* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Dietary carbohydrate: relationship to cardiovascular disease and
Survey
Document related concepts
Vegetarianism wikipedia , lookup
Obesity and the environment wikipedia , lookup
Dietary fiber wikipedia , lookup
Calorie restriction wikipedia , lookup
Food choice wikipedia , lookup
Thrifty gene hypothesis wikipedia , lookup
Human nutrition wikipedia , lookup
Abdominal obesity wikipedia , lookup
Diet-induced obesity model wikipedia , lookup
Low-carbohydrate diet wikipedia , lookup
Transcript
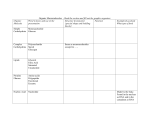
European Journal of Clinical Nutrition (2007) 61 (Suppl 1), S100–S111 & 2007 Nature Publishing Group All rights reserved 0954-3007/07 $30.00 www.nature.com/ejcn REVIEW Dietary carbohydrate: relationship to cardiovascular disease and disorders of carbohydrate metabolism J Mann Department of Human Nutrition, Edgar National Centre for Diabetes Research, University of Otago, Dunedin, New Zealand The nature of carbohydrate is of considerable importance when recommending diets intended to reduce the risk of type II diabetes and cardiovascular disease and in the treatment of patients who already have established diseases. Intact fruits, vegetables, legumes and wholegrains are the most appropriate sources of carbohydrate. Most are rich in nonstarch polysaccharides (NSPs) (dietary fibre) and other potentially cardioprotective components. Many of these foods, especially those that are high in dietary fibre, will reduce total and low-density lipoprotein cholesterol and help to improve glycaemic control in those with diabetes. There is no good long-term evidence of benefit when NSPs or other components of wholegrains, fruits, vegetables and legumes are added to functional and manufactured foods. Frequent consumption of low glycaemic index foods has been reported to confer similar benefits, but it is not clear whether such benefits are independent of the dietary fibre content of these foods or the fact that low glycaemic index foods tend to have intact plant cell walls. Furthermore, it is uncertain whether functional and manufactured foods with a low glycaemic index confer the same long-term benefits as low glycaemic index plant-based foods. A wide range of carbohydrate intake is acceptable, provided the nature of carbohydrate is appropriate. Failure to emphasize the need for carbohydrate to be derived principally from wholegrain cereals, fruits, vegetables and legumes may result in increased lipoprotein-mediated risk of cardiovascular disease, especially in overweight and obese individuals who are insulin resistant. European Journal of Clinical Nutrition (2007) 61 (Suppl 1), S100–S111; doi:10.1038/sj.ejcn.1602940 Keywords: cardiovascular disease; impaired carbohydrate metabolism Dietary carbohydrate and cardiovascular disease Traditional dietary patterns, which are high in carbohydrate, are associated with low rates of coronary heart disease (CHD). This appears to be the case regardless of the carbohydrate containing primary staple, for example rice in most Asian countries and a range of cereals, root crops and pulses in different parts of Africa. However, cross-cultural comparisons provide no indication as to whether the percentage of energy intake derived from total carbohydrate intake, total quantity of carbohydrate, particular classes of carbohydrate and other nutrients, which are found in carbohydrate-containing foods or method of food preparation, account for the cardioprotection afforded by such traditional carbohydrate-containing diets. Furthermore, it is possible that cardiovascular risk is reduced simply because Correspondence: Professor J Mann, Department of Human Nutrition, Edgar National Centre for Diabetes Research, University of Otago, Dunedin, New Zealand. E-mail: [email protected] traditional high carbohydrate diets are low in fat, especially saturated fat, or because they promote satiety and thus protect against overweight and obesity. Indeed, it is conceivable that high carbohydrate diets simply act as a marker for some other protective factor. Prospective epidemiological studies and a range of experimental approaches examining the effects of carbohydrates on cardiovascular risk factors have attempted to clarify the role of total carbohydrate and carbohydrate classes (sugars, oligosaccharides and polysaccharides) and subgroups (for example starch, nonstarch polysaccharide (NSP)) in CHD and stroke. Prospective epidemiological studies Several limitations are common to all prospective studies examining the relationship between foods and nutrients and disease risk. However, there are issues that are of particular relevance when considering the role of carbohydrates. The lack of consistency in the methods used for the measurement of different classes and subgroups of carbohydrate, Cardiovascular disease and diabetes J Mann S101 especially the NSP, complicates comparisons between the results of studies and their extrapolation into nutritional recommendations. The term ‘dietary fibre’ is often incorrectly regarded as being synonymous with NSP. However, in this paper, the terms will be used as they occur in the relevant literature, dietary fibre having been measured and reported in most of the epidemiological studies and much of the experimental research. In some countries, total carbohydrate is measured ‘by difference’, after water fat, protein and ash have all been measured. This is a less reliable measure than that derived from adding the various classes of carbohydrate measured individually (see accompanying papers on ‘definition’ and ‘measurement’). Of equal, or arguably greater, importance is the extent to which sources of dietary carbohydrate have changed over time or differ throughout the world. In some developing countries, a high proportion of total sugars may be derived from intact fruits and vegetables. The same may have been true in the past for societies that are now relatively affluent. However, nowadays, in most countries, sucrose, high fructose corn syrup and other free sugars contribute a substantial proportion of total sugars. Foods rich in free sugars are usually energy dense and are often poor sources of essential micronutrients (Baghurst et al., 1991), and are thus likely to be associated with different physiological effects and clinical consequences when compared with fruits and vegetables. Thus, knowledge of total sugar content provides little information relating to physiology. Similarly, until relatively recently, dietary fibre was likely to be derived principally from minimally processed cereals, vegetables, fruits, legumes and ‘wholegrain’ cereal foods likely to contain at least a reasonable proportion of intact or lightly processed grains. Now, dietary fibre is often an added ingredient and the definition of ‘wholegrain’ permits foods to be described as such if they contain the constituents of the grain without requiring the structure to be intact. Again, the physiological effects of dietary fibre, when derived from intact fruits, vegetables and grains, may differ from that added to manufactured products. Thus, it may not be appropriate to extrapolate the findings of epidemiological studies involving the consumption of conventional foods to carbohydrate-containing manufactured and functional foods, which provide a substantial proportion of total energy in most affluent and many developing counties. Early prospective studies reporting the cardioprotective effect of total carbohydrate intakes and intake of dietary fibre were published in the 1970s and early 1980s (Morris et al., 1977; Garcia-Palmieri et al., 1980; McGee et al., 1984). They were relatively underpowered and confounding of results by a range of factors certainly could not be excluded. During the past 20 years, results have been published from a substantial number of prospective studies involving cohorts of sufficient size to enable examination of potentially confounding factors. There has been particular emphasis on the cardioprotective role of cereal grains and dietary fibre. Most studies define wholegrain as either intact or milled grain with bran, germ and endosperm in the same proportion as the unmilled grain. Wholegrain foods have generally been arbitrarily defined as those foods with more than 25% wholegrain or bran content by weight (Flight and Clifton, 2006). The studies have been systematically reviewed (for example Liu, 2002; Truswell, 2002; Hu, 2003; Slavin, 2003; Flight and Clifton, 2006) and meta-analysed (Anderson, 2002, 2003). Despite the use of different instruments for assessing dietary intake, the results of the studies show a remarkably consistent trend. Meta-analysis, involving four of the largest published studies, suggested a 28% reduction in risk of CHD when comparing individuals in the highest and lowest quintiles of intake of wholegrains (relative risk 0.72, 95% confidence intervals: 0.48, 0.94) (Anderson 2003). The size of the most recent cohort studies has enabled analyses to examine the extent to which these findings might be confounded by other cardioprotective factors. While residual confounding cannot be excluded with absolute certainty, such analyses provide reasonable evidence that wholegrains protect against CHD regardless of the degree of adiposity and other measured variables associated with healthy lifestyles and eating habits. However, it is acknowledged that people who consistently eat wholegrain breads do indeed have different lifestyles from those who do not, and it may not be possible in epidemiological studies to measure all attributes of lifestyle. The possibility that an association is truly causal is strengthened by the existence of a dose response effect. Such an effect has been demonstrated in the Iowa Women’s Health Study. After adjustment for cardiovascular risk factors, relative risks for cardiovascular disease were 1.0, 0.96, 0.71, 0.64 and 0.70 in ascending quintiles of wholegrain intake, P for trend ¼ 0.02 (Jacobs et al., 1998). However, the epidemiological studies do not provide an indication of whether all grains are equal in this respect. There is no clear evidence as to which constituent of the grain provides cardioprotection or as to whether the structure of the grain needs to be wholly or partially intact. Relatively few groups have examined the extent to which wholegrain intakes influence the risk of stroke. Reporting on the largest of the prospective studies, the Nurses’ Health Study, Liu et al. (2000a) observed risk reductions of magnitude similar to those observed for CHD (relative risk 0.69, 95% confidence intervals: 0.50, 0.98 when comparing highest relative to lowest quintile of intake of wholegrains). Similar risk reductions have been observed in three other somewhat smaller cohorts. Wholegrains differ in a number of respects from highly refined cereals, and several of the constituents may explain their cardioprotective effects (Table 1). Dietary fibre has been studied more than the other constituents. Several groups of researchers have pooled the results from a number of studies. For example, Pereira et al. (2004) reported a relative risk of 0.90 (95% confidence intervals: 0.77, 1.07 that is not statistically significant) for total CHD events for each 10 g/day increase in cereal fibre. When considering CHD European Journal of Clinical Nutrition Cardiovascular disease and diabetes J Mann S102 Table 1 Constituents of wholegrains which may confer cardioprotection Antioxidant Dietary fibre (nonstarch polysaccharide) Unsaturated cis: n–3 and n–6 Folate Vitamin E Selenium Flavenoids Phytooestrogens O O O O O O deaths, the relative risk, 0.75 (95% confidence intervals: 0.63, 0.91) was statistically significant, the association being independent of a number of dietary factors and other cardiovascular risk factors. However, other analyses suggest that while cereal fibre is inversely associated with CHD rates, the relationship is not as strong as the inverse relationship between CHD and wholegrain bread (Anderson et al., 2000). Furthermore, the effect of dietary fibre may be largely explained by fibre derived from wholewheat, rye or pumpernickel breads (Mozaffarian et al., 2003). A single study suggested risk reduction among those with the highest intake of added bran compared with those who consumed no added bran (Jensen et al., 2004). The suggestion that reduced cardiovascular risk principally results from consumption of the wholegrain rather than dietary fibre is supported by findings from the Iowa Women’s Health Study. CHD rates were compared in women consuming similar amounts of cereal fibre from either predominantly refined grain sources or predominantly wholegrains. After adjustments, all cause mortality was significantly lower, and CHD appreciably (though not statistically significantly) reduced among the latter group (Jacobs et al., 2000). The absence of a universally adopted definition of ‘wholegrain’, and the even more inconsistent use of the terms ‘wholemeal’ and ‘wholewheat’ preclude more definitive conclusions and complicate extrapolation into guidelines. Fruits and vegetables are important sources of carbohydrate and also contain a range of potentially cardioprotective components, including dietary fibre, folate, potassium, flavonoids and antioxidant vitamins. Pooled analyses of the Nurses’ Health Study and the Health Professionals’ Follow-up Study suggested risk reductions of 20 and 30% for CHD and ischaemic stroke, respectively, when comparing extreme quintiles of fruit and vegetable intake (Joshipura et al., 2001). Similar findings were reported in a recent meta-analysis (He et al., 2006). A dose–response effect was reported with lowest risk for CHD being associated with eight servings or more per day and for stroke, four or more servings daily. It is noteworthy that in this, the largest study reported to date, individual items relatively low in total carbohydrate appear to have the most striking protective effect—green leafy vegetables in the case of CHD and cruciferous vegetables, citrus fruits and juices and vitamin C-rich European Journal of Clinical Nutrition Lipid-lowering Enzyme modulator O fruits and vegetables in the case of stroke. In the Physicians’ Health Study, Liu et al. (2001) reported an inverse association between carotenoid rich vegetables and CHD risk, and Finnish data suggested that flavonoid-rich foods (for example berries, onions, apples) were especially beneficial in this regard (Knekt et al., 1994). Legume consumption four or more times per week compared with less than once per week has also been associated with cardiovascular risk reduction (Bazzano et al., 2001). During the 1960s, Yudkin (1964) and co-workers reported strong associations between high sugar intakes and CHD. The data were cross-sectional and flawed (Keys, 1971; Truswell, 1987). The Iowa Women’s Health Study found no relationship between intake of sweets and desserts and CHD in over 30 000 women followed for 9 years (Jacobs et al., 1998). The glycaemic index (GI; and more recently the glycaemic load, GL) has provided a means of determining the extent to which carbohydrate-containing foods may determine cardiovascular risk through their potential to raise blood glucose. Liu et al. (2000b) reported from the Nurses’ Health Study that women who consumed diets with a highglycaemic load (that is high in rapidly digested starches) were at increased risk of CHD compared with those with a lower consumption; a twofold increase in risk over a 10-year follow-up was observed when comparing those in the highest and lowest quintiles of intake. The effect appeared to be independent of total energy intake and other cardiovascular risk factors. The potential of dietary patterns, rather than the effect of individual foods and nutrients on human health, have been examined in two of the largest cohort studies—the Nurses’ Health Study and the Health Professionals’ Study (Hu et al., 2000; Fung et al., 2001b). Factor analysis was used to examine the association between CHD and two major dietary patterns identified: ‘western’ and ‘prudent’. The prudent pattern was characterized by higher intakes of fruits, vegetables, legumes, fish, poultry and wholegrains and the western pattern, by higher intakes of red and processed meats, sweets and desserts, French fries and refined grains. After adjustment for cardiovascular risk factors, the prudent diet score was associated with relative risks of 1.0, 0.87, 0.79, 0.75 and 0.70 from the lowest to the highest quintiles. Conversely, the relative risks across increasing quintiles of the western pattern score were 1.0, Cardiovascular disease and diabetes J Mann S103 1.21, 1.35, 1.40 and 1.64. The patterns were also related to biochemical markers of CHD. Positive correlations were noted between the western pattern score and plasminogen activator antigen, fasting insulin, C-peptide, leptin, C-reactive protein and homocysteine after adjustment for confounders. A significant inverse correlation was observed between plasma folate and the western dietary pattern score. Inverse correlations were observed between the prudent pattern score and fasting insulin and homocysteine, and a positive correlation was observed with folate (Fung et al., 2001a). In summary, prospective epidemiological studies provide strong evidence for a protective role of wholegrain cereals, fruits and vegetables and dietary patterns characterized by relatively high intakes of such foods. While a high consumption of dietary fibre derived from cereals is also associated with a reduced risk of cardiovascular disease, it is not clear whether the cardioprotection can entirely be attributed to the polysaccharides per se. The effect seems to stem largely from dietary fibre in dark breads and may therefore be at least partially attributable to other constituents of wholegrains. It is not possible to determine the extent to which other potentially protective constituents of wholegrains are relevant. Epidemiological studies do not permit separating the effects of different wholegrains. Even the best prospective studies cannot conclusively eliminate the possibility of residual confounding, so recommendations regarding the intake of carbohydrates in relation to cardiovascular disease also depend on the intervention studies described below. Carbohydrates and cardiovascular risk factors Lipids and lipoproteins The effect of carbohydrates on lipids and lipoproteins has dominated discussions regarding the amounts and classes of carbohydrate likely to reduce cardiovascular risk. While there is no doubt that increasing total carbohydrate at the expense of fat, especially saturated and trans fatty acids in the Western diet, will result in reduction of total and lowdensity lipoprotein (LDL) cholesterol, concern has been expressed that other predictors of lipoprotein-mediated cardiovascular risk may be adversely affected by substantial increases in total carbohydrate. The potential of high carbohydrates to increase fasting triglycerides was first demonstrated in the 1960s (Ahrens et al., 1961) but later considered to be a transient phenomenon, the hypertriglyceridaemia diminishing with prolonged exposure to a high carbohydrate intake (Antonis and Bersohn, 1961; Stone and Connor, 1963). However, more recent and more sophisticated studies suggest that, at least in certain circumstances, a low-fat, high carbohydrate diet may be associated with slightly elevated triglyceride levels for as long as 2 years (Retzlaff et al., 1995). Furthermore, such a diet may result in the appearance of small dense LDL particles that are particularly atherogenic and in an adverse ratio of total to high-density lipoprotein (HDL) cholesterol considered to be a more specific marker of CHD than total LDL cholesterol (Kinosian et al., 1995). The effect of carbohydrate as replacement energy for fatty acids has been examined in a fairly recent meta-analysis involving 60 mostly short-term controlled trials (Mensink et al., 2003). The results appeared to offer a strong message: regardless of the source of the fat displaced, an increase in total carbohydrate was associated with an increased ratio of total to HDL cholesterol. However, although these studies paid careful attention to ensure that the comparisons were carried out under isoenergetic conditions and food intake was thoroughly controlled, there was less consistency with regard to the source and class of carbohydrate that was used as fat replacement. A fairly substantial body of evidence suggests that the type of carbohydrate influences lipid and lipoprotein levels. The effect of sugars on triglyceride levels differs from that of polysaccharides. Compared with starches and NSPs, sugars, especially sucrose and fructose, may be associated with appreciable increases in triglyceride levels, especially when the sugars are consumed in the context of a diet high in total carbohydrate or when dietary fat comprises principally of saturated fatty acids (Truswell, 1994). The effect appears to be more marked in insulin resistant individuals with abdominal obesity (Fried and Rao, 2003). Unfortunately, few long-term data are available. However, the CARMEN study suggested that after 6 months, a very modest weight loss could mitigate the hypertriglyceridaemic effect of a moderate increase in sucrose (Saris et al., 2000). This has also been observed for diets high in total carbohydrate and starches, which might otherwise have been associated with hypertriglyceridaemia when compared with diets lower in total carbohydrates (Kasim-Karakas et al., 2000). Dietary fibre has a potentially important effect on lipids and lipoproteins when consumed in plant foods or as supplements Viscous subgroups, including pectins, b-glucans, glucomannans, guar and psyllium, which are generally water soluble, all lower total and LDL cholesterol between 5 and 10 g/day, lowering LDL by about 5% (Truswell, 2002). The mechanism appears to be by reducing ileal bile acid absorption (Morgan et al., 1993). These soluble forms of dietary fibre appear to have a negligible effect on triglyceride or HDL levels. Insoluble dietary fibre subgroups are derived largely from cereal sources and have little or no effect on lipids and lipoproteins (Jenkins et al., 2000). A Cochrane Review has been undertaken of randomized controlled trials (RCTs) investigating the effects of wholegrain cereals on CHD and cardiovascular risk factors. Only 10 studies were identified that met the strict criteria required for such a review. None had clinical end points. They compared wholegrain foods or diets high in wholegrain foods with other foods or diets with lower levels or no wholegrains. Eight of the ten studies evaluated wholegrain oats and clearly demonstrated the potential of such foods to reduce total LDL cholesterol. Levels were about 0.2 mmol/l lower European Journal of Clinical Nutrition Cardiovascular disease and diabetes J Mann S104 on the diet rich in oats compared with the control diet. No changes were observed in triglyceride or HDL cholesterol levels. Lack of appropriate studies precluded conclusions on wholegrains other than oats (Brunner et al., 2005). A Cochrane Review has also been undertaken to explore the extent to which low glycaemic index diets might influence CHD and risk factors. The average reduction in total cholesterol when comparing low and high GI diets was 0.17 mmol/l, P ¼ 0.03 (95% CI 0.32 to 0.02). No convincing differences were apparent in LDL cholesterol, HDL cholesterol or triglyceride levels (Kelly et al., 2004). In studies of free living individuals in whom fruits, vegetables and legumes rich in the viscous forms of NSPs replaced some of the relatively high fat foods typically consumed in a western diet, total and LDL cholesterol fell as expected, and the ratio of total (or LDL) cholesterol to HDL cholesterol improved with no change reported in triglyceride despite an appreciable increase in total carbohydrate (Turley et al., 1998). Total carbohydrate provided 59 and 43% total energy on the high and low carbohydrate diets. While the aim of these studies was not to achieve weight loss, small reductions in body weight did occur on the high carbohydrate diets, perhaps as a result of the enhanced satiety associated with the more bulky, less energy dense foods. This, together with the effects of dietary fibre, are likely to have contributed to the less atherogenic lipid profile observed on the high carbohydrate diet. Such findings provide a clear indication of the need to consider the nature of dietary carbohydrate when carbohydrate rich foods are recommended as replacement for dietary saturated fatty acids. Type II diabetes, impaired carbohydrate metabolism and insulin resistance See later section, which deals more fully with this topic. Inflammatory markers There has been considerable recent interest in the role of inflammation as a determinant of cardiovascular risk. Much of the research relating to the role of nutritional determinants has centred around different dietary fats (Basu et al., 2006). Jenkins et al. (2003) reported reduced C-reactive protein levels in hyperlipidaemic patients consuming a high carbohydrate diet rich in viscous fibre-containing foods. However, the diets were also high in nuts (almonds), plant sterols and soy proteins, and it is therefore impossible to disentangle separate effects. A very recent study (KasimKarakas et al., 2006) found that when carbohydrate replaced a substantial proportion of dietary fat under eucaloric conditions, the levels of several inflammatory markers increased along with an increase in triglyceride. However, when the participants (post-menopausal women) consumed the 15% fat diet ad libitum under free living conditions, they European Journal of Clinical Nutrition lost weight and triglyceride and the levels of inflammatory markers decreased. Hypertension Several ‘high carbohydrate’ dietary approaches have been shown to be associated with reduced levels of blood pressure. However, these have invariably involved many dietary changes. For example, the Dietary Approaches to Stop Hypertension approaches have involved an increase in intakes of fruits and vegetables, low fat dairy products and a reduction in sodium. Thus, it has been impossible to disentangle individual effects (Appel et al., 1997). RCT involving clinical end points A single RCT has examined the effect of altering dietary carbohydrate intakes on clinical end points. Burr et al. (1989) randomized 2033 men who had survived a myocardial infarction to receive one of eight possible combinations of dietary advice. Those who were advised to increase cereal fibre had a similar rate of CHD recurrences and deaths as those who did not receive this advice when considering a 10-year follow-up period. However, the study was underpowered and the degree of compliance is uncertain (Ness et al., 2002). Other RCTs, which involved an increase in dietary carbohydrate, from fruits, vegetables, legumes and wholegrain, as part of a multifactorial dietary approach to primary and secondary prevention of CHD, demonstrated reduction in clinical events among those receiving intensive dietary advice compared with control groups (Hjermann et al., 1981; de Lorgeril et al., 1994). The Women’s Health Initiative Randomised Control for Dietary Modification Trial involved the intervention group being recommended a high carbohydrate low fat diet. Failure to demonstrate significant differences in CHD rates in control and intervention groups contributed little to the understanding of the role of carbohydrates since long-term compliance with the intervention diet was poor (Howard et al., 2006). Dietary carbohydrate and cardiovascular disease: recommendations The joint WHO/FAO Expert Consultation on Diet, Nutrition and the Prevention of Chronic Disease (WHO Technical Report Series 916, 2003) considered that the evidence suggesting a cardio-protective effect of fruits and vegetables was ‘convincing’ and that relating to wholegrain cereals and NSP was ‘probable’. The evidence that high intakes of total carbohydrate might increase the risk of cardiovascular diseases was considered to be ‘insufficient’ (Table 10, p88 TRS 916). Difficulties with regard to the definition of wholegrains and inability to exclude the possibility of Cardiovascular disease and diabetes J Mann S105 residual confounding provide the justification for regarding the protective effect being graded as ‘probable’ rather than ‘convincing’. The Expert Consultation recommended that total carbohydrate should provide 55–75% total energy and that free sugars should provide less than 10%. Recommended intake of fruits and vegetables was 400 or more g per day, excluding tubers (that is potatoes, cassava). Precise amounts of NSPs or dietary fibre were not recommended. However, it was considered that appropriate intakes of fruits, vegetables, legumes and regular consumption of wholegrain cereals would provide in excess of 20 g/day of NSP and over 25 g of total dietary fibre. There was also no recommendation regarding glycaemic index. These recommendations would appear to be generally compatible with this update of the relevant literature with the following caveats: Many western countries have average intakes of carbohydrate, which are below 55% total energy. There is no good evidence that total carbohydrate intake for populations or individuals must reach the lower recommended intake in order to achieve a cardioprotective dietary pattern provided guidelines relating to dietary fat and other nutrients are met. Several national guidelines suggest a lower limit of 50% total energy. A wide range of carbohydrate intakes is compatible with cardioprotection. However, it is important to be prescriptive with regard to the nature of carbohydrate, especially when total carbohydrate intakes are at the upper end of the recommended range. Failure to emphasize the need for carbohydrate to be derived principally from wholegrain cereals, fruits, vegetables and legumes may result in increased lipoprotein-mediated risk of CHD associated with an increase in the ratio of total (or LDL) cholesterol to HDL cholesterol and an increase in triglyceride. This may apply particularly to overweight and obese individuals who are insulin resistant (see separate section on diabetes and insulin resistance). While fruits and legumes rich in viscous (soluble) forms of NSP and dietary fibre are associated with reduced LDL cholesterol, insoluble forms derived from wholegrain cereals also appear to confer cardioprotection possibly in association with other constituents of wholegrains. There is no convincing evidence that fibre supplements and manufactured and functional foods containing them reduce cardiovascular risk. Dietary carbohydrate and diabetes, impaired carbohydrate metabolism and the metabolic syndrome The escalating rates of type II diabetes worldwide and the realization that insulin resistance and its associated metabolic abnormalities contribute increasingly to the global epidemic of cardiovascular disease (Mann, 2000) have resulted in renewed interest in the nutritional determinants of these metabolic derangements. In the 1960s, Yudkin suggested that sugar (sucrose) was a major determinant of type II diabetes (then known as ‘maturity onset’ and later as ‘non-insulin dependent’ diabetes). The conclusions were based largely on highly selected, within country and cross country, comparisons (Yudkin, 1964; Nuttall and Gannon, 1981) later acknowledged to be totally inappropriate analyses (Nuttall et al., 1985). At about the same time, Trowell, then working in Uganda, suggested that the low rates of diabetes in rural Africa were likely to result from a protective effect of large intakes of dietary fibre found in the minimally processed or unprocessed carbohydrate, which provided a high proportion of total dietary energy in such societies (Trowell, 1975). Although it was not possible to know the extent to which these observations implied true causation or protection or simply represented confounding, they stimulated much subsequent epidemiological and experimental research. Prospective epidemiological studies A number of limitations apply to all prospective studies that have examined the association between foods and nutrients and the risk of various diseases. The issues that are potentially relevant to dietary carbohydrate have been considered in the previous section on cardiovascular disease, and they apply equally when relating various carbohydrates to risk of developing diabetes. Recent prospective studies provide some insight. In the Nurses’ Health Study, there was no association between total intake of grains and type II diabetes. However, wholegrain consumption appeared to be protective. When comparing the highest and lowest quintiles of intake, age and energy adjusted relative risk was 0.62 (95% CI: 0.53, 0.71). Further adjustment for other risk factors did not appreciably alter this risk estimate (Liu et al., 2000). A virtually identical risk reduction was observed among men participating in the Health Professionals Study (Fung et al., 2002). A relative risk of 0.63 was reported in association with three or more servings per day of wholegrains. In the Iowa Women’s Health Study, postmenopausal women in the upper quintile of wholegrain consumption (more than 33 servings per week) were 20% less likely to develop type II diabetes than those in the lowest quintile (fewer than 13 servings per week) (Meyer et al., 2000). Wholegrains have also been shown to be protective against type II diabetes in African-Americans (van Dam et al., 2006), Finns (Montonen et al., 2003) and Iranians (Esmaillzadeh et al., 2005). Cereal fibre, as distinct from fibre derived from other sources, appears to be associated with a protective dose–response effect that is present after controlling for a range of potentially confounding factors. In the Nurses’ Health Study, multivariate relative risks for quintiles 1–5 were 1.0, 0.85, 0.87, 0.82 and 0.64, respectively (Salmeron et al., 1997a). The role of wholegrains and dietary fibre in diabetes has been reviewed in detail in Venn and Mann (2004). European Journal of Clinical Nutrition Cardiovascular disease and diabetes J Mann S106 In the Nurses’ Health Study and the Health Professionals Follow-up Study, a statistically significant relative risk of about 1.4 was observed when comparing diabetes rates in the highest and lowest quintiles of dietary glycaemic load, after adjusting for potentially confounding factors (Salmeron et al., 1997a, b). A high dietary glycaemic index was also found to be associated with an increased risk of type II diabetes in the Melbourne Collaboration Cohort Study (Hodge et al., 2004). Rapidly digested starches and sugars, especially glucose, contribute to the glycaemic load of the diet, and thus such observations provide some evidence for a promotive role of these carbohydrates in type II diabetes. However, no association was found between sucrose intake and risk of diabetes during a 6-year follow-up of the Nurses’ Health Study (Colditz et al., 1992). Meyer et al. (2000), reporting the findings from the Iowa Women’s Health Study, found no relationship between type II diabetes and either glycaemic index or glycaemic load. However, dietary glucose and fructose (but not sucrose) were associated with increased risk. Women who developed gestational diabetes in the Nurses’ Health Study had lower intakes of dietary fibre and higher dietary glycaemic load than those who did not (Zhang et al., 2006). No prospective studies have examined the relationship between dietary carbohydrate and insulin resistance, considered to be the underlying abnormality in most cases of type II diabetes. However, two large cross-sectional studies, using validated food frequency questionnaires to assess nutrient intake and either the frequently sampled intravenous glucose tolerance test or homoeostasis model assessment for insulin resistance, found that intake of dietary fibre was inversely associated with the probability of having insulin resistance (Lau et al., 2005; Liese et al., 2005). In the Insulin Resistance Atheroscelerosis Study (Liese et al., 2005), it was possible to demonstrate that fibre was associated with increased insulin sensitivity even after adjustment for body mass index. Interestingly, neither study found any relationship between insulin sensitivity and glycaemic index or glycaemic load. While diets rich in wholegrains and dietary fibre may protect against diabetes and pre-diabetic states by virtue of their potential to promote satiety and weight loss in those who are overweight or obese (excess adiposity being the major determinant of these metabolic abnormalities), the epidemiological data do provide evidence for a protective effect independent of that on fat mass. The data do not permit distinction among different grains nor the extent to which structure of the grain or its constituents explain the protective effect. Several studies suggest that diets with a relatively low glycaemic index or glycaemic load are protective against disorders of carbohydrate metabolism, but the data are insufficient to establish with certainty the extent to which this is independent of other attributes of carbohydrates. European Journal of Clinical Nutrition Experimental studies Most studies that have compared the effects of carbohydrates and fats and the effects of different carbohydrates have been undertaken in people with established diabetes; however, some information is available concerning people with insulin resistance and the metabolic syndrome. Insulin resistance and its associated dyslipidaemia (high triglyceride, low HDL) have been shown to be more marked on a high carbohydrate diet when compared with a diet rich in monounsaturated fatty acids. However, while such studies may distinguish between sugars and polysaccharides, they often do not distinguish between starches, many of which are rapidly digested and absorbed, and NSPs (Mann, 2001). A study by Pereira et al. (2002) clearly demonstrates the importance of doing so. In a controlled 6-week study, overweight hyperinsulinaemic adults consumed diets providing 55% energy from carbohydrate and 30% from fat. Carbohydrates were derived from predominantly wholegrain or refined grain cereals, with dietary fibre content of the wholegrain diet 28 g compared with 17 g on the refined grain diet. Dietary fibre was predominantly from cereal sources. Total carbohydrate and fat and fat sources were virtually identical on the two diets. Insulin sensitivity measured by a euglycaemic hyperinsulinaemic clamp was appreciably improved on the wholegrain compared with the refined grain diet. Fasting insulins and area under the 2-h insulin curve were lower, despite body weight not being significantly different on the two diets. Rye bread (Juntunen et al., 2003) and purified cereal fibre (Weickert et al., 2006) have been shown to improve insulin sensitivity in overweight and obese women. Analysis of a subgroup of individuals within the CARMEN Study, who were diagnosed with the metabolic syndrome, showed that the reduction in body weight and improvement in metabolic indices seen when simple carbohydrate (sugars) were replaced with complex ones were more striking in people with this disorder than in the general population (Poppitt et al., 2002). Studies by McAuley et al. (2005; 2006) have compared different nutritional approaches in overweight insulin-resistant women. Although a low carbohydrate high fat diet resulted in initial weight loss and improvement in the metabolic derangements associated with insulin resistance, the improvement was not sustained. A diet relatively high in protein and unsaturated fat sources and with moderate amounts of fibre-rich carbohydrate, and one low in total fat and relatively high in fibre-rich carbohydrate produced sustained weight loss and improvement in a range of metabolic measurements over a period of a year. Thus, while weight loss in those who are overweight or obese is the cornerstone of management aimed at improving insulin sensitivity, it appears that this can be achieved by diets relatively high or relatively low in carbohydrates, provided the carbohydrate sources are wholegrain and rich in dietary fibre. Other studies that have compared the effects of diets of varying amounts of Cardiovascular disease and diabetes J Mann S107 carbohydrate have generated broadly similar results (Nordmann et al., 2006). The fact that fructose, compared with glucose, is preferentially metabolized to lipid in the liver and that fructose consumption induces insulin resistance, impaired glucose tolerance, hyperinsulinaemia, hypertriglyceridaemia and hypertension in animal models has led to the suggestion that fructose, sucrose or high fructose corn syrup may have uniquely untoward effects compared with other carbohydrates in humans when fed in the context of energy balance. However, while these sugars may contribute to increasing the risk of overweight and obesity and thus to the clinical and metabolic disorders (Mann, 2004), the evidence regarding fructose remains limited and conflicting, and no conclusions can be drawn (Elliott et al., 2002; Daly, 2003). A large number of studies have been undertaken to determine the extent to which total quantity and nature of dietary carbohydrate influence glycaemic control, insulin resistance and cardiovascular risk factors in people with type II diabetes. While such studies apply principally to diabetes management, it seems reasonable to assume that the data also have some relevance to disease prevention. A meta-analysis of nine studies has been undertaken to compare the effects of high carbohydrate and high monounsaturated fatty acid diets. The overall results provide evidence of higher fasting triglycerides and VLDL cholesterol, slightly lower HDL cholesterol, slightly higher glucose, but not glycated haemoglobin on the high carbohydrate diets, typically providing 55–60% total energy from carbohydrate (Garg, 1998). There was considerable variation in the results of the individual studies, partly due to the fact that they were all relatively underpowered and also because the severity of diabetes may influence response to dietary carbohydrate. However, equally important is the fact that the nature of dietary carbohydrate was not clearly specified. It appears that a range of ‘complex carbohydrates’ provided a substantial proportion of total carbohydrate on the high carbohydrate diets. It seems that there may have been a lack of appreciation regarding the different effects of starches and NSPs and indeed the different effects of NSPs from different sources. This is surprising, given that in the late 1980s, it had been clearly shown that high carbohydrate diets were only associated with beneficial effects in terms of glycaemic control and blood lipids when carbohydrate was derived principally from foods rich in soluble forms of dietary fibre, notably pulses, legumes and intact fruits and vegetables (Rivellese et al., 1980; Simpson et al., 1981; Riccardi et al., 1984; Mann, 2001). Higher intakes of cereal (insoluble) fibre were associated with less marked or no benefit in glucose or lipid levels (Simpson et al., 1979; 1982; Riccardi et al., 1984). The beneficial effects of soluble forms of dietary fibre derived from fruits and vegetables appear to have been rediscovered more recently in randomized crossover studies in type II diabetes (Chandalia et al., 2000). Dietary fibre has also been shown to be of benefit in type I diabetes (Giacco et al., 2000). Cross-sectional epidemiological data, based on the EURODIAB Complications Study, which included over 2000 patients in 31 European centres, showed an inverse association between dietary fibre intake of HbA1c and LDL cholesterol (in men only) and a positive association with HDL cholesterol in men and women (Toeller et al., 1999). An RCT (parallel design) in type I patients continued for 6 months, confirmed the potential for around 40 g/day dietary fibre (half of the soluble type from legumes, fruits and vegetables) to improve glycaemic control (Giacco et al., 2000). Some studies have shown improved glycaemic control when soluble fibres have been fed as supplements to patients with diabetes. However, evidence-based nutritional guidelines of the Nutrition Study Group of the European Association for the Study of Diabetes offer no recommendations regarding supplements of functional foods providing increased dietary fibre. Long-term clinical trials are deemed necessary before recommendations can be considered (Mann et al., 2004). In the 1980s, several RCT with crossover designs demonstrated no adverse effects on glycaemic control, lipids and lipoproteins when diets containing small amounts of sucrose (usually around 50 g) were compared under eucaloric conditions with virtually sucrose-free diets in type I and type II diabetes (Slama et al., 1984; Peterson et al., 1986; Mann, 1987). While there is thus clear evidence for the acceptability of moderate intakes of sucrose for most people with diabetes, there are few data from which to derive acceptable upper limits. For those who are overweight or obese or are markedly insulin resistant, fairly severe restriction may be appropriate. For all others, moderate intakes of free sugars (up to 50 g/day) are acceptable, provided that free sugars do not exceed 10% total energy. There are suggestions that sugar in beverages increases body weight to a greater extent than the same amount of sugar in the solid form (diMeglio and Mattes, 2000). A number of randomized trials have examined the extent to which diets with a low glycaemic index can improve glycaemic control and cardiovascular risk factors. Several meta-analyses have been published (Brand-Miller et al., 2003; Opperman et al., 2004) and the results are broadly comparable. For example, Opperman et al. reported a reduction in HbA1c of 0.27 (95% confidence intervals: 0.5 to 0.03) when comparing high and low glycaemic index diets. This issue was examined in a Cochrane Systematic Review, which suggested some evidence of an effect of low GI diets compared with high GI diets after 12 weeks. Pooled analysis of studies with a parallel design demonstrated mean HbA1c levels 0.45% less than the high GI diets (95% confidence intervals: 0.82 to 0.09, P ¼ 0.02). It is of importance to note that the low GI foods utilized in most of the studies were plant based (for example peas, lentils, beans, pasta, barley, parboiled rice, oats and cereals) as were the high GI foods (potatoes, wheatmeal and white bread and high GI breakfast cereals). The studies did not generally include many of the now widely available manufactured and functional foods, which are not necessarily predominantly plant based. European Journal of Clinical Nutrition Cardiovascular disease and diabetes J Mann S108 RCT with clinical end points Two RCTs involving people with impaired glucose tolerance consuming ‘western’ diets have examined the extent to which progression of impaired glucose tolerance to type II diabetes can be reduced by intensive lifestyle modification (Tuomilehto et al., 2001; Knowler et al., 2002). In both the Finnish and US intervention studies, advice regarding frequent consumption of wholegrain products, vegetables and fruits has been a pivotal component of the advice to achieve weight loss. Other components included recommendations to use monounsaturated oils, soft margarines and low fat meat and milk products, as well as to increase physical activity of moderate intensity. These interventions achieved a nearly 60% reduction of progression from impaired glucose tolerance to type II diabetes. While it is impossible to accurately disentangle the separate contributions of the different components of the intervention package, and weight loss was clearly the major determinant of risk reduction, increased intake of dietary fibre appeared to be independently associated with reduced risk of progression (Lindstrom et al., 2003). A similar study has been conducted in India (Ramachandran et al., 2006). Dietary carbohydrate and diabetes: recommendations The Joint WHO/FAO Expert Consultation on Diet, Nutrition and the Prevention of Chronic Disease (WHO Technical Report Series 916, 2003) describes the protective effect of NSP as ‘probable’. However, an explanatory note indicates that the level of evidence is graded as ‘probable’ rather than ‘convincing’ because of the apparent discrepancy between the experimental studies, in which it appears that soluble forms of NSP exert benefit in terms of glycaemic control, lipids and lipoproteins, and the prospective cohort studies, which suggest that cereal-derived insoluble forms are protective. The evidence regarding low glycaemic index foods as protective is graded as ‘possible’. The evidence table (Table 9, p 77 TRS 916) leads to the disease-specific recommendation regarding intakes of NSP, which quite appropriately disregards a clear distinction between soluble and insoluble forms and suggests that adequate intakes of NSP or dietary fibre can be achieved through regular consumption of wholegrain cereals, legumes, fruits and vegetables. There is no clear evidence on which to base precise quantities although a minimum intake of 20 g of NSP is recommended. These recommendations appear to be compatible with this update of the relevant literature with two caveats: There appears to be a reasonable body of evidence to suggest a protective effect of wholegrains. The apparently different effects of soluble and insoluble forms of NSP or dietary fibre may result from difficulty in accurately distinguishing between the two forms. European Journal of Clinical Nutrition Similar approaches to those suggested for reducing disease risk have been recommended for the management of diabetes. The European evidence-based nutritional approaches (Mann et al., 2004) to the treatment of diabetes indicate that a wide range of intakes of total carbohydrate (45–60% total energy) is acceptable, provided a high proportion of carbohydrate energy is derived from vegetables, legumes, fruits and wholegrain cereals. This should provide the recommended intake of total dietary fibre (more than 40 g/day or 20 g/1000 kcal/day), about half of which should be soluble. Cereal-based foods should whenever possible be wholegrain and high in fibre. Daily consumption of at least five servings of fibre-rich vegetables or fruits and at least four servings of legumes per week help to provide the minimum requirements for fibre. While a choice anywhere within this range is acceptable for most people, it is acknowledged that some, especially those with marked hypertriglyceridaemia and/or severe insulin resistance, may respond more appropriately to an intake at the lower end of the recommended range. Use of carbohydrate-containing foods with a low glycaemic index is encouraged. While a moderate amount of sugar is acceptable in the context of energy balance, those who are overweight should substantially restrict sugar-containing energy-dense foods. Sugar-containing beverages, while not energy dense, promote overweight and obesity and are best avoided. Finally, it is important to emphasize that the beneficial effects of certain carbohydrate-containing foods have been based principally on the consumption of conventional foods. Evidence for the benefit of manufactured and functional foods containing added dietary fibre or other components of wholegrains, fruits, vegetables and legumes is limited. This applies also to foods with a low glycaemic index. Some foods now marketed as having a low glycaemic index are high in fat and sugar and therefore may not be suitable for people with diabetes, especially those who are overweight. The paper describing the European recommendations (Mann et al., 2004) provides a detailed list of references justifying the conclusions summarized here. Conclusions Nutritional attributes that are likely to protect against diabetes and cardiovascular diseases are remarkably similar as are the principles of nutritional management for those who already have established disease. In summary, they are as follows: A wide range of intakes of carbohydrate containing foods is acceptable. Nature of carbohydrate rather than quantity is principally what matters. Intact fruits, vegetables, legumes and wholegrains are excellent sources of carbohydrate likely to be rich in NSP or dietary fibre and other potentially cardioprotective components. Cardiovascular disease and diabetes J Mann S109 There is no good evidence of benefit when NSP or other components of wholegrains, fruits, vegetables and legumes are added to functional and manufactured foods. Low glycaemic index foods may confer benefits in terms of lowering total cholesterol and improving glycaemic control in people with diabetes. However, it is not clear whether these benefits are independent of the effects of dietary fibre or the fact that low glycaemic index foods tend to have intact plant cell walls. Furthermore, it is uncertain whether functional and manufactured foods with a low glycaemic index confer the same long-term benefits as low glycaemic index predominantly plantbased foods. A low dietary glycaemic load may reduce the risk of type II diabetes and cardiovascular disease. The same caveats as those described above for the therapeutic role of low GI foods apply. Limitations to the use of the glycaemic index and glycaemic load concepts in the clinical setting are further described in the accompanying paper in this series. Acknowledgements I thank Professor Kjeld Hermansen, Dr Andrew Neil, Dr Gabriele Riccardi, Dr Angela Rivellese, Dr Monika Toeller, Professor A Stewart Truswell, Dr Rob M van Dam and Dr HH Vorster for the valuable comments they provided on the earlier paper. Conflict of interest During the preparation and peer-review of this paper in 2006, the author and peer-reviewers declared the following interests. Author Professor Jim Mann: none declared. Peer-reviewers Professor Kjeld Hermansen: none declared. Dr Andrew Neil: none declared. Dr Gabriele Riccardi: none declared. Dr Angela Rivellese: none declared. Dr Monika Toeller: none declared. Professor A Stewart Truswell: none declared. Dr Rob M van Dam: none declared. Dr HH Vorster: member and director of the Africa Unit for Transdisciplinary health Research (AUTHeR), Research grant from the South African Sugar association. References Ahrens E, Hirsch J, Oette K, Farquhar J, Stein Y (1961). Carbohydrateinduced and fat-induced lipemia. Trans Assoc Am Physicians 74, 134–146. Anderson JW (2002). Whole-grains intake and risk for coronary heart disease. In: Marquart L, Slavin JL, Fulcher RD (eds). Whole-grain Foods in Health and Disease. American Association of Cereal Chemists. St Paul: Minnesota, USA. pp 187–200. Anderson JW (2003). Whole grains protect against atherosclerotic cardiovascular disease. Proc Nutr Soc 62, 135–142. Anderson JW, Hanna TJ, Peng X et al. (2000). Whole grain foods and heart disease risk. J Am Coll Nutr 19, 291S–299S. Antonis A, Bersohn I (1961). The influence of diet on serum-triglycerides in South African White and Bantu prisoners. Lancet 7, 39. Appel LJ, Moore TJ, Obarzanek E et al. (1997). For the DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 336, 1117–1124. Baghurst KI, Record SJ, Baghurst PA (1991). The relationship between refined sugar and micronutrient intakes. Proc Nutr Soc Australia 16, 33. Basu A, Devaraj S, Jialal I (2006). Dietary factors that promote or retard inflammation. Arterioscler Thromb Vasc Biol 26, 995–1001. Bazzano LA, He J, Ogden LG, Loria C, Vupputuri S, Myers L et al. (2001). Legume consumption and risk of coronary heart disease in US men and women: NHANES 1 Epidemiologic Follow-up Study. Arch Intern Med 161, 2573–2578. Brand-Miller J, Hayne S, Petocz P et al. (2003). Low-glycemic index diets in the management of diabetes: a meta-analysis of randomized controlled trials. Diabetes Care 26, 2261–2267. Brunner EJ, Thorogood M, Rees K, Hewitt G (2005). Dietary advice for reducing cardiovascular risk. Cochrane Database of Systematic Reviews 4, Art. No: CD002128.DOl: 10.1002/. Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM et al. (1989). Effects of changes in fat, fish and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet ii, 757–761. Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ (2000). Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med 342, 1392–1398. Colditz GA, Manson JF, Stampfer MJ, Rosner B, Willett WC, Speizer FF (1992). Diet and risk of clinical diabetes in women. Am J Clin Nutr 55, 1018–1023. Daly M (2003). Sugars, insulin sensitivity, and the postprandial state. Am J Clin Nutr 78, 865S–872S. de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin J, Monjaud I et al. (1994). Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 343, 1454–1459. DiMeglio DP, Mattes RD (2000). Liquid versus solid carbohydrate: effects on food intake and body weight. Int J Obes Relat Metab Disord 24, 794–800. Elliott SS, Keim NS, Stern JS, Teff K, Havel PJ (2002). Fructose, weight gain, and the insulin resistance syndrome. Am J Clin Nutr 76, 911–922. Esmaillzadeh A, Mirmiran P, Azizi F (2005). Whole-grain consumption and the metabolic syndrome: a favorable association in Tehranian adults. Eur J Clin Nutr 59, 353–362. Flight I, Clifton P (2006). Cereal grains and legumes in the prevention of coronary heart disease and stroke: a review of the literature. Eur J Clin Nutr 60, 1145–1159. Fried SK, Rao SP (2003). Sugars, hypertriglyceridemia, and cardiovascular disease. Am J Clin Nutr 78 (Suppl 8), 73S–80S. Fung TT, Hu FB, Pereira MA et al. (2002). Whole-grain intake and the risk of type 2 diabetes: a prospective study in men. Am J Clin Nutr 76, 535–540. Fung TT, Rimm EB, Spiegelman D, Rifai N, Tofler GH, Willett WC et al. (2001a). Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr 73, 61–67. Fung TT, Willett WC, Stampfer MJ, Manon JE, Fu FB (2001b). Dietary patterns and risk of coronary heart disease in women. Arch Intern Med 161, 1857–1862. European Journal of Clinical Nutrition Cardiovascular disease and diabetes J Mann S110 Garcia-Palmieri MR, Sorlie P, Tillotson J, Costas Jr R, Cordero E, Rodriguez M (1980). Relationship of dietary intake to subsequent coronary heart disease incidence: The Puerto Rico Heart Health Program. Am J Clin Nutr 33, 1818–1827. Garg A (1998). High-monounsaturated-fat diets for patients with diabetes mellitus: a meta-analysis. Am J Clin Nutr 67, 577S–582S. Giacco R, Parillo M, Rivellese AA et al. (2000). Long-term dietary treatment with increased amounts of fiber-rich low-glycemic index natural foods improves blood glucose control and reduces the number of hypoglycemic events in type 1 diabetic patients. Diabetes Care 23, 1461–1466. He FJ, Nawson CA, Macgregor GA (2006). Fruit and vegetable consumption and stroke: metaanalysis of cohort studies. Lancet 367, 320–326. Hjermann I, Byer K, Holme I et al. (1981). Effect of diet and smoking intervention on the incidence of coronary heart disease. Lancet ii, 1303–1310. Hodge AM, English DR, O’Dea K et al. (2004). Glycaemic Index and dietary fiber and the Risk of type 2 diabetes. Diabetes Care 27, 2701–2706. Howard BV, van Horn JH, Manson JE et al. (2006) (reprinted) Low-fat dietary pattern and risk of cardiovascular disease: the women’s health initiative randomized controlled dietary modification trial. JAMA 295, 655–666. Hu FB (2003). Plant-based foods and prevention of cardiovascular disease: an overview. Am J Clin Nutr 78 (Suppl 3), 544S–551S. (review). Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC (2000). Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr 72, 912–921. Jacobs Jr DR, Meyer KA, Kushi LH, Folsom AR (1998). Whole-grain intake may reduce the risk of ischemic heart disease death in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr 68, 248–257. Jacobs Jr DR, Pereira MA, Meyer KA, Kushi LH (2000). Fiber from whole grains, but not refined grains, is inversely associated with all-cause mortality in older women: the Iowa women’s health study. J Am Coll Nutr 19, 326S–330S. Jenkins DJ, Kendall CW, Marchie A, Faulkner DA, Wong JM, de Souza R et al. (2003). Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA 290, 502–510. Jenkins DJA, Kendall CWC, Axelsen M, Augustin LSA, Vuksan V (2000). Viscous and nonviscous fibres, nonabsorbable and low glycaemic indeed carbohydrates, blood lipids and coronary heart disease. Curr Opin Lipidol 11, 49–56. Jensen MK, Koh-Banerjee P, Hu FB, Franz M, Sampson L, Gronbaek M et al. (2004). Intakes of whole grains, bran, and germ and the risk of coronary heart disease in men. Am J Clin Nutr 80, 1492–1499. Joshipura KJ, Hu FB, Manson JE et al. (2001). The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med 134, 1106–1114. Juntunen KS, Laaksonen DE, Poutanen KS, Niskanen LK, Mykkanen HM (2003). High-fiber rye bread and insulin secretion and sensitivity in healthy postmenopausal women. Am J Clin Nutr 77, 385–391. Kasim-Karakas SE, Almario RU, Mueller WM, Peerson J (2000). Changes in plasma lipoproteins during low-fat, high-carbohydrate diets: effects of energy intake. Am J Clin Nutr 71, 1439–1447. Kasim-Karakas SE, Tsodikov A, Singh U, Jialal I (2006). Responses of inflammatory markers to a low-fat, high carbohydrate diet: effects of energy intake. Am J Clin Nutr 83, 774–779. Kelly S, Frost G, Whittaker V et al. (2004). Low glycaemic index diets for coronary heart disease. Cochrane Database Syst Rev 18, CD004467. European Journal of Clinical Nutrition Keys A (1971). Sucrose in the diet and coronary heart disease. Atherosclerosis 14, 193–202. Kinosian B, Glick H, Preiss L, Puder KL (1995). Cholesterol and coronary heart disease: predicting risks in men by changes in levels and ratios. J Invest Med 43, 443–450. Knekt P, Reunanen A, Jarvinen R, Seppanen R, Heliovaara M, Aromaa A (1994). Antioxidant vitamin intake and coronary mortality in a longitudinal population study. Am J Epidemiol 139, 1180–1189. Knowler WC, Barrett-Connor E, Fowler SE, et al. , For the Diabetes Prevention Program Research Group (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346, 393–403. Lau C, Faerch K, Glumer C, Tetens I, Pedersen O, Carstensen B et al. (2005). Dietary glycemic index, glycemic load, fiber, simple sugars, and insulin resistance: the Inter 99 study. Diabetes Care 28, 1397–1403. Liese AD, Schulz M, Fang F, Wolever TM, D’Agostino RB, Sparks KC et al. (2005). Dietary glycemic index and glycemic load, carbohydrate and fiber intake, and measures of insulin sensitivity, secretion, and adiposity in the Insulin Resistance Atherosclerosis Study. Diabetes Care 28, 2832–2838. Lindstrom J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J et al. (2003). The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26, 3230–3236. Liu S (2002). Intake of refined carbohydrates and whole grain foods in relation to risk of type 2 diabetes mellitus and coronary heart disease. J Am Coll Nutr 21, 298–306. Liu S, Lee IM, Ajani U, Cole SR, Buring JE, Manson JE (2001). Intake of vegetables rich in carotenoids and risk of coronary heart disease in men: the Physicians’ Health Study. Int J Epidemiol 30, 130–135. Liu S, Manson JE, Stampfer MJ et al. (2000). A prospective study of whole-grain intake and risk of type 2 diabetes mellitus in US women. Am J Public Health 90, 1409–1415. Liu S, Manson JE, Stampfer MJ, Rexrode KM, Hu FB, Rimm EG et al. (2000a). Whole grain consumption and risk of ischemic stroke in women: a prospective study. JAMA 284, 1534–1540. Liu S, Willett WC, Stampfer MJ, Hu FB, Franz M, Sampson L et al. (2000b). A prospective study of dietary glycaemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr 71, 1455–1461. Mann J (2001). Dietary fibre and diabetes revised. Eur J Clin Nutr 55, 919–921. Mann J (2004). Free sugars and human health: sufficient evidence for action? Lancet 363, 1068–1070. Mann JI (1987). Simple sugars and diabetes. Diabet Med 4, 135–139. Mann JI (2000). Stemming the tide of the diabetes epidemic. Lancet 356, 1454–1455 (editorial). Mann JI, De Leeuw I, Hermansen K, Karamanos B, Karlström B, Katsilambros N et al. (2004). Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Nutr Metab Cardiovasc Dis 14, 373–394. McAuley KA, Hopkins CM, Smith KJ, McLay RT, Williams SM, Taylor RW et al. (2005). Comparisons of high-fat and high-protein diets with a high-carbohydrate diet in insulin-resistant obese women. Diabetologia 48, 8–16. McAuley KA, Smith KJ, Taylor RW, McLay RT, Williams SM, Mann JI (2006). Long-term effects of popular dietary approaches on weight loss and features of insulin resistance. Int J Obes 30, 342–349. McGee DL, Reed DM, Yano K, Kagan A, Tillotson J (1984). Ten-year incidence of coronary heart disease in the Honolulu Heart Program: relationship to nutrient intake. Am J Epidemiol 119, 667–676. Mensink RP, Zock PL, Kester ADM, Katan MB (2003). Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a metaanalysis of 60 controlled trials. Am J Clin Nutr 77, 1146–1155. Cardiovascular disease and diabetes J Mann S111 Meyer KA, Kushi LH, Jacobs Jr DR, Slavin J, Sellers TA, Folsom AR (2000). Carbohydrates, dietary fiber, and incident type 2 diabetes in older women. Am J Clin Nutr 71, 921–930. Montonen J, Knekt P, Jarvinen R, Aromaa A, Reunanen A (2003). Whole-grain and fiber intake and the incidence of type 2 diabetes. Am J Clin Nutr 77, 622–629. Morgan LM, Tredger JA, Shavila Y, Travis JS, Wright J (1993). The effect of non-starch polysaccharide supplementation on circulating bile acids, hormone and metabolite levels following a fat meal in human subjects. Br J Nutr 70, 491–501. Morris JN, Marr JW, Clayton DG (1977). Diet and heart: a postscript. BMJ 2, 1307–1314. Mozaffarian D, Kumanyika SK, Lemaitre RN, Olson JL, Burke GL, Siscovick DS (2003). Cereal, fruit and vegetable fiber intake and the risk of cardiovascular disease in elderly individuals. JAMA 289, 1659–1666. Ness AR, Hughes J, Elwood PC, Whiteley E, Smith GD, Burr ML (2002). The long-term effect of dietary advice in men with coronary disease: follow-up of the Diet and Reinfarction trial (DART). Eur J Clin Nutr 56, 512–518. Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy Jr WS, Brehm BJ et al. (2006). Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 166, 285–293. Nuttall FO, Gannon MC, Wald JL, Ahmed M (1985). Plasma glucose and insulin profiles in normal subjects ingesting diets of varying carbohydrate, fat, and protein content. J Am Coll Nutr 4, 437–450. Nuttall FO, Gannon MC (1981). Sucrose and disease. Diabetes Care 4L, 305–310. Opperman AM, Venter CS, Oosthuizen W et al. (2004). Meta-analysis of the health effects of using the glycaemic index in mealplanning. Br J Nutr 92, 367–381. Pereira MA, Jacobs Jr DR, Pins JJ, Raatz SK, Gross MD, Slavin JL et al. (2002). Effect of whole grains on insulin sensitivity in overweight hyperinsulinaemic adults. Am J Clin Nutr 75, 848–855. Pereira MA, O’Reilly E, Augustsson K, Fraser GE, Goldbourt U, Heitmann BL et al. (2004). Dietary fiber and risk of coronary heart disease: a pooled analysis of cohort studies. Arch Intern Med 164, 370–376. Peterson DB, Lambert J, Gerring S et al. (1986). Sucrose in the diet of diabetic patients-just another carbohydrate? Diabetologia 29, 216–220. Poppitt SD, Keogh GS, Prentice AM, Williams DE, Sonnemans HM, Valk EE et al. (2002). Long-term effects of ad libitum low-fat, high-carbohydrate diets on body weight and serum lipids in overweight subjects with metabolic syndrome. Am J Clin Nutr 75, 11–20. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V (2006). The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP—1). Diabetologia 49, 289–297. Retzlaff BM, Walden CE, Dowdy AA, McCann BS, Anderson KV, Knopp RH (1995). Changes in plasma triacylglycerol concentrations among free-living hyperlipidemic men adopting different carbohydrate intakes over two years: The Dietary Alternatives Study. Am J Clin Nutr 62, 988–995. Riccardi G, Rivellese A, Pacioni D, Genovese S, Mastranzo P, Mancini M (1984). Separate influence of dietary carbohydrate and fibre on the metabolic control in diabetes. Diabetologia 26, 116–121. Rivellese A, Riccardi G, Giacco A et al. (1980). Effect of dietary fibre on glucose control and serum lipoproteins in diabetic patients. Lancet 2, 447–450. Salmeron J, Ascherio A, Rimm EB et al. (1997b). Dietary fiber, glycemic load, and risk of NIDDM in men. Diabetes Care 20, 545–550. Salmeron J, Manson JE, Stampfer MJ et al. (1997a). Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA 277, 472–477. Saris WH, Astrup A, Prentice AM et al. (2000). Randomized controlled trial of changes in dietary carbohydrate/fat ratio and simple vs complex carbohydrates on body weight and blood lipids: the CARMEN study. The Carbohydrate Ratio Management in European National diets. Int J Obes Relat Metab Disord 24, 1310–1318. Simpson HCR, Carter RD, Lousley S, Mann JL (1982). Digestible carbohydrate—an independent effect on diabetic control in type 11 (non-insulin dependent) diabetic patients? Diabetologia 23, 235–239. Simpson HCR, Simpson RW, Lousley S et al. (1981). A high cabohydrate leguminous fibre diet improves all aspect of diabetic control. Lancet 1, 1–5. Slama G, Haardt MJ, Jean-Joseph P et al. (1984). Sucrose taken during mixed meal has no additional hyperglycaemic action over isocaloric amounts of starch in well-controlled diabetes. Lancet 2, 122–125. Slavin J (2003). Why whole grains are protective: biological mechanisms. Proc Nutr Soc 62, 129–134. Stone D, Connor W (1963). The prolonged effects of a lowcholesterol, high-carbohydrate diet upon serum lipids in diabetic patients. Diabetes 12, 127–132. Toeller M, Buyken AE, Heitkamp G, de Pergola G, Giorgino F, Fuller JH (1999). Fiber intake, serum cholesterol levels, and cardiovascular disease in European individuals with type 1 diabetes. EURODIAB IDDM Complications Study Group. Diabetes Care 22 (Suppl 2), B21–B28. Trowell H (1975). Dietary-fiber hypothesis of the etiology of diabetes mellitus. Diabetes 24, 762–765. Truswell AS (1987). Sugar and health: a review. Food Technology in Australia 39, 134–140. Truswell AS (1994). Food carbohydrates and plasma lipids—an update. Am J Clin Nutr 59, 710S–718S. Truswell AS (2002). Cereal grains and coronary heart disease. Eur J Clin Nutr 56, 1–14. Tuomilehto J, Lindström J, Eriksson JG et al. (2001). For the Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 334, 1343–1350. Turley ML, Skeaff CM, Mann JI, Cox B (1998). The effect of a low-fat, high-carbohydrate diet on serum high density lipoprotein cholesterol and triglyceride. Eur J Clin Nutr 52, 728–732. Van Dam RM, Hu FB, Rosenberg L, Krishnan S, Palmer JR (2006). Dietary calcium and magnesium, major food sources, and risk of type 2 diabetes in US black women. Diabetes Care 29, 2238–2243. Venn BJ, Mann JI (2004). Cereal grains, legumes and diabetes. Eur J Clin Nutr 58, 1443–1461. Weickert MO, Mohlig M, Schofl C et al. (2006). Cereal fiber improves whole-body insulin sensitivity in overweight and obese women. Diabetes Care 29, 775–780. WHO Technical Report Series 916 (2003). Diet, nutrition and the prevention of chronic diseases. Report of a Joint WHO/FAO Expert Consultation (Geneva). Yudkin J (1964). Dietary fat and dietary sugar in relation to ischaemic heart disease and diabetes. Lancet 4, 4–5. Zhang C, Liu S, Solomon CG et al. (2006). Dietary fiber intake, dietary glycemic load and the risk for gestational diabetes mellitus. Diabetes Care 29, 2223–2230. European Journal of Clinical Nutrition