* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Role of Gluten Peptides
Periodontal disease wikipedia , lookup
Molecular mimicry wikipedia , lookup
Ulcerative colitis wikipedia , lookup
Rheumatic fever wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Psychoneuroimmunology wikipedia , lookup
Infection control wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Kawasaki disease wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Behçet's disease wikipedia , lookup
Schistosomiasis wikipedia , lookup
Human leukocyte antigen wikipedia , lookup
Globalization and disease wikipedia , lookup
Germ theory of disease wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Inflammatory bowel disease wikipedia , lookup
Ankylosing spondylitis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Rheumatoid arthritis wikipedia , lookup
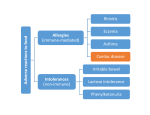
Coeliac Disease Jaide Brown Breea Buckley Krissy Rowe What is Coeliac Disease (CD)? • An immune-mediated disease triggered by glutencontaining grains • Presents in 2 forms – Typical CD – Atypical CD What is Gluten? • A protein found in the endosperm of seeds – Wheat’s gliadin and glutenin – Barley’s hordeins – Rye’s secalins • Responsible for the elastic texture of bread http://www.jci.org/articles/view/30253/figure/2 What are the Forms and Associated Symptoms of CD? • Typical CD – – – – Chronic Diarrhea/Constipation Abdominal pain, gas and distension Anemia Weight loss/malnutrition http://www.nature.com/nrgastro/journal/v6/n1/full/ncpgasthep1298.htm What are the Forms and Associated Symptoms of CD? • Atypical CD – – – – Bone/Joint Pain Delayed Puberty or Infertility Fatigue Tingling/Numbness in Extremities These cases are very rare What are the Forms and Associated Symptoms of CD? CD may be asymptomatic • If untreated can lead to; – Vitamin and iron deficiencies, osteoporosis, pancreatic insufficiencies, intestinal lymphomas or other GI Cancers Epidemiology • Affects ~1% of US population – Potentially affects a higher percentage – Many individuals go undiagnosed • RISK FACTORS – Genetic • Intestinal permeability, MHC – TGase enzyme – Enteric Infection – Co-morbidity with other autoimmune disease CD OVERVIEW http://www.jci.org/articles/view/30253/figure/2 What is the Immunological Mechanism of CD? Role of Gluten Peptides: • Gluten peptides are not easily digest by gastric, pancreatic or brush border enzymes – High concentration of proline and glutamine amino acids • Accumulation of large gluten peptide fragments – Some may be involved in the immune response Associated Risk Factors/Triggers • • Consumption of Gluten Intestinal Permeability (Genetics) Accumulation is not enough to develop CD Healthy vs. afflicted individuals show no difference in ability to digest these large peptides What is MHC’s Role in Developing CD? MHC-II alleles – HLA-DQ locus • HLA-DQ2 = 90-95% of CD cases • HLA-DQ8 = 5-10% of CD cases What is it about these alleles that increases the risk for CD? – APCs with HLA-DQ2 and HLA-DQ8 MHC-II can bind “gluten” peptides Associated Risk Factors/Triggers MHC-II Genetics HLA-DQ and HLA-DQ8 haplotypes can bind gluten These binding grooves favor negatively charged residues Not naturally found within lumen What is the Role of TGase in Development of CD? What is TGase? • Transglutaminase enzyme • Involved in tissue repair by crosslinking peptides Its Role? • Under certain conditions (low pH) TGase will deaminate glutamine to form negatively charged glutamic acid DEAMINATION L-Glutamine Glutamic Acid Associated Risk Factors/Triggers Release of TGase into the mucosal layer when gluten peptides are present Activation of CD4+ T cells • HLA-DQ2 and HLA-DQ8 restricted T cells interact with APCs and become activated • Activated CD4+ T cells secrete cytokines – IFN-γ (Interferon-gamma) • Associated with a TH1 immune response • Intracellular pathogen/autoimmunity – Associated with initiation of mucosal damage – Neutralization shown to prevent gluten-induced damage Why so rare? • 40% of population has HLA-DQ2 and HLA-DQ8 antigens Enteric Infection Role: – DQ2 and DQ8 MHC is poorly expressed in normal mucosa – TGase enzyme is poorly expressed in normal mucosa – Enteric viral infection up-regulates production of HLA antigens and cytokine production • Cytokines cause inflammation/tissue damage • Release of TGase enzyme leads to deamination The Big Picture: Who Should Be Tested? • 1st and 2nd degree relatives of CD patients • Relatives of patients and patients with Type-I diabetes • Individuals with Sjögren/Down/Turner Syndrome • People with immune, thyroid, and liver disorders How to Diagnose? • Serology – IgA • Endoscopy/Biopsy – Small Intestine • HLA – Absence of HLA-DQ2 or HLA-DQ8 Treatment • Gluten-free diet • Current research focuses on: – – – – Genetically detoxified grains Celiac vaccines (oral or intranasal) Inhibitors of TGase Inhibitors of effects of zoulin on intestinal permeability References Ahn R, Ding YC, Fasano A, Green PHR, Murray J, Neuhausen S, Garner C. 2012. Association Analysis of the Extended MHC Region in Celiac Disease Implicates Multiple Independent Susceptibility Loci. PLoS One 7(5): e36926. Carlo C, Fasano A. 2001. Current Approaches to Diagnosis and Treatment of Celiac Disease: An Evolving Spectrum. Gastroenterology 120: 636-651. Evans KE, Sanders DS. 2012. Celiac Disease. Gastroenterology clinics of North America. 41(3): 639-650. Kagnoff MF. 2007. Celiac Disease: Pathogenesis of a Model Immunogenetic Disease. The Journal of Clinical Investigation. 117(1): 41-49. Pietzak MM. 2005. Follow-up of Patients with Celiac Disease: Achieving Compliance with Treatment. Gastroenterology 128: S135-S141. Walker MM, Murray JA. 2011. An update in the diagnosis of coeliac disease. Histopathology. 59: 166-179. Questions For You! 1.Celiac disease is caused by... A.A specific allele that is present in all cases of Celiac Disease. B.Increased intestinal permeability. C.A viral infection that leads to inflammation. D.A variety of factors contribute to the onset of Celiac Disease including specific genotypes of MHC, genes involved in permeability of mucosa, and other genetic factors. Questions For You! 2. A woman is suspected of having coeliac disease; she undergoes an HLA test and an endoscopy. Which scenario most points to a diagnosis of coeliac disease? A) B) C) D) E) Negative HLA test, positive for villous atrophy Positive HLA test, negative for villous atrophy Positive HLA test, positive for villous atrophy Negative HLA test, negative for villous atrophy Both A and D Questions For You! 3.What is “gluten” A.A brush-border enzyme responsible for digesting cereal grains within the small intestine B.B)A generic term referring to proteins found in the endosperm of wheat, barley, and rye grains C.C)An enzyme responsible for deaminating glutamine to produce glutamic acid D.D)None of the above Questions For You! 4. An enteric infection leads to an increased risk of developing CD by… A.Upregulating MHC expression and cytokine production which results in inflammation and intestinal damage B.Overwhelming the immune system so it cannot combat both the viral infection and accumulation of gluten peptides C.Forming complexes of pathogenic toxins and gluten peptide fragments which cause intestinal inflammation and damage D.All of the above Questions For You! 5. Name 2 risk factors/triggers and give a brief explanation of how they contribute to the development of CD