* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Advances in Implants
Survey
Document related concepts
Transcript
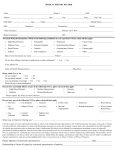
The Advances and Challenges in Ocular Drug EFFECT OF ENVIRONMENT AND CLOZAPINE ON BASAL AND STIMULATED MEDIAL PREFRONTAL GABA RELEASE IN TWO Delivery via Implantation Techniques RAT MODELS OF SCHIZOPHRENIA Adedoyin Awodele, Faye Carrington, Alanna Cavanagh, Constance Gaya Cremers, Sarah Kileen, Melissa MacPherson.. Pharmacology, UCD School of Biomolecular and Biomedical Science, University College Dublin, Ireland. Introduction Why Implants? •Provide sustained drug delivery to the posterior or anterior segment of the eye •Can be applied to various ocular layer depending on disease: subconjuctival/intravitreal/intrasceral •Implants reduce frequency of administration compared to I.V. Route in relation to treating diseases of the posterior segment, therefore they reduce risk of SEs Above: Insertion of Retisert •Minimise the importance of patient compliance. •Drug can be removed should toxicity occur. Ocular drug barriers: Dynamic: Static: •Tear Dilution- max. only 30µl tear volume comfortably accomm. In eye when the average eye drop is 50 µl in volume – inevitable spillage! •Naso-lacrimal duct- when tears exceed normal tear volume of 7-10 µl •Systemic Removal – the conjunctiva is highly vascularised and any drug permeating it is rapidly removed by the systemic circulation and eventually transported to the GIT. •Cornea-Hydrophobic and hydrophilic layers connected by tight junctions and containing efflux pumps inducing multidrug resistance. (p-glycoprotein and MRP) •Sclera-Opaque matrix of proteoglycans and collagen that acts as a filter with preferred permeability for small, hydrophilic and positively charged molecules due to it’s structure. •Blood-Ocular Barriers –the blood-retinal barrier arises from the retinal pigment epithelium prevents transfer of molecules between itself and choroidal blood with tight junctions and according to some studies show P-gp efflux pumps present also. Diseases of the Eye •Age-related Macular Degeneration (AMD) : Damage to retina by accumulation of drusen can cause loss of central vision. •Diabetic Retinopathy is a type of retinal damage that can lead to blindness caused by microvascular changes due to diabetes mellitus. •Diabetic Macular Edema (DME) is the most common cause of visual loss and is characterised by accumulation of extracellular fluid in the macular which occurs after the break down of the blood-retinal barrier due to dilated hyper-capillaries and microaneurysms.. •Glaucoma is caused by damage to the optic nerve by loss of retinal ganglion cells and increased fluid pressure in the eye. What are they? •.Usually made of polymers that release a drug over a prolonged period of time. There are two types: Implant Type: Biodegradable NonBiodegradable Pros: Cons: No need for surgical removal. Can be fashioned into various shapes. Increase halflife of drug. Drug release can be controlled more precisely and for longer periods of time (years.) Control of drug release from degradable systems is more difficult. Must be surgically removed. Larger Incisions required for insertion. Non-Biodegradable Retisert Silicone cup Top View containing drug Release orifice •0.59mg tablet is held in a silicone elastomer cup. •The release orifice is separated from the drug by a PVA membrane. •The structure is held together with silicone glue 3mm Side View 2mm 5mm PVA structure tab •CMV Retinitis is a chronic, infection of the retina caused by the cytomegalovirus. Predominantly affects immunosuppressed individuals and estimated to affect 1540% of AIDS patients. •Uveitis is the swelling and irritation of the uvea (anterior segment) and can be caused by autoimmune disorders, infection or exposure to toxins. Vitrasert •For treatment of chronic, non-infectious uveitis (inflammation) including sympathetic ophthalmia. •3mm x 2mm x 5mm in size •Reservoir of flucinolone acetonide (corticosteroid thought to act by inducing phospholipase A2 inhib. proteins). 600ng a day decreasing to 300400ng over the first month. •Inserted through the pars plana into the vitreous humour •Active for 2 and a half years •Removal can cause problems •SEs = Cataracts (observed in 90% of patients after 3 years), increased I.O pressure, eye pain, headache, nasopharyngitis and joint pain. Structure •Retinitis Pigmentosa is a progressive retinal dystrophy which affects the photoreceptors and causes loss of peripheral vision and eventually central vision. FDA approved in 1996, Vitrasert was first non-biodegradable, intravitreal implant. Used for the delivery of the anti-viral drug, ganciclovir to treat AIDs-related Cytomegalovirus (CMV) Retinitis. Ganciclovir is a synthetic analogue of the nucleoside 2-deoxyguanosine, which causes chain termination, preventing replication. Each implant holds 4.5-5mg of the prodrug which is released at a rate of approx. 11.5µg/hr over 5-8 months. The 4mm device consists of a compressed drug pellet core which is completely covered, except at its top surface, with the impermeable polymer; EVA. This entire assembly is then coated by the permeable polymer; (PVA). Pros: In addition, to reduced systemic S/Es, increased efficacy and reduced dosing frequency, studies show treatment with vitrasert significantly slows down the median time to disease progression in comparison to I.V. ganciclovir therapy. Con: Increased risk of developing contralateral eye retinitis and systemic CMV. Surgical Implantation The implant is inserted by making a 5-6mm scleral incision into the pars plana. It is then fixed into place using sutures. The wound is closed and a saline solution is injected to restore normal ocular pressure. Most patients experience blurred vision which usually clears between 2-4 weeks after surgery. Implants: The way forward? Side Effects and Complications of Implants Vitreous Haemorrhage Endophthalimitis Cystoid Macular Oedema Retinal Detachment Advances in Implants/ Developments Injectable Implants: •Iluvien is a non-biodegradable implant that was recently approved as a treatment for DME. It is in phase II trials for the treatment of wet and dry AMD and RVO and its active ingredient is fluocinolone acetonide. It can be delivered intravitreally using a 25 gauge needle, this is a mninimally invasive procedure as there is no need for a suture and is easier to deliver than retisert due to its smaller size. Biodegradable Ozurdex Ozurdex is a biodegradable implant that contains demaxethasone. It is an intravitreal implant that delivers a sustained release of demaxaethasone (700ml) to the retina and vitreous humour. Ozurdex can improve visual acuity and macular thickness. It is used to treat macular edema, retinal vein occlusion and non-infectious uveitis (posterior). Encapsulated Cell Technology (ECT) •ECT has been used in non-biodegradable implants and is a cell-based delivery system whereby implants can be used to deliver genetically modified cells in a hollow tube made from semi-permeable membrane with both ends of the polymer sealed. Ciliary neurotrophic factor (CNTF) has been proved to protect the retina against degeneration. An ETC implant containing NTC-201 cells which were human retinal pigment epithelial cells that were modified to over produce CNTF were shown to significantly reduce retinal degeneration in animal models. Future Perspectives References