* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Choroidal Neovascular Membrane Mimicking a Branch Retinal Vein
Survey
Document related concepts
Transcript
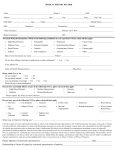
Choroidal Neovascular Membrane Mimicking a Branch Retinal Vein Occlusion Resident’s Day Case Report Lindsey M. Jendrasko, OD Optometry Resident, VA Togus [email protected] Abstract Idiopathic CNVM can mimic other retinal diseases including BRVO. OCT can miss early cases, while FA is a more reliable test for definitive diagnosis. I. Case History - - 61 year old Caucasian male Chief Complaint Black spot in center of vision, right eye only, for past two months. Noted wavy lines when looking at roofs. Condition constant and relatively stable since onset. - Ocular History - Medical History - No history of eye exam. Coronary Artery Disease Hyperlipidemia Congestive Heart Failure Esophageal Reflux Paroxysmal Ventricular Tachycardia Smoker Medications Carvedilol Clotrimazole Lisinopril Omeprazole Rosuvastatin Vitamin C Aspirin 325 mg Ezetimibe/Simvastatin Omega 3 Acid Vitamin E II. Pertinent Findings - Initial Exam VA sc OD: 20/30-1 PH 20/20-2 OS: 20/25-1 PH 20/20 Amsler Grid OD: Superior Distortion OS: Normal Dilated Fundus Exam OD: cluster of blot hemorrhages and swelling following distribution of retinal venule OS: Normal ocular health Macular OCT OD: Central Thickness 282, intraretinal thickening inferior temporal to macula OS: Central Thickness 234, normal foveal contour OD OD OS OD - Differential Diagnosis - Impression - Following consult with ophthalmology, patient asked to: 1. Return in one month. 2. Begin home Amsler Grid. 3. In case of deterioration, Anti-VEGF was planned. Two Week Follow-Up- An Early Return OD Branch Retinal Vein Occlusion Plan - Branch Retinal Vein Occlusion (BRVO) Risk factor of coronary artery disease Intraretinal hemorrhages and macular edema consistent with typical presentation Juxtafoveal Retinal Telangietctasia (JFRT) Age and sex of patient consistent with unilateral, idiopathic presentation that JFRT can exhibit Often presents with exudates which are not present in this patient. Diabetic Retinopathy (DR) Blot hemorrhages and macular edema consistent with DR Medical record showed regular care and labs were not indicative of diabetes Choroidal Neovascular Membrane (CNVM) Age of patient appropriate for suspicion of CNVM due to macular degeneration No drusen or pigmentary changes in either eye. Patient returned two weeks early with worsening vision and increased Amsler Grid distortion in the right eye. Best corrected visual acuity worsened in the right eye to 20/40Dilated Fundus Exam OD: Cluster of hemorrhages, 1DD of edema inferior to macula. Also noted: a grey-green appearance in the edematous area. Macular OCT OD: Central thickness 372 microns, change analysis of +90 microns, thickening with disruption and elevation at level of RPE/choroid OS: Central thickness 230 microns, stable & normal OS OD Fluorescein Angiography (FA) - OD: Early, well-defined hyperfluorescence consistent with a classic choroidal neovascular membrane OS: Normal OD III. Differential Diagnosis: Causes of CNVM Age-Related Macular Degeneration Age and smoking status of patient suggestive No drusen or RPE disruption in diseased or fellow eye. Myopic Degeneration Patient is not myopic. Angioid Streaks None present. Trauma No history of trauma. Inflammation (such as Presumed Ocular Histoplasmosis Syndrome) No signs of ocular inflammation No risk factors in medical history for inflammatory disease. IV. Diagnosis and Discussion V. Final Diagnosis: Idiopathic Choroidal Neovascular Membrane No associated signs suggesting underlying disease process. OCT failed to show the lesion early on, but later did at follow-up. The diagnosis was then confirmed with a fluorescein angiogram. Variability exists in the literature regarding the detection of subtle OCT changes in chorioretinal disease9. Some report morphologic changes on OCT precede subjective and functional changes8, while others cite discrepancies between FA and OCT in the detection of macular disease. It has been suggested that a retinal vein occlusion could preclude the development of a CNVM 1, but this does not seem likely in this case. The lack of collateral vessel formation does not point to a causal relationship. If this was the case, it would likely occur more frequently in ischemia from diabetic retinopathy and retinal vein occlusion, which are the two leading causes of retinal vascular disease in the United States1,2. Treatment & Management Following the FA, a treatment series of three intravitreal Lucentis injections was initiated. The patient will return in 1 month for the second injection. Anti-VEGF therapy has been successfully used in the treatment of neovascular AMD, proliferative diabetic retinopathy, retinal vein occlusion, diabetic macular edema and retinopathy of prematurity2,7. Large clinical trials investigating anti-VEGF for idiopathic CNVM have not been performed, but several smaller studies suggest it is beneficial, safe and well tolerated for CNVM secondary to non-AMD causes3,4,5,6. VI. Conclusion CNVM, especially idiopathic, can mimic a BRVO. Even in the absence of associated signs and risk factors, CNVM must remain a top differential diagnosis in cases of macular edema with intraretinal hemorrhaging. o OCT provides limited information in the early detection of choroidal changes, and fluorescein angiography remains an important diagnostic indicator in chorioretinal disease of unclear etiology. o Home Amsler Grids can detect subtle changes and facilitate earlier diagnosis and treatment. o Lastly, anti-VEGF has become the standard treatment for chorioretinal diseases involving the macula. o VII. Bibliography 1. Fea, Antonio et al. Subfoveal choroidal neovascularization in a patient with hemicentral vein occlusion. Int Ophthalmol 2010; 2=30: 207-210. 2. Channa, R, et al. “Treatment of macular edema due to retinal vein occlusions.” Clinical Ophthalmology 2011:5 705-713 3. Ciulla, Thomas A. et al. Anit-Vascular endothelial growth factor therapy for neovascular ocular diseases other than age-related macular degeneration. Curr Opin Opthalmol 20: 166-174. 4. Mandal, Subrata, et al. Intravitreal Bevacizumab for Subfoveal Idiopathic Choroidal Neovascularization. Arch Ophthalmol. 2007; 125 (11): 1487-1492 5. Chang, Louis K, et al. Bevacizumab Treatment for Subfoveal Choroidal Neovascularization From Causes Other Than Age-Related Macular Degeneration. Arch Ophthalmol. 2008; 126(7):941-945 6. Carneiro, Angela, et al. Ranibizumab Treatment for Choroidal Neovascularization from Causes Other than Age-Related Macular Degeneration and Pathological Myopia. Ophthalmologica 2011; 225: 81-88 7. Campochiaro, PA, et al. “Ranibizumab for Macular Edema following Branch Retinal Vein Occlusion.” Ophthalmology 2010; 117 (6): 1102-1112 8. Hoerster, R, et al. “Subjective and functional deterioration in recurrences of neovascular AMD are often preceded by morphologic changes in optic coherence tomography.” Br J Ophthalmol (2011) doi:10.1136/bjo.2010.201129 9. Kozak, I, et al. Discrepancy between fluorescein angiography and optical coherence tomography in detection of macular disease.” Retina. 2008 April; 28(4):538-544