* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Human Dissection Anatomy
Survey
Document related concepts
Transcript
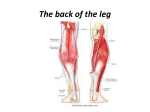
Human Dissection Anatomy Texts: - Anatomy by Carmine D. Clemente, 5th edition, available at the ASUCLA bookstore or the Health Sciences bookstore - Course Lab Manual– available at the ASUCLA bookstore Course Materials: You are responsible for providing your own lab coat and dissection kit. Both are available at the Health Sciences bookstore, and must be obtained before the first lab meeting. Course objectives: To expose students to a more in depth analysis of human anatomy than they have previously received through dissection of the of the upper and lower extremity. Dissection will focus on musculature, vascularization, and innervation. Lecture will cover all anatomical features seen in lab, as well as developmental, functional, and clinical considerations. Grading: The following is the point distribution for the class: Lower extremity Written Exam 100pts Practical Exam 100pts Prosection/Participation 25pts Upper Extremity Written Exam 100pts Practical Exam 100pts Prosection/Participation 25pts Quizzes 50pts TOTAL 500pts Quizzes will be based on your preparation for the day’s lab and will be given at the beginning of each lab. The Prosection/Participation grade will be based on attendance, participation, and quality of dissection. This class will based on a straight scale. There will be no curve: 93-100% = A 83-87% = B 73-77% = C 90-93% = A80-83% = B70-73% = C87-90% = B+ 77-80% = C+ 67-70% = D+ 63-67% = D 60-63% = DBelow 60% = F Make-up written exams are available only under extraordinary circumstances and only with verifiable documentation. Make-up practical exams are NOT possible. The schedule for the quarter is given below; please plan accordingly. There is no extra credit available. Course Schedule (Labs on topics are following day): Date Topic Lecture 1 Introduction, development, LE overview, skinning of Gluteals, Inguinal Region and Thigh; Anatomy of Interior Pelvis Lecture 2 Anterior and Medial Thigh Lecture 3 Posterior Thigh, Gluteal Region including External Rotators Lecture 4 Skinning of Leg; Anatomy of Posterior Leg and Sole of Foot Lecture 5 Anterior and Lateral Leg and Dorsum of Foot; Gait; Review of prosections Lecture 6 Lower Extremity Written Exam Lecture 7 Lower Extremity Practical Exam Lecture 8 UE Overview, skinning of back, shoulder, and chest; Anatomy of Back, Scapular, and Pectoral Regions; Biomechanics Lecture 9 Abdomen, Axilla, Brachial Plexus Lecture 10 Skinning of arm and forearm; Anatomy of Anterior Arm and Forearm Lecture 11 Posterior Arm and Forearm Lecture 12 The Hand; Review of prosections Lecture 13 Upper Extremity Written Exam Lecture 14 Upper Extremity Practical Exam Sources for pictures and diagrams in lecture and dissector: Agur,A.M.R, M.J. Lee. 1999. Grant’s Atlas of Anatomy. 10th ed. Lippincott, Williams & Wilkins, New York. 760pp. Aiello, L. and C. Dean. 1990. An Introduction to Human Evolutionary Anatomy. Academic Press, London. 596p. Cahill, D.R. 1997. Lachman’s Case Studies in Anatomy. 4th ed. Oxford University Press, New York. 415pp. Clemente, C.D. 1997. Anatomy. 4th ed. Lippincott, Williams & Wilkins, New York. 604pp. Gilbert, S.F. 1997. Developmental Biology. 5th ed.Sinauer Associates, Inc., Sunderland, MA. 957pp. Hildebrand, M. 1995. Analysis of Vertebrate Structure. 4th ed. John Wiley & Sons, Inc., New York. 657pp. Kapit, W. and L.M. Elson. 1993. The Anatomy Coloring Book. 2nd ed. Harper Collins, New York. 194pp. McMinn, R.M.H., R.T. Hutchings, J.Pegington, P.Abrahams. 1993. Color Atlas of Human Anatomy. 3rd ed. MosbyWolfe, New York. 359pp. Rohen, J.W., C. Yokochi. 1993. Color Atlas of Anatomy. 3rd ed. Igaku-Sholin, New York. 484pp. Rosse, C and P. Gaddum-Rosse. 1997. Hollinshead’s Textbook of Anatomy. 5th ed. Lippincott-Raven, New York. 902pp. Sadler, T.W. 1995. Langman’s Medical Embryology. 7th ed. Williams and Wilkins, Baltimore. 460pp. Sauerland, E.K. 1999. Grant’s Dissector. 12th ed. Lippincott, Williams & Wilkins, New York. 329pp. Tilton, B. 1998. The Wilderness First Responder. The Globe Pequot Press, Guilford, CT. 314pp. LECTURE 1 AN INTRODUCTION TO TISSUES, SPINAL NERVES, AND THE DEVELOPMENT, EVOLUTION, AND ANATOMY OF THE LOWER EXTREMITY Connective Tissue Loose Connective Tissue Dense Connective Tissue Peripheral Nerves Dorsal Root Ventral Root Spinal Nerve Dorsal Ramus Ventral Ramus Development and Evolution Embryonic Tissues Axes Determination proximal-distal anterior-posterior dorsal-ventral forelimb-hindlimb Evolutionary axes Lower Extremity Overview Movements Hip: Knees: Ankle: Toe: Blood Supply: Innervation: The Interior of the Pelvis Musculature Psoas Major m. Iliacus m. Blood Supply of the Pelvis Nerves of the Pelvis LAB 1: SKINNING THE THIGH AND STRUCTURES OF THE PELVIS General Notes on Dissection Techniques The goals of this course are to extend your knowledge of anatomy that you obtained in Physiological Sciences 107, as well as a more practical goal of preparing cadavers for use in that class this year as prosections. In pursuit of these goals, there are some important things you should keep in mind while dissecting. First and foremost, it is important to isolate structures without causing excessive damage. If you are not told to cut or remove a structure, DON’T. To facilitate this, the majority of the dissection you do will be BLUNT DISSECTION. You will use forceps, scalpel handles, probes and your fingers to separate large structures. Smaller structures can be separated with scissors using an OPENING motion parallel to the structure of interest. SCALPEL BLADES WILL GENERALLY ONLY BE USED FOR INITIAL SKIN INCISIONS, and even then only with great care. The most important thing you can do is COME PREPARED. Read these guides before coming to lab and familiarize yourself with the corresponding pages in the atlas. Having a knowledge of the area you are working on ahead of time will help you to deliberately look for structures, instead of “digging around” and happening upon “something interesting”. Keep your atlas present while dissecting. Remember, a clean dissection is part of your grade so it is in your best interest to do a good job. At the same time you need to be efficient enough to learn all the material in the allotted time. Note that the plates listed are suggestions to help you find structures. Most structures are shown on multiple plates, and not all are listed, so it would be worth it to look up things in the index to find different views. The structures you are responsible for identifying during today’s lab are: great saphenous v. femoral n. descending aorta obturator n. common iliac a. obturator a. internal iliac a. iliacus m. external iliac a. psoas major m. saphenous opening Before beginning your prosection, orient yourself to the limb. Note its side, gender, and any abnormalities. Skinning the Thigh (Plate 370) The first step in doing any dissection is the removal of the skin. While removing it you will note many layers. The actual skin varies in thickness, and this should be noted in order to facilitate a better dissection. Under the skin is a layer of subcutaneous fascia. this contains much of the body’s fat, as well as connective tissue and superficial nerves. We won’t concentrate much on structures in this layer. The final layer is a deep fascia, or fascia lata as it’s known in the leg, which should be kept intact until necessary. A good technique for skinning is shown in the figures at the end of this lab. Making a hole for a finger to pull back a flap of skin will allow you to keep tension while cutting connective tissue. In our case, we will be removing the superficial fascia as well. It is important when making skin incisions to not go too deep; you can always deepen them later. • • • • • • Using a scalpel, make a superficial incision from a point midway between the anterior superior iliac spine and the pubis, down the anterior aspect of the thigh, to just below the tibial tuberosity. Next make two encircling incisions, one about two inches below the tibial tuberosity, and another along the inguinal line and around posteriorly following the gluteal crease. Finally make a vertical incision on the posterior aspect of the thigh connecting your two encircling incisions. Start by removing the skin from the lateral aspect of the thigh. Remove both skin and superficial fascia, but be careful not to pierce the deep fascia. Make horizontal incisions as necessary to expedite the process. Be especially careful of the deep fascia around the knee, as it serves as attachment for some important muscles. When you have finished the lateral surface, move to the medial surface. All layers of skin and fascia are much thinner here so you should be more careful. Also, make note of the great saphenous vein which runs on the medial surface of the thigh superficial to the deep fascia. Preserve about 4-6 inches of this vein near where it enters the deep fascia, through the saphenous opening. This will serve as a landmark later. Finally, remove the skin from the gluteal region. It is especially important to keep the deep fascia intact here as the fibers of the gluteus maximus m. are closely adhered to this fascia. It is easiest to start the gluteal skinning at the superiomedial corner, where there is usually a thick layer of superficial fascia. Find where this fascia separates and extend this down the length of the sacrum. Now remove the skin from medial to lateral. Some superficial fascia will remain and can be removed later. Lastly, remove the genitalia, being careful not to damage any underlying muscles as many have their origins on the pubic bone. Structures of the pelvis (Plates 252, 253, 256, 282, 287) • Begin by removing any remaining viscera in the pelvic cavity. This can be done while a lab mate is skinning the thigh. Also remove the underlying fascia, or peritoneum, being careful not to damage any underlying structures. • If your cadaver has any part of the descending aorta remaining follow it inferiorly until it branches into the right and left common iliac arteries. Each of these further subdivides into the internal and external iliac arteries. The internal iliac gives off several branches, but you only need to identify the obturator a. • Palpate the floor of the pelvis and find the obturator foramen. The obturator a. will be seen passing through the muscles covering the foramen, accompanied by the obturator n. The obturator nerve and artery supply the muscles on the medial aspect of the thigh that will be examined later. Refer to the diagram at the end of this lab for reference. At this time you can remove the iliac veins that run roughly parallel to the iliac arteries. • Finally, locate and clean the proximal portions of the iliacus and psoas major muscles. The psoas major lies adjacent to the lumbar vertebra. Make note of and KEEP INTACT the various nerves passing under and through the psoas major; many of these are branches of the lumbo-sacral plexus, of which we will only be studying some of the terminal branches. Technique for skinning Vessels and nerves of the pelvic floor LECTURE 2 THE ANTERIOR AND MEDIAL COMPARTMENTS OF THE THIGH Muscular Compartments and Deep Fascia Anterior compartment Lateral Intermuscular Septum Posterior Compartment Posterior Intermuscular Septum Medial compartment Medial Intermuscular septum Iliotibial band (tract) Tensor Fasciae Lata m. Anatomical Spaces of the Anterior Thigh Femoral Triangle Borders Importance Femoral n. Femoral Sheath Lymphatics Adductor Canal Borders Importance Femoral a. Femoral v. Saphenous n. Anterior Compartment of the Thigh Musculature Sartorius m. Quadriceps femoris mm. Rectus femoris m. Vastus lateralis m. Vastus medialis m. Vastus intermedius m. Articularis genu m. Blood Vessels Nerves Medial Compartment of the Thigh Musculature Gracilis m. Pectineus m. Adductor longus m. Adductor brevis m. Adductor magnus m. Blood Vessels Nerves LAB 2: STRUCTURES OF THE ANTERIOR AND MEDIAL COMPARTMENTS OF THE THIGH (Plates 370-383) The structures you are responsible for identifying during this lab are: Inguinal ligament Medial circumflex a. Lateral intermuscular Femoral triangle Lateral circumflex a. septum Femoral n. Pectineus m. Medial intermuscular Femoral sheath Sartorius m. septum Femoral a. Adductor longus m. Gracilis m. Femoral v. Ilopsoas tendon Adductor brevis m. Femoral canal Rectus femoirs m. Adductor magnus m. Deep femoral a. Vastus medialis m. Adductor canal Tensor fascia lata m. Vastus intermedius m. Adductor hiatus Iliotibial band Vastus lateralis m. Patellar tendon The Femoral Triangle • Follow the remnant of the great saphenous v. back to where it enters the saphenous opening, a hole in the deep fascia. The great saphenous vein joins the femoral v. within the femoral triangle, which you can see part of through the saphenous opening. • You can widen the saphenous opening by using blunt dissection to separate the fascia from the underlying tissues, and then cutting it using scissors. Do not extend the cut superiorly to avoid cutting the inguinal ligament. Note the borders of the femoral triangle: the sartorius m. laterally, the adductor longus m. medially, the inguinal ligament superiorly and the roof formed by the deep fascia (which you have cut). The floor of the triangle, which you will see later, is formed by the iliopsoas tendon and pectineus m. • You will note the great saphenous v. entering the femoral sheath to join the femoral v. Within this sheath are other important structures. Open the sheath by passing a probe into it and cutting to the probe. Laterally you will observe the femoral a., a continuation of the external iliac a. you observed in the pelvis. In the middle of the sheath is the femoral v. Medially is the femoral canal, a space containing fat and lymph nodes and vessels. • Lateral to the femoral sheath find the femoral n. which commonly runs superficial to the iliopsoas tendon as it enters the femoral triangle. Be careful not to damage the branches of the femoral nerve that supply the musculature of the anterior compartment of the thigh. • Branching posteriorly from the femoral a. notice three large branches. These may arise from a common stem or separately from the femoral a. They are the deep femoral a. which passes posterior to the adductor longus m., between it and the pectineus m., to supply the posterior compartment of the thigh. The lateral circumflex a. passes deep to the rectus femoris m.. The medial circumflex a. passes between the iliopsoas tendon and the pectineus m. The Anterior Compartment of the Thigh • To expose the anterior compartment of the thigh you will need to remove the remaining part of the deep fascia. Using scissors carefully cut the fascia from the saphenous opening to a • • • • • • point approximately 5 cm above the patella, where the deep fascia becomes continuous with the knee joint capsule. Run your hand laterally under the deep fascia to separate it from the muscles of the anterior compartment. If you extend your hand deep enough you will reach the lateral intermuscular septum and your hand will be redirected toward the femur where the septum attaches at the linea aspera. Note that the deep fascia is thicker on the lateral side of the thigh, forming the iliotibial band (ITB), which can be tensed by the tensor fascia lata m., which is encased in the deep fascia posterior and inferior to the anterior superior iliac spine (ASIS). To preserve this structure trace and cut along its medial border, from the ASIS to the lateral border of the patella. You can now remove the medial portion of the deep fascia. You can now identify the muscles of the anterior compartment. Start with the sartorius and clean it of any remaining connective tissue, being careful not to cut the branch of the femoral nerve that innervates it, and not to extend too distally to where the sartorius inserts into the deep fascia on the medial aspect of the knee. Repeat this procedure for the rectus femoris m. Now, while lifting the rectus femoris m., define the borders of the three vasuts muscles, the vastus lateralis m., the vastus medialis m., and the vastus intermedius m. Together with the rectus femoris m. these muscles form the quadriceps muscle group, which insert, via the patellar tendon, through the patella to the tibial tuberosity. The innervation of the vastus muscles may be less obvious than that of the sartorius and rectus femoris muscles, but you should try to preserve it where it is visible. Replace the sartorius in its anatomical position and note that crosses the thigh superiolaterally to inferio-medially and covers the femoral artery and vein after they leave the femoral triangle, as well as two small nerves (branches of the femoral nerve). These nerves are the branches to the vastus medialis m. and the saphenous n. (a cutaneous branch). The space that the sartorius m. creates, along with the vastus medialis m. and adductor longus m. is called the adductor canal, and where the vessels exit the canal and pass posteriorly through the adductor magnus m. is called the adductor hiatus. The femoral vein can be removed inferior to its junction with the great sahpenous vein. The Medial Compartment of the Thigh • Remove the remainder of the fascia covering the medial compartment of the thigh. • Begin superiorly by locating the two branches of the obturator nerve as they pass anterior and superior to the adductor brevis m. • Isolate and clean the pectineus m., the three adductor muscles, and the gracilis m. As with the sartorius, be careful when cleaning the distal attachment of the gracilis m. as it inserts into the deep fascia on the medial aspect of the knee. Try to preserve the perforating arteries of the deep femoral a. as it travels deep to the adductor longus m. LECTURE 3 GLUTEAL REGION, POSTERIOR COMPARTMENT OF THE THIGH, POPLITEAL FOSSA Gluteal Region Sacrospinous ligament Sacrotuberous ligament Musculature Gluteus maximus m. Gluteus medius m. Gluteus minimus m. External Rotators of Hip Piriformis m. Gemellus superior m. Obturator internus m. Gemellus inferior m. Obturator externus m. Quadratus femoris m. Blood Supply Nerves Posterior Compartment of Thigh Musculature “hamstrings” Semitendinosus m. “pes anserinus” Semimembranosus m. Biceps femoris m. – long head Biceps femoris – short head Blood Supply Nerve Supply Popliteal Fossa Borders Contents popliteal a. popliteal v. tibial n. common peroneal n. LAB 3: GLUTEAL REGION, POSTERIOR COMPARTMENT OF THE THIGH, AND POPLITEAL FOSSA (Plates 383-396) The structures you are responsible for identifying during this lab are: Gluteus maximus m. Piriformis m. Biceps femoris m. Gluteus medius m. Quadratus femoris m. (both heads) Gluteus minimus m. Obturator externus m. Tibial n. Sciatic n. Obturator internus m. Common peroneal n. Superior gluteal a. Gemellus superior m. Popliteal a. Superior gluteal n. Gemellus inferior m. Pudendal a. Inferior gluteal a. Semitendinosus m. Pudendal n. Inferior gluteal n. Semimembranosus m. Genicular aa. Gluteal Region • Locate the superior and inferior borders of the gluteus maximus m. and cut the deep fascia along the superior border. You will see a portion of the gluteus medius m. above the superior border of the gluteus maximus m. Pass your hand under the gluteus maximus m. and separate it from the muscles deep to it. Be careful not to break any vessels or nerves you feel. Once you have separated the muscle insert a scalpel handle deep to the muscle and as far medially as possible. Cut through the muscle with another scalpel using the handle of the inserted scalpel as a depth gauge. Inferiorly notice that the muscle is attached to the sacrotuberous ligament. You will need to detach the muscle from this as well to reflect it. • When reflecting the gluteus maximum muscle note the vessels and nerves entering its deep surface. Cut these close to the muscle to allow for reflection. • You should now see the large sciatic n. entering the area below the piriformis m. Also note the stumps of the inferior gluteal n. and inferior gluteal a. entering the field in the same place, which entered the deep surface of the gluteus maximus m. Also found below the piriformis m. are the pudendal a. and pudendal n.. These are only briefly seen as they pass around the sacrospinous ligament to renter the pelvis in the pudendal canal. (see diagrams below) • Immediately inferior to the piriformis m. locate the gemellus superior m.. Immediately inferior to this is the obturator internus m., and then the gemellus inferior m. Inferior to this is the obturator externus m. although it is probably obscured by the gemellus inferior m. and the next inferior muscle, the quadratus femoris m. (see diagrams below) • In the same technique as used for reflecting the gluteus maximum muscle, identify the free border of the gluteus medius m. and detach it from its proximal attachment on the ilium. Be careful not to sever any vessels or nerves below it. These structures, the superior gluteal a. and superior gluteal n. arise superior to the piriformis and inferior to the gluteus minimus m. which is now visible. Posterior Compartment of the Thigh • Remove the remainder of the deep fascia from the posterior thigh, being careful to leave the posterior extent of the ITB. This can be done by inserting a hand under the fascia, locating the lateral intermuscular septum and using that as the posterior border of the ITB. • Clean and expose the muscles of the posterior compartment of the thigh, the hamstrings. Also clean the sciatic nerve, found by moving the biceps femoris m. laterally, being careful to preserve the branches of it, as well as perforating branches of the deep femoral a. Note that the 3 hamstrings, the semimembranosis m., the semitendinosis m., and the biceps femoris m. have a common origin from the ischial tuberosity, except for the short head of the biceps femoris m. which arises from the linea aspera (and is therefore not considered a hamstring muscle). Clean their distal attachments on either side of the popliteal fossa, being careful not to damage the common attachment of the semitendinosus m., sartorius m. and gracilis m. at the pes anserinus. Popliteal fossa • Note the borders of the popliteal fossa: superio-laterally the biceps femoris m., superiomedially the semimembranosus m. and semitendinosus m., and inferiorly the heads of the gastrocnemius m. (which we will discuss later) • Follow the sciatic n. to where it branches into the tibial n. and common peroneal n.. Clean these as they pass through the popliteal fossa. • Remove fat in the popliteal fossa surrounding the popliteal a. and popliteal v. If you pass a probe from the anterior compartment of the thigh, through the adductor hiatus, and into the popliteal fossa you will verify that the popliteal a. is just a continuation of the femoral a. Remove the popliteal vein, and with further cleaning you may be able to identify the genicular branches of the popliteal a. LECTURE 4 POSTERIOR COMPARTMENT OF THE LEG AND SOLE OF THE FOOT Compartments of the Leg Anterior Compartment Lateral Compartment Posterior Compartment Posterior Compartment of the Leg – Superficial Musculature “triceps surae” Gastrocnemius m. Soleus m. Plantaris m. Posterior Compartment of the Leg – Deep Popliteus m. Tibialis posterior m. Flexor digitorum longus m. Flexor hallucis longus m. Retinaculum Blood Supply Nerves The Sole of the Foot Layer 1: Flexor digitorum brevis m. Abductor hallucis m. Abductor digiti minimi m. Layer 2: Quadratus plantae m. Lumbrical mm. Layer 3: Flexor hallucis brevis m. Flexor digiti minimi brevis m. Adductor hallucis m. Layer 4: Plantar interossei Dorsal interossei Ligaments Long Plantar ligament Short plantar (calcaneocuboid) ligament Plantar calcaneonavicular (spring) ligament Blood Supply Nerves LAB 4: THE POSTERIOR COMPARTMENT OF THE LEG AND SOLE OF THE FOOT (Plates 396, 400, 408, 412-429) The structures you are responsible for identifying during this lab are: Gastrocnemius m. Tibialis posterior m. Adbuctor digiti minimi m. Plantaris m. Posterior tibial a. Flexor digiti minimi brev. m. Soleus m. Sural n. Medial plantar a. Achilles tendon Peroneal a. Medial plantar n. Popliteus m. Flexor retinaculum Lateral plantar a. Flexos hallicus longus m. Abductor hallucis m. Lateral plantar n. Flexor digitorum longus m. Flexor hallucis brevis m. Quadratus plantaem. Lumbrical mm. Plantar aponeurosis Skinning the Leg • Make a vertical incision along the medial surface of the tibia stopping at the ankle. make a cut encircling the ankle from malleolus to malleolus, being VERY careful not to incise the deep fascia, which form the retinacula in this area. Remove the skin from the leg using blunt dissection • On the foot make two shallow incisions on the medial and lateral surfaces. Starting at the heel reflect the skin off the foot to the base of the toes. On the sole it may be necessary to take the skin off in sections due to its tight adhesions to the deep fascia. Be careful near the toes not to cut the tendons of the digital flexors. • Identify the sural n., a cutaneous nerve, arising from the fascia between the heads of the gastrocnemius m. about midway down the leg. The Posterior Compartment • Remove the deep fascia overlying the posterior musculature. • Clean the proximal portion of the gastrocnemius m., being careful to preserve the tibial n. as it passes between the heads of, and deep to, this muscle. Separate the heads as far as BLUNT dissection will allow. • Slip your fingers between the gastrocnemius m. and the underlying soleus m. and separate them only as far as BLUNT dissection will allow. Look for the thin tendon of the plantaris m. lying between these muscles and follow it proximally to its small muscle belly. Locate the origin of the popliteus m. near that of the plantaris m. and clean it. • Follow the Achilles tendon distally to its insertion into the calcaneus. Pass a probe under the tendon, separating it from underlying tissues. Using the probe as a depth gauge, cut this thick tendon with a scalpel. • Clean out the fibrous tissue deep to the insertion of the Achilles tendon. On the medial and lateral surfaces of the deep fascia you will see an area that is striated and thicked, the flexor retinaculum. Trim the deep fascia to this point, being careful not to go more anterior than the malleoli. • Carefully reflect the soleus m. and separate it from its medial attachment as much as possible without damaging the muscle. Under the soleus m. is an intermusclular septum separating it from the deeper muscles of the posterior leg. • After carefully slitting the intermuscular septum you should be able to see the posterior tibial a., peroneal a., and tibial n. The peroneal a., after branching off the posterior tibial a., • will pass deep to the flexor hallucis longus m. (on the lateral side of the posterior leg, attached to the fibula), while the other two structures will remain superficial to this muscle. The posterior tibial a. will travel on the surface of the tibialis posterior m., which is in the middle of the leg. Identify the other deep muscle of the leg the flexor digitorum longus m. medially, and follow the tendons of all three deep muscles until they pass under the fascia covering the ankle. Note their relations to the malleolus and sustentaculum tali. The posterior tibial a. and tibial n. travel together and branch to form the medial plantar a. and n., and lateral plantar a. and n. deep to the flexor retinaculum. The Sole of the Foot (see diagrams below) Layer 1 • Remove any remaining superficial fascia of the foot. Next, gently cut through the plantar aponeurosis at the calcaneus and retract it distally. Be careful not to damage the underlying flexor digitorum brevis m., which should then be cleaned. • Find the abductor hallucis m. and abductor digiti minimi m. on the medial and lateral surfaces of the foot, respectively. Also locate the distal ends of the flexor hallucis brevis m. and flexor digiti minimi brevis m. which lie toward the middle of the foot next to their respective abductors. • Pass a probe under the proximal attachment of the flexor digitorum brevis m. to use as a depth gauge, cut the muscle, and reflect it distally. You should now be able to see the plantar nerves and arteries. Layer 2 • Under the reflected flexor digitorum brevis m. you should see the tendons of the flexor digitorum longus m. as well as the tendon of the flexor hallucis longus m. • Attached to the tendons of the flexor digitorum longus m. notice the lumbrical mm. inserting into the toes, as well as the distal attachment of the quadatus plantae m. which arises on the calcaneus. LECTURE 5 ANTERIOR AND LATERAL COMPARTMENTS OF THE LEG AND DORSUM OF THE FOOT Anterior Compartment of the Leg Musculature Tibialis anterior m. Extensor hallucis longus m. Extensor digitorum longus m. Fibularis tertius m. Retinacula Blood Supply Nerves Lateral Compartment of the Leg Musculature Fibularis longus m. Fibularis brevis m. Retinacula Blood Supply Nerves Dorsum of Foot Musculature Extensor hallucis brevis m. Extensor digitorum brevis m. Blood Supply Nerves Gait Cycle Center of Mass Gait Cycle Heel Strike Flat Foot Heel Off Toe Off Swing Phase Sexual Dimorphism Trendelenburg Gait Foot Drop LAB 5: THE ANTERIOR AND LATERAL COMPARTMENTS OF THE LEG AND THE DORSUM OF THE FOOT (Plates 399-411) The structures you are responsible for identifying during this lab are: Tibialis anterior m. Anterior tibial a. Peroneus longus m. Extensor hallucis longus m. Deep peroneal n. Peroneus brevis m. Extensor digitorum longus m. Extensor hallucis brevis m. Common peroneal n. Peroneus tertius Superficial peroneal n. Dorsalis pedis a. Extensor digitorum brevis m. Extensor retinaculum The Anterior Compartment • Because the deep fascia on the anterior surface of the leg is an origin for the tibialis anterior m. it is difficult to remove. The best way is to begin distally over the tendon of the tibialis anterior m. Lift a small piece of fascia with a forceps and use a probe to separate it from the underlying tissues. Peel the fascia superiorly, using scissors when necessary to cut some of the tighter adhesions of the tibialis anterior m., being careful not to excessively damage the muscle. • Examine the four muscles of the anterior compartment. From medial to lateral they are: tibialis anterior m., extensor hallucis longus m., then the extensor digitorum longus m.. The peroneus tertius m. is an offshoot of the extensor digitorum longus m. • Between the tibialis anterior m. and the extensor hallucis longus m. find the anterior tibial a. (which comes over the interosseous membrane from the posterior tibial a. in the posterior compartment) and deep peroneal n. (arising from the peroneal n. at the head of the fibula) • Find the extensor retinaculum, a thickened, striated portion of the deep fascia on the medial surface of the ankle. It forms a Y, with the base at the calcaneus, and arms ending at the medial malleolus and dorsum of the foot. • Remove the deep fascia of the dorsum of the foot, keeping the retinaculum intact, noticing the tendons of the digital extensors. The Lateral Compartment • Remove any remaining fascia over the lateral compartment being careful not to damage the superficial peroneal n. (the other terminal branch of the peroneal n.), and identify and clean the peroneus longus m. and peroneus brevis m. The Dorsum of the Foot • Identify the two small muscles deep to the tendons of the extensor digitoum longus m., the extensor hallucis brevis m. and extensor digitorum brevis m. Also note the anterior tibial a. terminating in the dorsalis pedis a. LECTURE 6 INTRODUCTION TO THE UPPER EXTREMITY; BACK, SCAPULAR, PECTORAL REGIONS Upper Extremity Overview Movements: Scapula: Glenohumeral: Humeroulnar: Radioulnar: Wrist: Fingers: Blood Supply: Nerves: The Back Musculature Latissimus Dorsi m. Trapezius m. Rhomboid major m. Rhomboid minor m. Levator scapulae m. DEEP BACK MUSCULATURE Erector Spinae Group Transversospinalis Group The Scapular Region Musculature Teres major m. Deltoid m. THE ROTATOR CUFF MUSCLES Subscapularis m. Supraspinatus m. Infraspinatus m. Teres minor m. Blood Supply Nerves Anatomical Spaces Quadrangular Space Triangular Space Pectoral Region Musculature Pectoralis major m. Pectoralis minor m. Serratus anterior m. Blood Supply Nerves Anatomical Space Deltopectoral triangle LAB 6: THE BACK, SCAPULAR, AND PECTORAL REGIONS (Plates 11-15, 24-25, 3031, 328, 330) The structures you are responsible for identifying during this lab are: Trapezius m. Circumflex scapular a. Supraspinatus m. Latissimus dorsi m. Pectoralis major m. Subscapularis m. Rhomboids major m. Pectoralis minor m. Serratus anterior m. Rhomboids minor m. Medial and lateral pectoral nn. Long thoracic n. Levator scapulae m. Deltopectoral triangle Infraspinatus m. Cephalic v. Teres major m. Quadrangular space Teres minor m. Triangular space Axillary n. Posterior humeral circumflex a. Skinning the Thorax and Arm • Make an incision encircling the arm, halfway between the shoulder and elbow. Extend the incision up the lateral surface of the arm, across the shoulder, to the root of the neck. Make a third incision up the medial surface of the arm and back down the lateral surface of the thorax. Keep these incisions relatively shallow to avoid damaging superficial structures. • Start skinning at the inferio-medial corner of the back and continue superio-laterally to remove the skin on the back. Be particularly careful on the medial border of the back to avoid damaging the attachment of the latissimus dorsi m., the thoracolumbar fascia. In order to facilitate this, when cleaning the latissimus dorsi m. after skinning, extend no further medially than the muscle fibers. • Next skin the anterior thorax, and end with the skinning of the upper arm. Be careful over the deltoid muscles, as they are closely adhered to the deep fascia. The Back • Identify and clean the two large superficial muscles of the back: the latissimus dorsi m. and the trapezius m. • Starting inferiorly, detach the trapezius muscle from its origin on the spinous processes of the vertebrae. Be sure not to damage the attachments of the underlying rhomboid major and minor mm. • After reflecting the trapezius m., clean the rhomboid mm. Look for and clean the levator scapulae m. deep to the trapezius m. attached to the superior angle of the scapula The Scapular Region • The supraspinatus m. and subscapularis m. will be hard to see because of the insertion of the trapezius m., but note where they are. The infraspinatus m. should be evident and easy to clean • Clean the teres major m. and teres minor m. lateral to the scapula, attached at its inferior border. Be careful not to damage the contents of the two important anatomical spaces they border. • The quadrangular space is bordered by the teres major m., teres minor m., the long head of the triceps brachii m. and the humerus. Identify and clean this space, noting its contents, the axillary n. and posterior humeral circumflex a. • The triangular space is bordered by the teres minor m., teres major m., and the long head of the triceps brachii m. Identify and clean this space and its contents, the circumflex scapular a. a branch of the subscapular a. The Pectoral Region • Turning now to the anterior surface of the body, clean and define the borders of the pectoralis major m. Note that it has fibers running in two directions, a clavicular part with horizontal fibers, and a sternal part with oblique fibers. • At the superior border of the pectoralis major m. note the deltopectoral triangle between it and the anterior deltoid. The cephalic vein is found here. • Make an incision along the clavicular origin of the pectoralis major m., continuing down along the sternal origin until the entire muscle can be reflected toward the arm. When reflecting it, cut an nerves or vessels to it close to the muscle. • Clean the underlying nerves and vessels, and the pectoralis minor m. Using blunt dissection to separate this muscle from the underlying structures and then detach it near its insertion at the coracoid process. • Also note the oblique fibers of the serratus anterior m. extending from the digit-like origins on the anterolateral wall of the thorax around the back and under the scapula. The long thoracic n. lies on top of this muscle. LECTURE 7 ABDOMINAL WALL AND AXILLA Abdominal Wall Musculature External oblique m. Internal oblique m. Transversus abdominis m. Rectus abdominus m. The Axilla Borders Contents Vessels Axillary a. and its branches Supreme thoracic a. Thoracoacromial Lateral thoracic a. Subscapular a. Anterior humeral circumflex a. Posterior humeral circumflex a. Nerves Brachial Plexus Branches from Roots Dorsal scapular n. Long Thoracic n. Branches from Trunks Nerve to subclavius m. Suprascapular n. Branches from Divisions Branches from Cords Lateral pectoral n. Upper subscapular n. Thoracodorsal n. Lower subscapular n. Medial Pectoral n. Medial brachial cutaneous n. Medial antebrachial cutaneous n. Terminal Nerves Musculocutaneous n. Axillary n. Radial n. Median n. Ulnar n. LAB 7: THE ANTERIOR ABDOMINAL WALL AND AXILLA (Plates 16-21, 36-37, 178, 180-184) The structures you are responsible for identifying during this lab are: Axillary a. BRACHIAL PLEXUS: Lateral thoracic a. Lateral Cord Thoracoacromial a. Medial Cord Subscapular a. Posterior Cord Circumflex scapular a. Medial & lateral pectoral nn. Posterior humeral circumflex a. Long Thoracic n. Anterior humeral circumflex a. Thoracodorsal n. Coracobrachialis m. Medial brachial cutaneous n. External oblique m Axillary n. Linea alba Musculocutaneous n. Interal oblique m. Median n. Transversus abdominus m. Ulnar n. Rectus abdominus m. Radial n. Rectus sheath Medial antebrachial cutaneous n. Thoracodorsal a. The Anterior Abdominal Wall • Remove all remains of the superficial fascia from the external oblique m., so that you are able to clearly distinguish between the muscular and aponeurotic portions. Note the linea alba at midline • Now try and expose the rectus abdominus m. To do this, open the rectus sheath just lateral to the linea alba. Observe that the rectus sheath is firmly attached to the rectus muscle at 3 or 4 tendinous insertions. These can be severed with a scalpel, and the rectus sheath reflected laterally. • You can also try and observe the interal oblique m. and transversus abdominus m. which lie successively deeper to the rectus abdominus m. Their aponeurotic portions have a complex relationship with this muscle. The Axilla • Begin by identifying the axillary a. Recall that it is the distal extension of the subclavian a. and is divided into three parts determined by its relative position to the pectoralis minor m. • Identify the two branches of the second part of the axillary a. (the part under the pectoralis minor m.): the thoracoacromial a. and the lateral thoracic a. The thoracoacromial artery has two main branches, one towards the acromion and one to the pectoral muscles. The lateral thoracic a. joins the long thoracic n. down the lateral side of the thorax. • Identify the 3 branches of the third part of the axillary a. (the part distal to the pectoralis minor m.): 1)the subscapular a., which branches to form the circumflex scapular a. (which you saw in the triangular space last lab) and the thoracodorsal a. which travels with the thoracodorsal n. to the latissimus dorsi m.; 2) the posterior humeral circumflex a. (which you saw last lab in the quadrangular space); 3) the anterior humeral circumflex a. which may come from a common trunk with the posterior humeral circumflex a. • • • • On the medial surface of the arm identify the median n. and ulnar n. They should be near the axillary artery. Follow them back toward the brachial plexus where they are met by the musculocutaneous n. which passes through the coracobrachialis m. These three nerves form an M on the anterior surface of the axillary a. Now find the radial n. deep to the axillary a. Follow it proximally and find the axillary n. as it branches to enter the deltoid muscle. Proximal to this branch point is the posterior cord of the brachial plexus. Identify the origin of the thoracodorsal n. as it branches from this cord. Follow the musculocutaneous n. proximally and identify the lateral cord. Find the lateral pectoral n. as it branches from the lateral cord. Follow the ulnar n. proximally and identify the medial cord. Find the medial pectoral n., the medial brachial cutaneous n., and the medial antebrachial cutaneous n. as they branch off the medial cord LECTURE 8 ANTERIOR COMPARTMENTS OF ARM AND FOREARM Anterior Compartment of Arm Muscles Coracobrachialis m. Biceps brachii m. (long head) Biceps brachii m. (short head) Brachialis m. Blood Supply Nerves Cubital Fossa Borders Contents Anterior Compartment of Forearm Muscles Superficial Group Flexor carpi ulnaris m. Flexor digitorum superficialis m. Palmaris longus m. Flexor carpi radialis m. Pronator teres m. Deep group Flexor digitorum profundus m. Flexor pollicis longus m. Pronator quadratus m. Blood Supply Nerves Carpal Tunnel Borders Contents LAB 8: THE ANTERIOR COMPARTMENT OF THE ARM AND FOREARM (Plates 2937, 46-53) The structures you are responsible for identifying during this lab are: Brachial a. Palmaris longus m. Radial a. Deep brachial a. Flexor carpi ulnaris m. Ulnar a. Bicipital aponeurosis Pronator teres m. Common Biceps brachii m. Flexor digitorum superficialis m. interosseous a. Brachialis m. Flexor digitorum profundus m. Flexor retinaculum Brachioradialis m. Flexor pollicis longus m. Flexor carpi radialis m. Pronator quadratus m. Skinning the Arm and Forearm • Make an incision encircling the wrist being careful not to damage superficial structures • Make a second incision on the ventral surface at the arm, starting at the proximal end of the remaining skin and moving distally to your first incision. Remove the skin keeping the deep fascia intact • After the arm is skinned, you may remove the deep fascia from the surface of the muscles, being careful near the wrist not to destroy the flexor retinaculum. The Anterior Compartment of the Arm • Follow the median n., ulnar n., and brachial a. (a continuation of the axillary a. after the teres major m.) from the axilla to the cubital fossa. Notice that for much of its length the median n. lies medial to the brachial a. Note that neither nerve supplies any muscles in the arm. Also notice how the ulnar n. wraps around the medial epicondyle of the humerus. • Identify the deep brachial a. branching from the posterior aspect of the brachial a. at its proximal end, and going to the posterior compartment of the arm. • Find the musculocutaneous n. as it exits the coracobrachialis m. between the biceps brachii m. and the brachialis m. This is nerve of the anterior compartment of the arm. • Clean all the anterior compartment muscles. The Cubital Fossa • Follow the biceps distally into the forearm. On the medial surface of its tendon find the bicipital aponeurosis that attaches to the deep fascia of the forearm. Note that it covers the brachial a. and median n. Sever this aponeurosis without damaging the underlying strucutures or tendon • Clean the contents of the cubital fossa: the brachial a. branching into the ulnar a. and radial a., and the median n. The Anterior Compartment of the Forearm • In the forearm, separate the muscles of the superficial layer: (from lateral to medial) the brachioradialis m., the pronator teres m., the flexor carpi radialis m., the palmaris longus m., and the flexor carpi ulnaris m.. Do not separate the muscle bellies of the deeper muscle, the flexor digitorum superficialis m. • • • Note the ulnar n. and ulnar a. deep to the flexor digitorum superficialis m. Lateral to these, at the midline of the forearm, and also under that muscle, find the continuing course of the median n. Clean the brachioradialis m. and find the radial a. running deep to it. Finally locate the deep muscles of the forearm, the flexor digitorum profundus m., the flexor pollicis longus m., and the pronator quadratus m. LECTURE 9 POSTERIOR COMPARTMENTS OF ARM AND FOREARM Posterior Compartment of Arm Muscle Triceps brachii m. Blood Supply and Nerve Posterior Compartment of Forearm Muscles Superficial layer Brachioradialis m. Extensor carpi radialis longus m. Extensor carpi radialis brevis m. Extensor digitorum m. Extensor digiti minimi m. Anconeus m. Extensor carpi ulnaris m. Deep group Supinator m. Abductor pollicis longus m. Extensor pollicis brevis m. Extensor pollicis longus m. Extensor indicis m. Anatomical snuffbox Vessel and Nerve LAB 9: THE POSTERIOR COMPARTMENT OF THE ARM AND FOREARM (Plates 38-43, 54-61) The structures you are responsible for identifying during this lab are: Triceps brachii m. Extensor carpi ulnaris m. Ext. pollicis brevis m Extensor carpi radialis longus m. Supinator m. Abd. poll. longus m. Extensor digitorum m. Extensor indicis m. Post. interosseous a. Extensor digiti minimi m. Extensor pollicis longus m. Deep radial n. Extensor carpi radialis brevis m. The Posterior Compartment of the Arm • Follow the radial n. out of the brachial plexus. It should be found in the interval between the brachioradialis m., biceps brachii m., and brachialis m. Note the nerve’s passage deep to the lateral head of the triceps brachii m. with the deep brachial a. Note that both structures lie in the spiral groove of the humerus. • Clean and separate the three heads of the triceps brachii m. and note that they receive their innervation from the radial n. The Posterior Compartment of the Forearm • Clean the deep fascia from the posterior surface of the arm. Be careful to preserve the extensor retinaculum near the wrist. Also be careful to not damage any muscles when separating the fascia from the proximal forearm where many muscles use it as an attachment site. • Separate the muscles of the superficial layer, which mainly arise from the lateral side of the elbow: the extensor carpi radialis longus m., the extensor carpi radialis brevis m., the extensor digiti minimi m., the extensor digitorum m., and the extensor carpi ulnaris m. • Deep to the extensor digitorum m. find the posterior interosseous a. and deep radial n. • Find the three tendons bordering the anatomical snuffbox on the lateral surface of the wrist. Follow these proximally to the muscle bellies of the abductor pollicis longus m., the extensor pollicis brevis m., and the extensor pollicis longus m. These, along with the supinator m., and the extensor indicis m. form the deep group of posterior compartment forearm muscles. • Note that the radial artery passes deep to the extensor retinaclum and deep fascia of the hand and through the anatomical snuffbox. LECTURE 10 THE HAND Muscles Thenar eminence Abductor pollicis brevis m. Opponens pollicis m. Flexor pollicis brevis m. Adductor pollicis m. Middle Compartment Lumbrical mm. Palmar interossei mm. Dorsal interossei mm. Hypothenar eminence Abductor digiti minimi m. Flexor digiti minimi m. Opponens digiti minimi m. Vessels Nerves Biomechanics Lever Systems Increasing Power LAB 10: THE HAND (Plates 62-71, 75) The structures you are responsible for identifying during this lab are: Abductor pollicis brevis m. Abductor digiti minimi m. Superficial palmar arch Flexor pollicis brevis m. Flexor digiti minimi m. Recurrent branch of the Opponens pollicis m. Opponens digiti minimi m. median n. Adductor pollicis m. Lumbrical mm. Palmar aponeurosis The Palm of the Hand • Remove the skin and superficial fascia from the palm of the hand • You should now be able to see the palmar aponeurosis. Just distal to the pisiform, cut through the palmar aponeurosis and retract it distally. Leave some of the proximal part intact, where it serves as an attachment for the palmaris longus m. • Separate the muscle bellies of the abdcutor pollicis brevis m. and flexor pollicis brevis m. and notice the opponens pollicis m. beneath them. • Note the adductor pollicis m. between the thumb and first digit. • Carefully separate the muscle bellies of the abductor digiti minimi m. and flexor digiti minimi m. far enough to see the opponens digiti minimi m. beneath them. • Gently pass a probe alongside the ulnar a., and notice it ending in the superficial palmar arch in the middle compartment of the hand. Medial to this artery you should see the ulnar n. passing deep to the hypothenar muscles. • Locate the median n. and its recurrent branch deep within the middle compartment of the palm going to the thenar muscles. Also notice the lumbrical mm. as they arise from the tendons of the flexor digitorum profundus m. The Dorsum of the Hand • On the dorsal surface of the hand note the interconnections between the tendons of the extensor digitorum muscle. • Deep to these tendons, between the metacarpals, notice the dorsal interossei mm. The First Digit • Carefully skin the index finger. • On the palmar side, follow the tendon of the flexor digitorum superficialis m. to the point where it forks, just before the proximal interphalangeal joint. Notice the tendon of the flexor digitorum profundus m. passing deep to this fork to go on to the distal phalanx. • On the dorsal surface, not the dorsal digital expansion (extensor hood) and the insertion of the lumbricals.