* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Approach to chronic cough in children
Survey
Document related concepts
Gastroenteritis wikipedia , lookup
Oesophagostomum wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neonatal infection wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Leptospirosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Tuberculosis wikipedia , lookup
Neisseria meningitidis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Hepatitis C wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Chagas disease wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Transcript
Approach to chronic cough in
children
د هالة الرفاعي
• INTRODUCTION
• Coughing is an important defensive reflex that
protects from aspiration of foreign
• materials, and enhances clearance of
secretions and particulates from the airways.
Healthy children may
• cough on a daily basis; one study documented
an average of 11 cough episodes every 24
hours
• However, a cough may also be the presenting
symptom of a serious underlying pulmonary or
• extrapulmonary disease. The causes of chronic
cough in children are quite different from that of
adults,
• so evaluation and management of children
should not be based on adult protocols.
Adolescents 15 years
• and older may be evaluated using guidelines for
adults
• The differential diagnosis of chronic cough in
children includes subacute and chronic
infections
• bacterial bronchitis
• pertussis,
• mycoplasma, tuberculosis
• foreign body aspiration, and cough dominant
• asthma
• Gastroesophageal reflux, upper airway cough
syndrome (formerly
• known as postnasal drip syndrome), and
sinusitis are sometimes implicated because of
associations with
• chronic cough in adults, but their role in
causing chronic cough in children is
controversial [
• Less
• common disorders must be excluded if the
cough is unusually severe and/or frequent, or
when there is
• evidence of failure to thrive, growth
retardation, purulent sputum, exertional
dyspnea, hypoxemia, chest
• pain, or hemoptysis
• chronic cough appears to be common, with an
estimated prevalence of 5 to 7
• percent in preschoolers, and 12 to 15 percent in
older children
• Cough is more common among
• boys than girls up to 11 years of age
• and may be less common in developing countries
than in
• affluent countries [
DEFINITION
• There is no consensus as to the length of time in
the definition of chronic cough in
• children. The American College of Chest
Physicians, Thoracic Society of Australia and New
Zealand,
• and many studies have defined chronic cough as
one that lasts more than four weeks, because
most acute
• respiratory infections in children resolve within
this interva
• In comparison, guidelines from the
• British Thoracic Society define chronic cough
as one that lasts more than eight weeks
• However,
• these guidelines also describe a "prolonged
acute cough" as one that lasts at least three
weeks
PHYSIOLOGY
• Each cough occurs through the stimulation of
a complex reflex arc
• This
• is initiated by the irritation of cough receptors
that exist not only in the epithelium of the
upper and lower
• respiratory tracts, but also in the pericardium,
esophagus, diaphragm, stomach, and external
ear
•
•
•
•
Chemical receptors sensitive to acid, heat
mechanical cough receptors can
be triggered by touch or displacement.
The proximal airways (larynx and trachea) are
more sensitive to
• mechanical stimulation, the distal airways more
sensitive to chemical stimulation. Irritation at the
• bronchiolar and alveolar level does not cause
cough
• Impulses from stimulated cough receptors
traverse afferent branches of the vagus nerve to a
"cough
• center" in the medulla and nucleus tractus
solitarius, which itself is under control by higher
cortical
• centers. The cough center generates an efferent
signal that travels down the vagus, phrenic, and
spinal
• motor nerves to expiratory musculature to
produce the cough
• The mechanical events of a cough can be
divided into three phases
• Inspiratory phase: Inhalation, which generates the
volume necessary for an effective cough.
• Compression phase: Closure of the larynx combined
with contraction of muscles of chest wall,
• diaphragm, and abdominal wall result in a rapid rise in
intrathoracic pressure.
• Expiratory phase: The glottis opens, resulting in high
expiratory airflow and the coughing sound.
• Large airway compression occurs. The high flows
dislodge mucus from the airways and allow
• removal from the tracheobronchial tree.
• The specific pattern of the cough depends on the
site and type of stimulation. Mechanical laryngeal
• stimulation results in immediate expiratory
stimulation (sometimes termed the expiratory
reflex),
• probably to protect the airway from aspiration;
stimulation distal to the larynx causes a more
prominent
• inspiratory phase, presumably to generate the
airflow necessary to remove the stimulus
• Cough is an important defensive reflex that is
required to maintain the health of the
• lungs. Children who do not cough effectively
are at risk for atelectasis, recurrent
pneumonia, and chronic
• airways disease from aspiration and retention
of secretions
• Many disorders can impair a child's ability to
• cough effectively, resulting in persistent
cough. Children with neuromuscular disease
and chest wall
• deformities may not generate a deep enough
inspiratory volume or expiratory flow
necessary for
• effective clearance of secretions due to
defective "pump" mechanisms
• Children with reduced
• function of the abdominal wall musculature are particularly
at risk for ineffective cough. Children with
• tracheobronchomalacia
• ("floppy" airways), or with obstructive airways diseases,
often do not generate
• the high flow rates needed for effective clearance of
secretions. Individuals with laryngeal disorders,
• including those with tracheostomies, may not achieve
sufficient laryngeal closure to generate the
• increased intrathoracic pressures necessary for an effective
cough [
DIAGNOSTIC APPROACH
• Children with chronic cough should be
evaluated with a detailed history, physical
examination, chest
• radiograph, and (if the child is able)
spirometry
• This evaluation often provides sufficient
• information to categorize the cough as specific
(ie, caused by an underlying disease) or
nonspecific
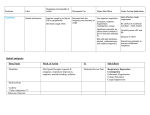
• Specific cough — The causes of specific
chronic cough fall into the following general
categories
•
•
•
•
•
•
•
•
Asthma
Persistent bacterial bronchitis
Chronic suppurative lung disease and bronchiectasis
Airway abnormality (congenital, foreign body, or
neoplastic)
Aspiration
Chronic or less common infections
Interstitial lung disease
Extrapulmonary causes: cardiac abnormalities, ear
conditions
• The sequence of evaluation for these
disorders is informed by the age and
presenting features of the
• child. Identification of the presenting features
and cough characteristics is important
because many are
• easily recognizable and strongly suggestive of
a specific cause; this is less true in adults.
• Key symptoms and signs — Certain symptoms
and signs are highly predictive of a specific
cough.
• These signs or symptoms narrow the
diagnostic possibilities and call for further
specific testing or
• referral
• Chronic wet cough
• Wheezing or crepitations
• Onset after an episode of choking, or sudden
onset while eating or playing
• Abnormal chest radiography or spirometry
• Associated cardiac or neurologic abnormalities
• Failure to thrive, feeding difficulties, or
hemoptysis
• the symptom of a chronic wet cough, with or
without production of purulent sputum, is
• always pathologic and warrants investigations
for a persistent endobronchial infection
(persistent
• bacterial bronchitis or chronic suppurative
lung disease), retained airway foreign body, or
• immunodeficiency
• Nonspecific cough — If symptoms suggesting
specific cough are absent and the chest
radiograph and
• spirometry are normal
• the possibility of asthma should be considered
and pursued with an empiric
• trial of bronchodilators and other asthma
medications
• If there is no response, the child should be
considered to have a nonspecific cough, and
the medication
• should be stopped. The child and parents
should be reassured and the patient observed
over time for
• possible emergence of specific symptoms
• HISTORY — The diagnostic approach outlined
above requires a detailed history, which should
focus on
• the following key elements
• Age and circumstances at onset — Neonatal
onset of coughing should prompt consideration
of
• congenital malformations (eg,
tracheobronchomalacia), conditions predisposing
to aspiration
• tracheoesophageal fistula, laryngeal cleft, or a
neurological disorder), or chronic pulmonary
infections
• (eg, cystic fibrosis or ciliary dyskinesia
• A cough that begins suddenly while playing or eating,
especially in the toddler age range, should raise
• suspicion of an aspirated foreign body in the airway.
The physician should specifically ask about a
• history of choking, because this may have occurred
weeks before and the family may not voluntarily
• recall the information. Even if there is no history of
choking, a foreign body remains a diagnostic
• possibility
• An episode of severe pneumonia can damage
the airways, making the child vulnerable to
chronic cough.
• More rarely, severe pneumonia may cause
frank bronchiectasis. A psychogenic or
habitual cough also
• often begins after an upper respiratory
infection.
Nature of the cough
• .
• Chronic paroxysmal cough triggered by
exercise, cold air, sleep, or allergens is
• often seen in patients with asthma.
• Barking or brassy cough suggests a process in
the trachea or more
• proximal airways, such as airway malacia,
laryngotracheobronchitis, spasmodic croup, or
foreign body
• Staccato cough in young infants can be the
result of infection with Chlamydia
trachomatis. Cough that is
• honking ("Canadian Gooselike")
• and disappears at night suggests a
psychogenic or habitual cough.
• A chronic productiv coughe
• suggests a suppurative process, and may require
further
• investigation to exclude
• Bronchiectasis
• cystic fibrosis immune deficiency, or congenital
• malformation
• active infection
• Acute or subacute paroxysmal cough suggests
infection with pertussis or parapertussis; this
characteristic
• cough can be retriggered by subsequent upper
respiratory illness
Timing and triggers
• The timing and triggers associated with cough
can help guide diagnosis
• Cough
• due to asthma typically occurs following
exposure to characteristic asthma triggers (ie,
allergens, smoke,
• exercise, cold air, or viral infection), and
typically worsens during sleep
• Cough associated with nasal
• problems typically is worst during changes of
position,
• while cough due to bronchiectasis typically is
• worst and most productive early in the day.
• Cough that is triggered during swallowing is
suggestive of aspiration, either primary or due
totracheoesophageal fistula or laryngeal
abnormalities
• Cough in the first hour after meals, or which is
• worse while supine, may reflect
gastroesophageal reflux
Associated symptoms
• A history of dyspnea or hemoptysis should trigger
a search for an underlying
• lung disease
• Hemoptysis should also raise concerns of
bronchiectasis, cavitary lung disease (tuberculosis
• or bacterial abscesses), heart failure,
hemosiderosis, neoplasm, foreign bodies,
vascular lesions, endobronchial lesions,
catamenial bleeding, and clotting disorders
• Cough, with or without symptoms of
pancreatic insufficiency, recurrent
endobronchial infection, and/or
• failure to thrive should raise suspicion of cystic
fibrosis
• Cough associated with persistent fever, and/or
• failure to thrive, or weight loss should raise
suspicion of chronic infection and immune
deficiency
• Children with neurologic impairment or
seizures frequently have chronic aspiration
• Anaphylactic reactions to food can include
cough but are unlikely to present with
recurrent cough in the
• absence of other symptoms of anaphylaxis
Past medical history
• The past medical history should include an
account of the pregnancy, labor, and
• delivery, as well as the neonatal course
• Low birth weight and/or premature neonates
are at risk for
• developing atopic sensitization and asthma.
• The past medical history should also include
questions related to eczema and pulmonary
infections. In
• preschool children, a history of infantile
eczema is often associated with inhalant
allergy
Family history
• Family history of atopy or asthma increases
the risk in offspring, and suggests a
• diagnosis of either allergic rhinitis or asthma
in the child with chronic cough
• Family history of
• cystic fibrosis or primary ciliary dyskinesia should raise
suspicion for these disorders.
• A careful history
• should be obtained for current illness in family
members or close contacts; such individuals with
cough,
• weight loss, and night sweats should arouse suspicion
of tuberculosis. In some cases, the possibility of
• HIV transmission from mother to child should be
assessed
• Social history and environmental exposures
• Passive or active exposure to smoke from tobacco
• marijuana, cocaine or other chemical irritants can
result in chronic cough
• In addition, woodburning
• stoves cause indoor air
• pollution and can predispose children to
respiratory infection s Gas stoves are also
associated with
• respiratory symptoms in children
• It is important to elicit any history of contact with
pets or other animals, as cough may be induced
by
• allergy to the animals. Similarly, the location of
the child's home and travel history may be
relevant.
• Local epidemiology can inform the diagnostic
considerations, especially with respect to
endemic fungal
• and parasitic infections
• Histoplasmosis is commonly associated with
exposure to birds and
• bats, and echinococcosis with exposure to
dogs and sheep
• Medications — Response to prior therapy may
yield some diagnostic clues regarding the
cause of
• chronic cough. Previous response to
antihistamines suggests a component of
rhinitis and postnasal drip,
• while a response to inhaled bronchodilators
suggests possible asthma.
• Any medications taken by the patient should
be reviewed carefully; angiotensin converting
enzyme
• (ACE) inhibitors are a wellestablished
• cause of chronic cough. Patients previously
treated with cytotoxic
• drugs or thoracic radiation are at risk of
interstitial lung disease.
PHYSICAL EXAMINATION
• General examination — The physical
examination should pay close attention to the
following signs of
• chronic underlying disease
• General appearance of chronic illness
• Poor growth, thinness, or obesity
• Increased work of breathing, retractions, accessory
muscle use, chest wall hyperinflation or
• deformity, abnormal breath sounds (reduced intensity,
asymmetry, wheezing, stridor, crackles)
• Shiners, swollen nasal turbinates, nasal obstruction,
nasal polyps, allergic nasal crease, halitosis,
• tonsillar hypertrophy, pharyngeal cobblestoning, high
arched or cleft palate, hoarseness
•
•
•
•
Tympanic membrane scarring or frank otorrhea
Abnormal heart sounds, abnormal pulses
Hepatoand/
or splenomegaly, abdominal masses, bloating,
rectal prolapse
• Edema of the extremities, cyanosis and/or
clubbing of the digits
• Rashes and other skin lesions (eg, scars of healed
recurrent impetigo)
Chest examination
• Polyphonic wheezing (ie, many different
pitches) with cough is typical of asthma; the
wheezing occurs
• on expiration and sometimes also on
inspiration
• Many children with asthma are also atopic
and exhibit
• signs of rhinitis, conjunctivitis, and/or eczema
• Other causes of polyphonic wheezing include
viral
• bronchiolitis, obliterative bronchiolitis,
bronchiectasis (cystic fibrosis, allergic
bronchopulmonary
• aspergillosis, primary ciliary dyskinesia),
bronchopulmonary dysplasia, heart failure,
immunodeficiency, bronchomalacia, and
aspiration syndromes.
Monophonic wheezing
• Monophonic wheezing (a single, distinct noise
of one pitch and starting and stopping at one
discrete
• time) and cough should always raise suspicion
of large airway obstruction caused by foreign
body
• aspiration or malacia and/or stenosis of the
central airways
• lymphadenopathy, and mediastinal
• tumors can cause extrinsic large airway
obstruction. Tuberculosis should always be
considered in a child
• with a monophonic wheeze, particularly in
areas where the disease is prevalent
CHEST RADIOGRAPHY
• In addition to a thorough history and physical
examination, a chest
• radiograph should be obtained. If foreign body
aspiration is suspected because of the age, clinical
• presentation or history, frontal films should be
obtained during both inspiration and expiration, to
• evaluate for unilateral lung hyperinflation that would
suggest airway obstruction. Similar information can
• be obtained from the combination of frontal, right
lateral decubitus, and left lateral decubitus
• radiograph
PULMONARY FUNCTION TESTS
• Spirometry will show signs of obstruction in
diseases that
• obstruct the airways, and restriction in
interstitial or chest wall restrictive processes.
Suboptimal effort on
• the part of the child will also result in a
restrictive picture; thus, spirometry should be
conducted by a
• technician proficient in testing children
• If an obstructive pattern is seen on the expiratory
flowvolume
• loop, the reversibility of the obstruction
• can be assessed by measuring FEV1 before and
after inhalation of a bronchodilating agent. A
positive
• response to bronchodilators establishes the
presence of airway reactivity, and is suggestive of
asthma but
• does not rule out other disorders
BRONCHOSCOPY
• The primary indication for urgent
bronchoscopy in children with chronic cough
• is for suspected foreign body aspiration.
• Bronchoscopy is also valuable in the
evaluation of suspected airway malacia,
tracheoesophageal fistula,
• or stenosis
• Patients with presumed infectious etiologies in
whom a sputum sample is not obtained or
• yields negative results can be evaluated with
flexible bronchoscopy to perform
bronchoalveolar lavage
• for bacterial, fungal, and mycobacterial cultures.
Bronchial brushings can also be taken for patients
with
• suspected ciliary dyskinesia, although nasal
brushings also may be used
OTHER TESTS
• Esophageal pH monitoring —
• Whether gastroesophageal reflux disease
(GERD) is an important cause
• of isolated chronic cough in children is
controversial. Most authorities suggest that
this is not a common
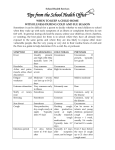
• Sinus imaging
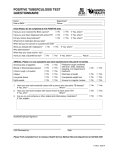
• Tuberculin testing
• Allergy testing
SUMMARY AND RECOMMENDATIONS
• There is no consensus definition of the time frame for
chronic cough in children. Chronic cough is
• often defined as a cough lasting more than four weeks,
because most acute respiratory infections in
• children resolve within this interval. Other schemes
define chronic cough as one that last more than
• eight weeks but also recognize that a relentlessly
progressive cough often warrants evaluation prior
• to eight weeks
• Chronic cough can be a symptom of congenital
anomalies, genetic disease, airway
obstruction,
• infection, airway inflammation without
infection (as in asthma), neoplasia, or
psychogenic
• processes
• The evaluation of a child with chronic cough
should include a detailed history, physical
• examination, chest radiograph, and
spirometry (when possible
• Symptoms and signs that are highly predictive of
a specific cough include chronic wet cough,
• wheezing or crepitations, onset after a choking
episode, abnormal chest radiography or
spirometry,
• associated cardiac or neurologic abnormalities,
and failure to thrive, feeding difficulties, or
• hemoptysis. These signs or symptoms narrow the
diagnostic possibilities and call for further
• specific testing or referral
• The symptom of a chronic wet cough in a
young child, usually indicates persistent
bacterial
• sinusitis or retained foreign body
شكرا •