 2005 ’ ’ now (51) Int CL A 61N 1/08 (52) U 5 Cl U'Séc ' (58) Field P t. N .7 899 533. a O ’ ABSTRACT . . . . . An Implantable med1ca1 deVIce prOVIdes ventr1cu1ar pac1ng capabilities and optimizesAV intervals for multiple purposes. In general, intrinsic conduction is promoted by determining When electromechanical systole (EMS) ends and setting an (200601) """"" u (57) . ’ 607/25 607/9 AV interval accordingly. EMS is determined utilizing various ’ data including QT interval, sensor input, and algorithmic USPC .................. .. 607/9, 17, 18, 25; 600/509, 513, calculanons' 600/5 1 6, 5 17 See application ?le for complete search history. 10 Claims, 16 Drawing Sheets US. Patent Jul. 30, 2013 Sheet 2 0f 16 US 8,498,705 B2 US. Patent Jul. 30, 2013 Sheet 3 0f 16 US 8,498,705 B2 US. Patent Jul. 30, 2013 US8A98J05B2 Sheet 4 0f 16 Dis-side i 5 Time peréoc's: A Active Tr cuiar P ‘ ?x 9 m ‘ “ \ ystohc 2: pressure T15 US. Patent Jul. 30, 2013 Sheet 5 0f 16 m $1? M m“ EMS TI. EMS US 8,498,705 B2 US. Patent 315 Jul. 30, 2013 Sheet 6 0f 16 US 8,498,705 B2 31g 5 Caicuia‘har’ Puise Genera‘i'or 52.; W‘ Avm?x : CL - QT $5.9 T Cisak Ciock m 3&5. Sigma! iZQ 1w Pmaessor Q QT Dame? fr: 349 m US. Patent Jul. 30, 2013 use. 5404 anem or“ g; Sheet 7 0f 16 US 8,498,705 B2 v (Zlmk F" @ A w “W Calcuimor Ciosk avmax : CL - EMS 4 416 54-18“ W A 58mm 468 M “N W "4119“ M k y Prk559nai I .ncesmr 4i “ » Defac‘ror iii US. Patent Jul. 30, 2013 Sheet 8 0f 16 US 8,498,705 B2 / 566 Puise Generahr‘ 526 m 536 E Frogmmmer 21.9 / V W v REG A REG B REG (3 EMS? CLr CLp REG D IVE) REG E MD R565 F PSO V V v CALCULATIQN MQEBE gig US. Patent Jul. 30, 2013 Sheet 9 0f 16 Upper Rafe ADL Qa’re Lawer 9m HQ, g US 8,498,705 B2 US. Patent Jul. 30, 2013 US 8,498,705 B2 Sheet 10 0f 16 m? Tail $.?53123”.1 ,. MEW E‘HM BE‘ E¢ Emw?m W: a,3.E,N» _ w QtQM Egga US. Patent Jul. 30, 2013 US 8,498,705 B2 Sheet 11 0f 16 Ew?“b. .“ Qt US. Patent Jul. 30, 2013 Sheet 12 0f 16 US 8,498,705 B2 @HmNM $3BE? \V Esmw é $3 123! @Lsm hi US. Patent Jul. 30, 2013 Sheet 13 0f 16 US 8,498,705 B2 2 wm $EUWLEQM 23 $ $365% wham? TE w US 8,498,705 B2 1 2 SYSTEM AND METHOD OF AV INTERVAL SELECTION IN AN IMPLANTABLE MEDICAL DEVICE tioned at the right ventricular apex. Assuming a given patient had no intrinsic rhythm and fully relied upon the pacemaker, This application is a divisional of US. patent application Ser. No. 11/257,643, ?led Oct. 25, 2005 entitled “SYSTEM the rate would always be the device’s escape interval which de?nes an A-A interval. This interval may be varied by the device based upon sensor input to provide rate responsive (RR) pacing. An AVI or AV interval is programmed and may be varied by the device depending upon rate or other factors. AV synchrony is maintained in that a ventricular paced event AND METHOD OF AV INTERVAL SELECTION IN AN IMPLANTABLE MEDICAL DEVICE”, US. Pat. No. DDD pacemaker may operate in this manner. RELATED APPLICATION (VP) will always follow an atrial paced event (AP). A typical 7,899,533, issued Mar. 1, 2011 herein incorporated by refer While the present discussion is overtly super?cial both in terms of the cardiac cycle and operation of a pacemaker, ence in its entirety. several fundamental aspects have been illustrated that are FIELD OF THE INVENTION currently being questioned. The ?rst is that ventricularpacing in the right ventricular apex may not be hemodynamically optimal for all patients. The second is that a programmed AV The present invention relates to implantable medical devices. More speci?cally, the present invention relates to implantable medical devices that are capable of delivering interval that more or less assures ventricular pacing, even to maintain synchrony, is not necessarily optimal in all patients. pacing stimuli. 20 DESCRIPTION OF THE RELATED ART At a super?cial level, the mechanical aspects of the cardiac cycle of the human heart are fundamentally simple. The heart has four chambers. Deoxygenated blood is returned from the Implanting leads into the right atrium and right ventricle is signi?cantly easier than implanting leads to pace the left 25 body to the right atrium. The right atrium (RA) ?lls the right ventricle (RV), which, upon contraction, pumps blood to the lungs. Oxygenated blood from the lungs ?lls the left atrium (LA), which in turn ?lls the left ventricle (LV). The contrac tion of the left ventricle then delivers oxygenated blood throughout the body. Thus, the atrial chambers serve the trodes within the left atrium or left ventricle as this could 30 cycle are also fundamentally simple, at a super?cial level. The 35 Ventricular pacing from the right ventricular apex causes 40 been recognition that intrinsic conduction is preferable to pacing in most cases. That is, even if the AV delay is longer than “normal,” it is preferable to wait for the intrinsically ventricular (V) events. Thus, the activation of the SA node is 45 tricles depolarize. There is a delay and the process is repeated. Thus, normal timing is A-V-A-V, etc. For purposes of under standing the physiology as well as for programming various conducted beat than to pace. This is, of course, at odds with standard DDD (or similar) modes, which will provide a ven tricular pace after a predetermined interval (AVI), which is pacemakers, this simple understanding provides several com 50 will be used herein for explanatory purposes). The time usually short enough that it precludes intrinsic conduction. Certain patients who are pacemaker dependant, e.g., those that have complete heart block, will require and bene?t from such ventricular pacing. Other patients may have pacemakers implanted for other reasons and have intact conduction or may have intermittent block. For those patients, intrinsic con between the atrial event and the ventricular event is the AV interval and not surprisingly, the time between the ventricular event and the subsequent atrial event is the VA interval. As rate is increased, the A-A interval decreases in duration. The AV node modi?es the delay imparted, thus the AV inter val is also reduced. The mechanical actions involved (con of the left ventricle with respect to the right ventricle is skewed electrically and mechanically. Recently, there has depolarizing and contracting the ventricles. The cardiac cycle is often described by atrial (A) events and mon variables. The rate of the heart is de?ned by a complete cycle and may either be an A-A interval or V-V interval (A-A norm. When dual chamber pacemakers are so implanted, the device is typically programmed to operate in a DDD mode or VDD for a single chamber, ventricular pacemaker. Such set tings restore rhythm, but ensure that pacing occurs in a high the depolarization wave to travel a rather unnatural path and while it will cause the left ventricle to depolarize, the timing chambers respond to the depolarization by engaging in a an intrinsic atrial depolarization. Some time later, the ven promote clotting that results in a thrombus. Thus, right side implantation of single or dual chamber pacemakers is the percentage of cardiac cycles. and initiates electrical depolarization of the heart at a prede termined rate, based upon physiologic need. The SA node is located in the right atrium and upon activation, the atrial muscular contraction. The depolarization wavefront eventu ally reaches the AV node, where a delay is imparted before atrium or left ventricle, as leads on the left side are preferably implanted epicardially or within the veins of the heart proxi mate, but external to the relevant left sided chamber. That is, there is a general medical bias against placing leads or elec purpose of ?lling their respective ventricular chambers. Similarly, the electrical and timing aspects of the cardiac sinoatrial node (SA node) is the heart’s natural pacemaker Finally, the entirety of the above discussion was in terms of RA to RV electrical timing, which while common parlance tends to ignore a great many aspects of the cardiac cycle. 55 duction is often if not always possible and is typically pre cluded by standard DDD mode settings. Again referencing a device having leads in the right atrium and/or right ventricle, the timing relied upon both for pro gramming/discussion purposes as well as what is sensed by traction of a chamber; ejection of a ?uid) may occur more quickly, but there is a limit or minimal time required for the implanted device is based upon right side electrical tim ing. The use of right side timing will tend to ignore the delays e?icacious operation. This highly simpli?ed overview can actually provide for of pacing. In a normal, healthy heart the SA node will depo many of the key programming parameters in a given dual chamber pacemaker. Typically, a dual chamber pacemaker will have an atrial lead (and electrode) positioned within the right atrium and a ventricular lead (and electrode) positioned within the right ventricle, generally with the electrode posi in left sided response that occur naturally and/ or as the result larize and generate a wavefront along an atrial conduction pathway that eventually reaches the left atrium causing it to 65 depolarize and contract. The wavefront also reaches the AV node and progresses along the Bundle of His. The left sided pathway propagates somewhat faster than the right, but US 8,498,705 B2 3 4 because the right ventricle is smaller the wavefront leads to a FIGS. 14-16 are ?owcharts illustrating processes utilizing embodiments consistent with the teachings of the present invention. generally synchronized mechanical contraction of both ven tricles. When atrial pacing is introduced, the electrode is typically offset from the SA node, commonly in the right atrial append age, and different conduction (and possibly less e?icient) DETAILED DESCRIPTION FIG. 1 is schematic, sectional diagram illustrating the pathways are taken. See US. Pat. No. 5,179,949, issued to anatomy of a human heart 10. Blood returning from the venous system ?ows into the right atrium 20 from the superior (SVC) 50 and inferior vena cava. In a normal, healthy heart Chirife, which is herein incorporated by reference in its entirety. The net result is that there is an interatrial conduction delay (IACD) that is imposed. That is, the left atrium will 10, the sinoatrial (SA) node 22 produces an action potential that is responsible for the automaticity of the cardiac conduc tion process. A depolarization wavefront is generated and depolarize and then contract after a longer interval from the pacing pulse than would occur intrinsically, i.e., after the SA node initiates depolarization. Thus, if the remainder of the conduction pathway were intact, this would skew the results for ventricular sensing. That is, an A pace occurs and after some interval, ventricular depolarization is sensed in the right ventricle by the pacemaker. This duration is determined to be the AV interval. However, the left atrium did not depolarize simultaneously with the A pace, nor within the normal physi progress through the right atrium (RA) 20 along the atrial conduction pathway 26 to the atrioventricular (AV) node 24. At the same time, the depolarization wavefront propagates from the SA node 22 into the left atrium (LA) 40 along the RA to LA conduction pathway 30. The depolarization wavefront, generally referred to as the P wave triggers a subsequent 20 muscular contraction as it propagates. That is, the electrically detected wavefront, i.e., an EKG, is not identically synchro nized with the mechanical contraction. As blood is ?lling the RA 20, the LA 40 is similarly being 25 ventricle (RV) 46 and the left ventricle (LV) 54 are being ologic window. Thus, the left sided AV (LAV) interval is shorter than the sensed right sided (RAV) interval. That is, LAVIRAV—IACD. ?lled via the pulmonary veins. During this time, the right Another left sided variation to timing occurs when right sided ventricular pacing, particularly at the right ventricular apex is provided. As indicated, normal ventricular conduction passively ?lled with blood ?owing through the tricuspid valve 52 and the mitral valve 56, respectively. When the atrial chambers mechanically contract, they force an additional volume of blood into the ventricles, causing the ventricles to begins at the AV node and more or less simultaneously propa gates along a left and right side of the Bundle of His and spreads around each ventricle. With right sided pacing, the normal conduction pathway is not necessarily activated and 30 When the atrial electrical wavefront reaches the AV node rate. In addition, the wavefront propagates from the apex retrograde along the Bundle of His, then down the left side pathway eventually depolarizing the left ventricle. The delay imparted from the ventricular pace to contraction of the left 35 ventricle is referred to herein as the interventricular conduc tion delay (IVCD). Yet another offset is the difference between an event, e.g., an atrial depolarization, and the time at which that event is sensed by the pacemaker. This delay is referred to as the P 40 These various delays are biased towards right side events. That is, failing to account for such delays may have the most consequence on left side activity, which is generally more 45 BRIEF DESCRIPTION OF THE DRAWINGS FIG. 1 is schematic, partially sectional view of a human heart. 50 heart progressing through a cardiac cycle. FIG. 3 is illustrates a correspondence between depolariza tion events occurring throughout a heart and how those events 55 FIG. 4 is a graph illustrating correlations between a surface the period of isovolumic relaxation, where all valves (AV and semilunar) are again closed. As diastole continues (FIG. 2D), FIG. 6 is a block diagram of a ?rst embodiment of the 60 FIG. 7 is a block diagram of a second embodiment of the present invention. ther ?ll the ventricles. The process then returns to FIG. 2A and repeats. present invention. corresponding EKG data. passive ventricular ?lling occurs as the pressure within the atrial chambers causes the AV valves 100 to open. During active ?lling (FIG. 2E), the atrial chambers contract and fur FIG. 8 is a block diagram of a third embodiment of the FIG. 9 is a graph illustrating device rate limits. FIGS. 10-13 illustrate stylized pressure waveforms and isovolumic contraction. The AV valves 100 (mitral and tri cuspid) and semilunar valves 110 (aortic and pulmonic) are closed at this point. In FIG. 2B, systole continues with the period of ej ection where the out?ow of blood opens the semi lunar valves 110. FIG. 2C illustrates the onset of diastole and EKG, pressure data, volume data and heart sounds. FIG. 5 is a series of stylized EKG tracings. present invention. pid valve 52 and mitral valve 56 to close. The continued contraction ejects a large percentage of the ?uid from the ventricles in a coordinated action. After cardiac cells depo larize, they are refractory for a period of time. The contracted chambers relax and the process repeats. FIG. 2 illustrates some of the mechanical and ?uid ?ow characteristics generated during the cardiac cycle. In FIG. 2A, the heart 10 is entering systole and is in the period of FIGS. 2A-2E illustrate the mechanical contractions of a generate a composite EKG tracing. 24, a delay is imparted. This delay provides time for the atrial chambers to contract and fully ?ll the ventricles, prior to ventricular contraction. After this delay (the PR interval), the depolarization wavefront progresses downward through the ventricular septal wall along the Bundle of His 32 and splits into the left bundle branch (LBB) 35 and right bundle branch (RBB) 36. The bundle branches diverge proximate the apex 42 of the heart 10 and propagate along the Purkinje ?bers 41 surrounding the ventricles. Due to the atrial kick, the ven tricles are expanded or stretched somewhat. As the muscular contraction occurs in response to depolarization, the ?uid pressure within the ventricles increases and causes the tricus wave sense offset (PSO). important to hemodynamic performance. stretch somewhat. This is referred to as atrial kick and improves overall cardiac output. instead propagation from cell to cell may occur at a slower 65 In describing the cardiac cycle, both electrical and mechanical reference points have been described. Typically, the cardiac cycle is represented electrically and most accu US 8,498,705 B2 6 5 Cycle length (CL), as used herein is simply the length of a rately in that context by a surface EKG. Electrodes on the surface of the skin detect, over multiple vectors, the electrical signals generated as depolarization occurs. A complete car diac cycle includes a P wave indicative of atrial depolariza given cycle (e.g., T1 to T10) and may vary on a beat to beat basis due to physiologic demand for an intrinsic rate or con trolled by a pacemaker based upon programmed parameters and various sensory input. As cycle length decreases, the AV interval (T1 to T3) is able to slightly decrease. Similarly, tion, a QRS complex indicative of ventricular depolarization, and a T wave indicative of ventricular repolarization. FIG. 3 illustrates the potential along the conduction pathways and how each portion contributes to the overall represented cycle. ventricular diastole may be shortened. Of note, the electrical representation does not indicate any mechanical effect. That is, there is a difference between the onset of electrical activity and mechanical contraction. Like within certain parameters. The present invention relates to Such variation based upon dynamic cycle lengths is normal promoting intrinsic conduction without permitting these variations from exceeding those normal parameters. As illus trated in FIG. 4, ventricular systole occurs from time T5 with isovolumic contraction and ends at time T8, when isovolumic relaxation begins. This is the time period during which the left ventricle is actually contracting. As used herein, the term wise, the electrical signals do not represent either the strength of ef?cacy of a given contraction. Finally, the representative EKG signal is a summation of electrical activity and does not readily allow for differentiation of certain components. FIG. 4 is a timing diagram that illustrates the correlation in time of an idealized EKG tracing A, pressure graph B, ven tricular volume graph C, and heart sound graph D. The pres sure graph B includes left atrial pressure P1, left ventricular pressure P2 and aortic pressure P3. At time T1, the surface EKG indicates initiation of the P wave (atrial depolarization); however, there is a delay until LA contraction occurs and begins to increase atrial pressure P1 at time T2. Prior to this point, the LV has been passively ?lled and with the LA con traction beginning at time T2, a maximum or end diastolic volume is reached at time T5. electromechanical systole (EMS) begins with either the pac ing pulse or R wave depending upon the embodiment, and ends when passive left ventricular ?lling begins at time T9. In other words, EMS includes a time period initiated by the 20 ends at time T8 or at a time between T8 and T9, as described herein. FIG. 5 illustrates three timing diagrams, schematically 25 Ventricular depolarization begins with the initiation of the QRS complex at time T3. Isovolumic contraction of the LV begins after a delay at time T5 and the pressure within the LV causes the mitral valve to close. Pressure P2 within the LV period of ejection occurs between time T6 and T8 and LV volume (graph C) falls as blood is ejected from the LV into the arterial system. The T wave, or repolarization, begins during the period of ejection, as illustrated. When the falling LV pressure P2 is exceeded by aortic pressure P3, the semilunar valves close at time T8. The time illustrating selected events at various times for different heart rates. In each scenario, the AV interval is constant. In scenario A, the heart rate is assumed to be 70 beats per minute (BPM). At time T1, an atrial pace is delivered with an R wave occur 30 ring at time T2. The EMS is illustrated through time T3 and a second atrial pace is delivered at time T4. The time difference between T3 and T4 is suf?cient for ventricular passive ?lling increases but the semilunar valves remain closed until this pressure exceeds that within the aorta P3 at time T6. When the LV pressure P2 exceeds aortic pressure P3, the semilunar valves open at time T6. LV pressure P2 continues to increase until approximately time T7 and then begins to drop. The pacing pulse (or sensed R wave), mechanical systole, and the period of isovolumic relaxation. In some embodiments, EMS (see FIG. 4). In scenario B, the heart rate is 90 BPM; thus, the A-A interval is shorter than in scenario A. Here, the secondA pace is delivered at time T4, very close in time to the end of 35 40 EMS at time T3. This will overlap the period of passive ventricular ?lling with active ?lling due to left atrial contrac tion. Finally, in scenario C, the heart rate is at 110 bpm. As such, the atrial pace is delivered (T3) during the EMS which ends at T4, causing truncation of active atrial ?ow. There are two undesired results that may occur as an atrial event encroaches the EMS. The ?rst is that the period for period referred to as isovolumic relaxation occurs between active ?lling overlaps with passive ?lling rendering left atrial times T8 ad T9. During this time, LV pressure P2 is falling rapidly, but is still in excess of LA pressure; thus keeping the mitral valve closed. At time T9, the LV pressure P2 falls tion occurs (in full or in part) during the EMS. During this time, the ventricular pressure is higher than the atrial pres contraction less ef?cacious. The second is that atrial contrac 45 below the LA pressure P1 and the mitral valve opens. This sure. Thus, even with atrial contraction, insuf?cient pressure begins the period of passive ventricular ?lling that occurs up is generated to open the AV valves; thus, ?uid ?ow is pre until time T11. A second cardiac cycle is illustrated with the initiation of the P wave at time T10, initiation of active LV ?lling at T11, start of the QRS complex at time T13, R wave at time T14 and isovolumic contraction from T15-T16. The T wave begins at time T17 and isovolumic relaxation begins at time T18. Thus, one complete cardiac cycle may be de?ned from a ?rst P wave at time T1 to a second P wave at time T10. Similarly, the cycle cluded to the ventricles but does occur retrograde into the pulmonary veins and pulmonary capillary vessels. Mean pul 50 monary venous pressure will increase and may result in ?uid passing from the veins into the pulmonary tissue, impeding normal gas exchange. Symptoms similar to that of heart fail ure may occur or preexisting pulmonary edema may worsen. The condition may be referred to as pacemaker syndrome or 55 pseudo-pacemaker syndrome if no pacemaker is implanted. may be de?ned by a ?rst R wave at time T4 to a second R wave at time T14. The surface EKG illustrates the intition of a P As illustrated, in FIG. 5, this occurs at a higher atrial rate with a constant AV More accurately, the AV interval (or PR wave at time T1. It should be appreciated that for a variety of interval) is too long for scenario C; thus leading to the second A pace occurring during the EMS. It should be appreciated, reasons, an implanted device might not sense this same P wave at time T1. Rather, the implanted device will sense the P wave at time T1+PSO, where PS0 is a P-wave sense offset. 60 Depending upon lead placement and location, sensed activa tion is not necessarily the earliest actual activation. While this does not change the times at which the other events occur, it does change how the electrical representation or at least a portion thereof would be shifted with respect to the actual occurrence of these other events. 65 that abnormally long AV intervals may result in the same or similar symptoms even in the absence of atrial pacing. This situation is commonly averted through the use of a pacemaker operating in a traditional DDD mode. A simple solution is to utilize the standard DDD pacing mode with relatively short AV interval to avoid encroachment; however, as previously mentioned, intrinsic conduction is highly pref erable to ventricular pacing when possible. The scenarios