* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Virulence Mechanisms in Tuberculosis
Community fingerprinting wikipedia , lookup
Human microbiota wikipedia , lookup
Marine microorganism wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Magnetotactic bacteria wikipedia , lookup
Triclocarban wikipedia , lookup
Tuberculosis wikipedia , lookup
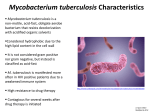
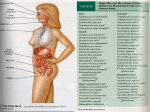
Virulence Mechanisms in Tuberculosis Priscille BRODIN Institut Pasteur Korea, Inserm Avenir, Seoul, Korea I will discuss what is currently known about the virulence mechanisms in tuberculosis. I. Definition of Mycobacterium Tuberculosis Virulence 1. The Etiological Agent Mycobacterium tuberculosis is caused by a mycobacteria belonging to the mycobacterium genus, which comprises over 17,000 different strains. M. tuberculosis agent can be stained with a specific method, the Ziehl Neelsen method, due to the rich composition of its cell-wall in mycolic acids and glycolipids. Working with mycobacteria is considered rather difficult, due to their slow replication time approximately one day. In addition, mycobacteria are highly infectious, so researchers are obliged to work in Class III biosafety laboratories. 2. Disease Process When a patient is infected with M. tuberculosis, the bacilli reach the alveoli and infect the alveolar macrophages in the lungs. At this stage, it is considered an intracellular bacillus, since it is located within the host cell. The next stage is the latency stage, and in approximately 10% of the cases, the tuberculosis disease is developed. A critical feature of the latency stage is granuloma formation, with the presence of giant cells. This leads to caseous necrosis and the release of bacilli, which can then be transmitted to new patients and infect them. At this stage, the bacilli are referred to as extracellular bacilli, and their condition is anaerobic. Then, is some cases, calcification occurs, while in others, dissemination takes place, with miliary tuberculosis or meningitis. 3. Defining Virulence I believe virulence is slightly different than resistance. I would define virulence as the ability of a microbe to cause disease in a host. It can also be defined as the degree of pathogenicity of a microbe. Thus, virulence is always related to a host body or cell. Virulence is caused by several factors that are encoded by the bacteria. There are then several different ways by which the bacteria can cause the disease. First, the virulence factors can induce cell adhesion to the host cell. Second, they can increase the colonisation of the host body and the persistence. Third, they can favour invasion into host cells. Fourth, the bacteria can express inhibitors of the immune response. Fifth, some bacteria can express toxins. It has often been noted that there are no classical bacterial virulence factors for M. tuberculosis. That is, no toxin has been identified, and there is no pathogenicity island in the genome. Thus, although there are numerous putative virulence factors, we must admit that our knowledge is still limited. 4. Models for Measuring Virulence Nevertheless, TB virulence can be quantified, with the help of two models: the animal model and the cellular model. The animal model utilises mice, guinea pigs, and non-human primates. Typically, the animals are infected either via the aerosol route, or intranasally, like the natural infection. The animals usually receive 100 CFU ((colony forming unit, or number of living bacteria) at day zero. Then, typically, following a month, there is a 3 log increase of the CFU. Then, the number of bacteria remains constant for two or three months. a. The Mouse Model There are typically two target organs in the mouse model - the lungs and the spleen. In parallel to examining the CFU, we also examine the lesion, to determine the severity of the strain. The parameters associated with virulence in the mouse model are colonization, persistence, and pathogenicity. These depend on the route of entry and the infecting dose, and we also examine morbidity and mortality. One the host side, it is possible to examine immunity. b. The Cellular Model The second model used to quantify virulence is the cellular model. Mycobacteria can infect the macrophages cells and dendritic cells, and can also enter the pneumocytes and adipocytes cells. The first feature we examine is invasion survival replication. Today, it is possible to follow the growth and spread of mycobacteria within the cells using automated fluorescent microscopy. We are thus able to quantify the bacterial burden, and obtain a precise measure of the invasion parameters, survival and multiplication inside the cells. This method can currently be applied to several hundreds of strains. A second feature we examine inside the cells is trafficking. The bacterium has the ability to block phagosome maturation. One of the critical features of mycobacteria is that they reside in endosomes that cannot be acidified into lysosomes. While we still do not understand the factors responsible for this phenomena, we estimate that it helps the bacteria survive and multiply within the cells. Examining cellular models also allows to study the cytokines release and profile. For example, it is possible to examine the release of TNFα, IL-2, IL-12, and IFNγ. II. Features of M. Tuberculosis The features of M. tuberculosis can be examined using a phylogenetic tree, based on 16S rRNA, hsp65, sodA, and rpoB sequences. In mycobacterial terminology, bacteria are divided into slow-growing and fast-growing types. M. tuberculosis, which is a slow-growing bacteria, belongs to the tuberculosis complex. It is striking that the Identity in nucleotidic sequence of the species in this complex is greater than 99.9%. Other slow-growing mycobacterium bacteria include the M. marinum and M. ulcerans. The latter are causing the Buruli ulcer, which is an emerging disease caused by mycobacteria, and is found mostly in Africa. 1. The M. Tuberculosis Complex The M. tuberculosis complex consists of six members. One is of course M. tuberculosis, which is the main agent in human TB. The other five are Mycobacterium africanum, bovis, canettii, pinnipedii and microti. The tropism of the different species varies. They each come from isolates, from some of which vaccines were developed. The most popular strain used in the laboratory is H37Rv, from which the H37Ra vaccine is derived, similarly to the way BCG has been obtained from passage of M. bovis. Currently, significant work is being conducted on the W-Beijing strain family, and particularly on the GC1237 isolate. M. bovis has the largest tropism, and can infect most mammals. It used to cause TB in humans, but more rarely, and all the BCG strains were derived from it. M. pinnipedii was shown to cause disease in Seals in Australia. I would like to briefly discuss M. microti. It was isolated in England in the 1930s among the population of small rodents called voles, which exhibited a disease similar to tuberculosis. More recently, human patients with active tuberculosis were diagnosed as infected with the M. microti. M. microti OV254 is a naturally attenuated strain, and its derivatives have been used in Czechoslovakia as a vaccine in the 1960s, instead of BCG. In conclusion, since the different isolates of M. tuberculosis differ in tropism and virulence, it follows that these strains must encode virulence factors. 2. Mycobacterium Specific Features: Cell Envelope One of the specific features of the M. tuberculosis is its cell envelope. On the membrane, there is arabinoglactan on top of the peptidoglycan, and then mycolic acid. There are also some Phenolic Glycolipid (PGL), and Lipoarabinomannan (LAM). It was recently shown that PGL seems to be reproduced by the Beijing strain, and can account for the increased virulence of the strain. LAM is an immunomodulator. 3. The TB Genome The first sequence of the TB genome, the H37Rv strain, was obtained 10 years ago. It is comprised of one circular chromosome, of 4.4 Mb, which contains about 4,000 genes. No extrachromosomic DNA has been found in this strain. The M. tuberculosis genome includes all the genes that enable the bacteria to survive in aerobic, microaerophilic, and anaerobic conditions. In comparison to other bacteria, it has a complex regulatory potential. It includes 13 sigma factors, 11 two-component systems, and histidine kinase factors. It was also striking to discover 11 Serine Threonine Protein Kinases in the TB genome. These kinases are one of the preferred targets of the pharmaceutical industry when looking for new drugs. The TB genome also includes a large number of genes involved in lipid metabolism, which is required for the metabolism of the cell wall. It also includes some degradative enzymes, such as 20 cytochrome P- 450, as well as many insertion elements, such as IS6110, which are the basis of genotyping. Another striking discovery was the presence of large gene families. There are about 160 members of the PE/PPE family in the genome, but we are not sure yet what their function is. Other families include mce, mmpL, and ESAT-6. Again, no toxin has been found, nor any obvious pathogenicity island, and merely a few classical virulence genes. 4. Summary To summarise, virulence in tuberculosis is different from that of classical bacteria. Although the major virulence factors remain to be identified, robust cellular and animal models allow to measure the virulence. According to clinical data, the M. tuberculosis strains and the clinical isolates exhibit significant virulence differences, so much can still be learned. Finally, there are many putative candidates arising from biochemical and genome global analyses. III. Approaches for Identifying TB Virulence Mechanisms For the past ten years, many laboratories have attempted to identify virulence mechanisms. Their approaches can be roughly classified into four major groups. 1. Strain Comparison: Comparative Genomics The first approach is comparative genomics. This method is to compare the genome content of virulent and non-virulent strains. This task requires an available sequence, typically of the virulent kind. We use the M. tuberculosis H37Rv sequence. Then, we use an attenuated or vaccine strain that is extremely similar genetically, such as M. bovis BCG or M. microti OV254. We also require genomics, genetic, and DNA based tools, such as Bacterial Artificial Chromosomes (BAC) libraries, microarrays and bioinformatics. Let us examine the differences between the genomes. First, we consider the Single Nucleotide Polymorphism (SNP), which is a single nucleotide that is mutated from one strain to another. 2,000 mutations were found between the two TB sequenced strains, H37Rv and CDC1551. Most of these mutations have no significant effect. A feature that is specific for TB is the regions of difference (RD regions). These regions correspond to a piece of DNA that has been lost from one strain to the other. The regions are numbered from RD1 to RD26. Then, the opposite phenomenon has been discovered: a complementary piece of DNA that was present in the attenuated strain, but absent in the virulent strains. These regions are called RvD regions. A third region, TbD, designates DNA that is absent in the tuberculosis strains. A famous example is TbD1, which is a piece of DNA that is absent in most of the strains, but still found in Indian strains. Once we have identified the genes that have been lost during attenuation, our goal was to discover what these genes encode. To achieve that goal, we required functional genomics. However, first, it was necessary to extend the study to multiple strains, in order to select the relevant regions for virulence. For that purpose, we have used internally controlled PCR amplification. We used two set of primers. The first set was an internal primer, which amplified a product within the RD region. The second set was a flanking primer, which provides a product merely when the region was lost. The aim of the PCR amplification was to determine, in many strains, whether a certain region is present or absent. We also used focused macro-arrays. These are basically membranes that have been spotted by different probes, corresponding to different genes from the TB genome, particularly from the RD regions. The technique is used to study a couple of hundreds of strains. I will now briefly describe how we demonstrated that RD1 was absent in M. microti. The RD1 region is displayed, and it encodes two secreted proteins, CFP10 and ESAT-6. ESAT-6, which is the basis of the new diagnostic method QuantiFERON, is a strong T-cell antigen. However, we still do not know its function at the cellular level. We obtained genomic DNA from different species of the tuberculosis complex. Then, we transferred the DNA into a membrane, and hybridised it with a probe that was generated with an ESAT-6 primer. We have obtained a product for the M. bovis, M. canettii and Rv stains, thereby demonstrating that ESAT-6 was indeed present in this genome. On the other hand, we did not obtain a product with BCG or with an entire set of M. microti isolates. As a confirmation, we used a RD1 probe, which also provided evidence of the RD1 division. We have demonstrated that the RD1 division was not the same in M. microti and BCG. Further, the findings might suggest that the RDI region could play an important role in virulence. Since, as I have noted, M. microti and BCG are the only two members of the tuberculosis complex that are non-virulent in humans. We conducted this study with all the members of the TB complex, to see what DNA regions have been lost by each species. The largest number of lost regions occurred in BCG and M. microti. Our goal was to find the region that has been lost in all the attenuated strains, but is still present in all the virulent ones. We discovered only one such region - RD1. RD1 is absent from the BCG and M. microti strains, but present in the human infectious strains. In order to determine whether the RD1 region is involved in virulence, we over-expressed the region within the BCG. For that purpose, we used the integrative cosmid tool, which allows the expression of a large DNA fragment inside the genome. We called the strain obtained BCG:RD1; that is, a BCG strain that expresses the entire RD1 region. Strikingly, we observed a difference in the morphology of the colony. We conducted the same experience with M. microti, to ensure that it was not a unique feature of BCG, and we observed the same phenomenon. Then, we infected mice with the BCG and BCG:RD1 strains, and examined the growth of the CFU in the lungs. We discovered that the BCG strain did not continue to grow, while the BCG:RD1 did. In addition, we found some lesion present in the BCG:RD1 stain, as well as a clear expression of the antigen ESAT-6. Since the increased bacterial burden and lesion formation is a correlate of virulence, we concluded that RD1 is a virulence factor. Furthermore, in a study conducted by W.R JACOBS et al, the RD1 strain has been removed from the RD region of the Rv strains. The researchers have found a significant decrease in the number of bacteria. The same decrease has been achieved by removing the ESAT6. It was therefore rapidly confirmed that the major virulence factor in the RD1 region is ESAT6. However, it is important to remember that when RD1 is added to the BCG strain, the result is not TB, and when it is deleted from the TB strains, the result is not BCG. Thus, RD1 is merely one of the virulence factors. 2. The Genetic Mutant Approach The first step of the genetic mutant approach is to formulate an hypothesis. Then, we create a mutant of the wild type strain, through a gene knock-out process. The deletion is performed either through allelic exchange or transposon insertion. The gene or the operon is not transcribed, and the protein is not synthesised. We thus obtain a genetic KO-mutant. Let us examine the isocitrate lyase (icl) example. Our initial observation was that isocitrate lyase activity increases when M. tuberculosis infects macrophages. Thus, it was reasonable to assume that it plays is an important role in macrophage replication. We thus isolated the wild type strain sequence from the genome analysis, and obtain a knock-out mutant, Δicl, in which an antibiotic marker replaced the icl gene. Then, we infected mice either with the wild type strain or the knock-out mutant. We observed that the growth of the two strains was identical during the first three weeks. However, then, the number of bacteria in the lungs of the icl mutant has decreased, while the number bacteria in the wild type strain remained unchanged. A survival study revealed that while 100% of the mutant mice survived until the end of the 24 week experiment period, all the mice infected with the wild type strains died within 16 weeks. These results led us to the conclusion that the icl gene is involved in persistence in mice, which is a virulence parameter. However, we wanted to confirm that the deleted gene is indeed responsible for the effect observed, and that it is not due to a side effect. We have therefore decided to add back the gene that we have omitted to the KO mutant. This has been achieved through insertion. Since the virulence has been restored when the gene was restored, we were provided with definite proof that the gene studied is indeed a virulence factor. 3. The Large Mutant Pool Approach Several laboratories have adopted the large mutant pool approach. It utilises a transposon mutant library, which is a pool of different genetically modified bacteria. Each bacteria mutant has one gene that has been inactivated through a transposon insertion. Thus, we obtain a mixture of bacteria that have different inactivated genes. Considering that the TB genome includes 4,000 genes, In a 100,000-member library, there are approximately 25 mutants for each gene. A study conducted by RUBIN et al examined genes that are essential for growth inside the mice. The researchers thus injected the pool of mutants into the mice, waited for a few weeks, extracted the target organs, and then recovered the bacteria. They then decided to compare the diversity of the output and input pools. If the genes that played an important role in growth inside the mice have indeed been deleted, they would not be found in the output pool. Using DNA PCR, labelling, and hybridisation to a genomic microarray, they managed to identify and compare the diversity of the bacteria responsible for growth in-vivo. The same experiment was conducted in-vitro, and the authors compiled a list of 194 genes that are necessary for growth in-vivo. The same approach was adopted in several studies focusing on macrophages over the past few years. While these studies do provide insight into virulence factors, they still require validation with individual mutants, as well as modelisation of molecular mechanisms. 4. Global Gene Expression Analysis The global gene expression analysis approach utilises regular tuberculosis or BCG strains instead of mutants. The element that is being modified is the model. While it is still possible to use mice, it is also possible to use in-vitro models, which are believed to mimic the in-vivo conditions of the persistent bacteria. Thus, it is possible to compare the bacteria state in anaerobic and aerobic conditions, when the bacteria are in nutrient starvation, or in different persistence models. For that purpose, it is possible to use postgenomics techniques, such as Transcriptomics, Proteomics and Lipidomics. These techniques enable us to search for the genes or proteins that are over-expressed in one condition, in order to compare them with another condition. Once again, we managed to obtain a list of genes that we believe are encoding putative virulence factors. In some studies, the analyses of the bacteria and the host factors have been conducted in parallel. These findings also require confirmation through genetic mutant studies. IV. M. Tuberculosis Virulence Factors I would like to provide a slightly more detailed description of the tuberculosis virulence factors, which I roughly classify into four categories. 1. Secreted Factors The first category is secreted factors, which are products that are exported outside the bacteria. They include culture filtrate proteins, such as HspX, Esat6/CFP-10, and 19-kD. These proteins have been studied thoroughly, due to their potential for vaccine and diagnostic applications. More recently, the protein Kinase G was shown to be involved in phagosome maturation arrest. 2. Cell Surface Components The cell surface components include proteins involved in synthesis of the cell wall. Among them, I would like to emphasise the LAM, which has multiple functions. First, it is an immunomudulator. In addition, it has been shown that LAM is able to inhibit the release of calcium. 3. Enzymes Involved in Metabolism The third category includes enzymes involved in general or cellular metabolism. Some of these enzymes are involved in lipid and fatty acid metabolism, which allows bacteria to grow on fatty acids. It was also discovered that when introducing knock-out mutants to the amino acid and purine biosynthesis pathway, then the bacteria has a different phenotype in virulence. A similar phenomenon was observed when disrupting the genes involved in metal uptake, as well as factors involved in anaerobic respiration and oxidative stress proteins. 4. Transcriptional Regulators The final category of virulence factors includes the transcriptional regulators. Following the systematic knock-out of all the sigma factors, four have been found to account for change in virulence in the mouse model. The PhoP/PhoR response regulatory is also an important virulence factor, and a knock-out mutant of PhoP/PhoR is considered a promising vaccine candidate. 5. Summary To summarise this section, numerous focused and global approaches have been undertaken to identify M. tuberculosis virulence factors. We have obtained long lists of genes, which I believe require further confirmation and investigation. Finally, the genes encoding virulence factors belong to different functional classes: secreted factors, cell surface components, metabolism enzymes, and transcriptional regulators I. Conclusions for Future Research I would like to offer several recommendations for future research. first, I believe it is necessary to increase the comparison of whole genome sequences from clinical isolates. Since it is easier to sequence a genome today, we should be able to learn more about the clinical isolates. Concerning the pooled screens, I believe it would be useful to investigate in different genetic backgrounds, such as an immuno-deficient background, or different animal models. When we study mutants in the animal model, it would be useful to be able to turn the gene expression ‘on’ or ‘off’. Therefore, inducible promoters that can be turned on in-vivo would be extremely helpful for determining in which part of the replication process of the bacteria the gene plays an important role in the animal model. Finally, we must remember that tuberculosis is a human infection. For that reason, we could greatly benefit from a global transcriptional and proteomics analysis of human infections. I. Question and Answer Session Ying ZHANG What is the size of the RD1 deletion in the microtic strain vs. the BCG strain? Do you know what causes the deletion? Pricille BRODIN The deletions are roughly the same size. However, in the microtic strain it is shifted from Rv3864 to Rv3876, whereas in the BCG1 it is shifted from Rv3871 to Rv3879. We do not know what causes the deletion; it is simply a loss of DNA that is being cut within the gene. When we compared the microti OV strains that were isolated in the 1930s with the microti isolates that were found in human TB patients, and we found exactly the same deletion. However, some microti isolates, which have been isolated in 1995 do not have the RD1 region, and are still considered as agents responsible for TB in humans. In this case, RD1 is not the virulent factor. Steffen STENGER What do you know about the immunology of the Mycobacterium microti, compared to other mycobacterium in the M. tuberculosis complex? It seems peculiar that organisms that are 99.9% identical on the genetic level would be so different in terms of the clinical disease. Pricille BRODIN We know that M. microti grows even slower than TB or BCG. Thus, it takes four weeks to obtain a colony on a plate, and eight weeks to obtain a clinical strain. OV254 is the model strain with which we have conducted all the investigations on the RD1. Generally, we did not find any difference between OV254 and BCG, besides the fact that the CFU grew somewhat slower. However, when we infected a mouse with the clinical isolate of microti, the bacteria grew significantly faster than on the plate, and killed the mouse.