* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Bone Mineral Density and Fat-Soluble Vitamin Status in Adults with
Survey
Document related concepts
Transcript
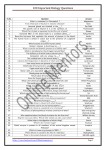
Pagination not final (cite DOl) / Pagination provisoire (citer Ie DOl). REPORT / RApPORT Bone Mineral Density and Fat-Soluble Vitamin Status in Adults with Cystic Fibrosis Undergoing Lung Transplantation: A Pilot Study GRACE HUBERT, RD BSca; THERESA TAM CHUNG, RD BSca; CONNIE PROSSER, PhD FCACBb; DALE LIEN, MDc; JUSTIN WEINKAUF, MDc; NEIL BROWN, MDc; MARIANNE GOODVIN, RN BNScd; KATHY JACKSON, RN BNScd; JOAN TABAK, RNe; JOSETTE SALGADO, RN BNSce; ABEER SALMAN ALZABEN, MScf; DIANA R. MAGER, PhD MSc RDfg "Nutrition Services, Alberta Health Services, Edmonton, AB; bDepartment of Laboratory Medicine, University of Alberta, Edmonton, AB; 'Division of Pulmonary Medicine, Department of Medicine, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB; dLung Transplant Program, Alberta Health Services, Edmonton, AB; "Adult Cystic Fibrosis Clinic, Alberta Health Services, Edmonton, AB; fDepartment of Agricultural, Food and Nutritional Science, University of Alberta, Edmonton, AB; gDepartment of Pediatrics, University of Alberta, Edmonton, AB ABSTRACT RESUME Purpose: Patients with cystic fibrosis (CF) often experience low bone Objectif. Les patients atteints de fibrose kystique (FK) ont souvent une mineral density (BMD) pre- and post-lung transplantation (LTX). The study purpose was to describe BMD and micronutrient status in adults with CF pre- and post-LTX. Methods: Twelve patients with CF (29 ± 8 years) were recruited from the CF clinic at the University of Alberta Lung Transplant Program. BMD and vitamins A, D, E, K status, and parathyroid hormone were measured pre- and post-LTX. Results: No significant differences pre- and post-LTX were observed at the different bone sites measured (lumber-spine, femoral-neck (FN), hip, and femoral-trochlea) (p) 0.05). BMD T-scores «-2) was present in lumbar-spine, FN, hip, and femoral-trochlea in 33%, 17%, 17%, and 25% of individuals pre-LTX and 58%, 33%, 58%, and 33% of individuals post-LTX, respectively. More than 50% of patients had suboptimal vitamin K levels (PIVKA-li values) 3 ng/mL) pre- and post-LTX. Conclusion: Adults with CF pre- and post-LTX had reduced BMD and suboptimal vitamin K status. (Can I Diet Pract Res. 2016;77:1-4) (DOl: 10.3148/cjdpr-2016-014) Published at dcjournal.ca on 19 July 2016. densite minerale osseuse (DMO) faible avant et apres la transplantation pulmonaire (TP). L'objectif de l'etude etait de decrire la DMO et l'etat nutritionnel en micronutriments des adultes atteints de FK avant et apres la TP. Methodes. Douze patients atteints de FK (29 ± 8 ans) ont ete recrutes Ii la clinique de FK du programme de transplantation pulmonaire de l'Universite de l'Alberta. La DMO et l'etat nutritionnel en vitamines A, D, E et K, et I'hormone parathyro'lde ont ete rnesures avant et apres la TP. Resultats. Aucune difference significative n'a ete observee avant et apres la TP aux differents sites osseux mesures (rachis lombaire, col femoral, hanche et trochlea femorale) (p ) 0,05). Des scores T de la DMO « - 2) etaicnt presents dans Ie rachis lombaire, Ie col femoral, la hanche et la trochlea femorale chez 33 %, 17 %, 17 % et 25 % des personnes avant la TP et chez 58 %, 33 %, 58 % et 33 % des personnes apres la TP, respectivement. Plus de 50% des patients avaient des taux de vitamine K sous-optimaux (concentrations de PIVKA-II ) 3 ng/rnl) avant et apres la TP. Conclusion. Les adultes atteints de FKavaient une DMO reduite et un taux de vitamine K sous-optimal avant et apres la TP. (Rev can prat rech dletet. 2016;77: 1-4) (DOl: 10.3148/cjdpr-2016-014) Publie au dcjournal.ca Ie 19 juillet 2016. INTRODUCTION Maintenance of bone health in patients with cystic fibrosis (CF) is an ongoing challenge, especially as the disease becomes more severe and the need for lung transplantation (LTX) becomes more eminent [1]. Pre-LTX and post-LTX, individuals with CF are at high risk for low bone mineral density (BMD) related to chronic use of corticosteroid and other immunosuppressive therapy (such as tacrolimus), antibiotic use and chronic undernutrition secondary to poor intake, increased energy expenditure, and pancreatic insufficiency [2-4). Suboptimal fat-soluble vitamin intake due to inadequate or poor diet quality and/or noncompliance to prescribed vitamin supplementation can also contribute to low BMD. Several studies have shown that fat-soluble vitamins can be low preLTX [5-7), whereas post-LTX, hypervitaminnosis A can contribute to low BMD [8). The University of Alberta Lung Transplant Program provides LTX for patients with end-stage lung disease from Alberta, including individuals with CF who have a reported 60%-75% 5-year survival rate [9). With increased survival, Canadian Journal of Dietetic Practice and Research - Vol 77, 2016 Pagination not final (cite 001) / Pagination provisoire (citer Ie 001). REPORT / RApPORT poor bone health is a significant concern, especially as it relates to increased morbidity and mortality and overall quality of life [4, 10]. Limited exposure to sunlight in northern climates also increases the risk for vitamin D (vitD) deficiency and subsequent poor bone health. For these reasons, patients are routinely supplemented with commercially available fatsoluble vitamins (A, D, E, and K) pre- and post-LTX. Although suboptimal vitamin K (vitK) status has been shown to be a contributor to low bone health in many clinical populations [11], it is currently unknown what the current prevalence of suboptimal vitK status is in adult patients post-LTX. This is particularly relevant in the CF population, as on-going fat malabsorption due to pancreatic insufficiency is not corrected or improved by lung transplantation. This pilot study describes BMD and fat-soluble vitamin status in adult CF subjects, pre- and post -LTX. METHODS Ethics approval (Pro 00001737) was obtained from the Human Research Ethics Board at the University of Alberta prior to study initiation. Adult CF patients (age> 18 years) who were referred to the University of Alberta Lung Transplant program between 2005 and 2012 were recruited and enrolled over a 12-month period. Study inclusion criteria included those on anti-resorptive therapy, as this is part of routine clinical care. Exclusion criteria included terminal illness, intensive care unit stay >72 hours, and subjects who were unable to provide informed consent. A total of 25 patients with CF undergoing lung transplant assessment were screened for eligibility; 13 were excluded due to coinciding illness requiring hospitalization, early lung TX, and/or refusal to participate. No Significant differences in demographic or anthropometric variables were noted between those who agreed to participate in the study and those who did not. Informed consent was obtained from all participants. Height and weight were measured using validated techniques. Blood was collected for measurement of vitamins A, D, E, and K (protein indicated in vitamin K absence (PIVKA-II)) and parathyroid hormone (PTH) at LTX assessment and at 3, 6, and 12 months post-LTX. The samples were analyzed according to standardized methodologies in the Core Laboratory at Alberta Health Services [12]. Serum 25-hydroxy vitamin D (25(OH)D) concentrations were assessed according to the Canadian Endocrine Practice Guidelines «75 nmol/L, insufficient/suboptimal; >75 nrnol/L, optimal) [13]. BMD was measured using hologic dual-energy X-ray absorptiometry 450 at LTX assessment and at 9 and 18 months postLTX (whole body, hip, femoral-neck (FN), femoral-trochlea, lumbar-spine). Analyses were performed using Statistical Analysis Software (SAS; version 9.4 SAS Institute, Cary, NC, USA). Data were analyzed by treating individual patient data as single measures, rather than repeated measures due to the small sample size at each individual time point. Continuous variables were expressed as mean ± SD. Normality was assessed using 21 Revuecanadiennede la pratiqueet de la rechercheen dietetique - Vol 77, 2016 the Shapiro-Wilk test. Non-parametric variables were log transformed. Continuous variables were analyzed using dependent t test to assess differences pre- and post-LTX with adjustments for potential confounding variables (season, age, sex). Statistical Significance was determined at P < 0.05. RESULTS Demographic, anthropometric, and laboratory data Anthropometric and demographic data for the 12 patients pre- and post-LTX are shown in Table 1. No significant age difference at time of LTX assessment was observed between sexes (males, 29 ± 10 years vs. females, 31 ± 6 years; P = 0.70). A total of 42% (n = 5) and 17% (n = 2) of participants had a mean BMI reflective of suboptimal nutritional status (BMI < 18.5) pre- and post-LTX, respectively. Laboratory data are shown in Table 2. Although there was no Significant difference in estimated glomerular filtration rate (GFR), values in 58% of patients were indicative of renal insufficiency (GFR <60; stage 3 chronic kidney disease) post-LTX. In addition, significant differences in urea, creatinine, and PTH pre- and post-LTX were noted, indicating worsening renal function and secondary hyperparathyroidism in 83% of patients postLTX. The majority of patients (67% pre-LTX and 58% postLTX) had optimal 25(OH) vitD levels (>75 nrnol/L), likely secondary to vitD supplementation (400-8700 IV/d) [13]. A total of 58% and 55% of patients had suboptimal vitK status (PIVKA-II values >3 ng/mL) pre- and post-LTX, respectively, despite routine recommendation for vitK supplementation Table 1. Anthropometric and bone health variables pre- and post-LTX in adult patients with cystic fibrosis. Anthropometrics Age (y) Weight (kg)b Height (m) BMI (kg/m2)b Spine BMD (gm/c2)C Hip BMD (gm/cm2)C Femoral-neck BMD (grn/crrr')" Femoraltrochlea BMD Pre-LTX (n=12; 7M, 5W Post-LTX (n=12; 7M, 5F)a 29 ± 8 (19-49) 54.8 ± 9.0 (39.1-71.0) 1.68 ± 0.08 (1.55-1.81) 19.3 ± 3.2 (15.1- 25.7) 0.86 ± 0.11 (0.69-1.03) 0.82 ± 0.14 (0.57-1.08) 0.71 ± 0.10 (0.56-0.90) 0.60 ± 0.11 (0.43-0.82) 30 ± 8 (19-52) 60.3 ± 5.6 (51.4-67.8) 1.68 ± 0.08 (1.55-1.81) 21.4 ± 2.4 (17.5-25.0) 0.86 ± 0.10 (0.69-1.07) 0.77 ± 0.12 (0.54-1.04) 0.67 ± 0.11 (0.54-0.91) 0.55 ± 0.10 (0.40-0.77) p 0.371 0.098 >0.05 0.103 0.992 0.262 0.324 0.166 (grn/cm)" 'Dataarepresentedasmean± standarddivision(range). bThenumberof measurements post-LTX was 11. 'Thenumberof repeatedmeasurements post-LTX was22. Note:LTX,lungtransplantation; M, male;F. female;BMI,bodymassindex;BMD.bone mineraldensity. Pagination not final (cite 001) / Pagination provisoire (citer Ie 001). REPORT / RApPORT Table 2. Laboratory variables pre- and post-LTXin adult patients with cystic fibrosis Biochemical '<, o Pre-LTX(n=12)a Vitamin A (IJmoI/L)b PIVKAII (ng/rnl)" Vitamin E (IJmoI/L)b Calcium (mrnol/l)'' PTH(prnol/l)" 25(OH)D (nrnol/L)" Urea (mrnol/L)" Creatinine (IJmoI/L)f GFR(ml/min/1.73 m2)g Hemoglobin A1C (%)h Post-LTX(n=12)a 1.4 ± 0.3 (0.8-2.0) 80.0 ± 171.9 (0.1-427.8) 26 ± 9 (10-43) 2.25 ± 0.10 (2.08-2.38) 4.4 ± 3.9 (1.4-160) 83 ± 40 (10-154) 4.3 ± 1.5 (1.2-6.8) 64 ± 18 (35-99) 60 ± 0 (60-60) 6.34 ± 0.57 (5.5-7.4) 2.7 ± 0.8 (1.3-4.0) 6.4 ± 14.2 (0.1-64.2) 40 ± 18 (13-86) 2.26 ± 0.13 (2.10-2.80) 9.8 ± 11.9 (2.1-61.0) 85 ± 23 (43-141) 7.1 ± 2.8 (19-10.7) 108 ± 35 (48-166) 53 ± 9 (30-60) 6.11 ± 0.47 (5.4-7.1) p Normal reference ranges 1.5-3.5 ,,3 12-45 2.10-2.60 1.2-6.8 <75 2.5-8.0 M: 50-115 F: 50-105 >60 <6.1 <0.001 0.206 0.010 0.773 0.025 0.798 0.006 <0.001 0.090 >0.05 'Data are presentedas mean ± standard division (range). bThenumber of measurementspre-L1Xwas 12; the number of repeated measurementspost-L1Xwas 33 'The number of measurementspre-Llx was 11; the number of repeated measurementspost-Llx was 20. dThenumber of measurementspre-L1Xwas 12; the number of repeated measurementspost-L1Xwas 34. 'The number of measurementspre-Ux was 12; the number of repeated measurementspost-L1Xwas 13. rThenumber of measurementspre-Ux was 12; the number of repeated measurementsposH1X was 24. gThenumber of measurementspre-Llx was 6; the number of repeated measurementsposHTX was 17. "None of the participants pre-L1Xwere on exogenous insulin vs 83% post-L1Xwho were on exogenousinsulin. Note: L1X,lung transplantation; PIVKAII, proteins Induced by vitamin K absenceII; PTH,parathyroid hormone; 25(OH)D,25-hydroxy vitamin D; GFR, glomerular filtration rate. (> 1 mg/d). Significant differences in serum retinol levels and vitamin E levels were also observed pre- and post- LTX (P < 0.05) with daily vitamin A (26 501 ± 14040 IU/d) and vitamin E (260 ± 179 IU/d) supplementation. Routine vitamin supplementation was typically in the form of single vitD (>1000 IU) and/or multivitamin preparations. Bone mineral density BMD data are shown in Table 1 and Figure 1. No significant differences pre- and post-LTX were observed at the different site measures (lumbar-spine, FN, hip and femoral-trochlea) (P > 0.05). With the exception of spinal-BMD (absolute; Figure 1. The average T-score of spine, hip, femoral-neck and femoral-trochlea pre- (n=12) and post-lung transplant (LTX)in adult patients with cystic fibrosis (n=12). The number of measurements post-LTXwas n=22 for hip, femoral-neck, and femoral-trochlea and n=23 for spine. 0.0 -0.5 -1.0 8 -1.5 Q) .: -2.0 II -+---1--1----1--1----1--1-- -2.5 +--I--I-----=.----I----~-3.0+-+-1:-----------3.5L.---------·Spine Hip Femoral Neck _ _ Femoral Trochlea Pre-LTX ..Post-LTX females, 0.91 ± 0.08 vs males, 0.82 ± 0.09 gm/cm/, P = 0.002) and T scores (females, -1.27 ± 0.79 vs males, -2.25 ± 1.26; P == 0.015), no Significant differences in absolute or T scores were observed between sexes at the different sites measured (P> 0.05). BMD T scores «-2) indicative of osteoporosis were present in lumbar-spine, hip, FN, and femoral-trochlea in 33%, 17%, 17%, and 25% individuals pre-LTX, respectively. In contrast, BMD T scores «-2) were present in lumbarspine, hip, FN and femoral-trochlea in 58%, 33%, 58%, and 33% individuals post-LTX, respectively. DISCUSSION This is a descriptive, pilot study that describes fat-soluble vitamin status and BMD in adults with CF pre- and post-LTX in a northern Canadian LTX program. A Significant finding is that the majority of patients had reduced BMD and suboptimal vitK status, despite healthcare practitioner recommendation for fat-soluble vitamin supplementation. Several factors may have influenced these findings such as low patient adherence to prescriber recommendation, ongoing pancreatic insufficiency and malabsorption refractive to pancreatic enzyme replacement therapy, poor diet quality, reduced weightbearing activities, and use of immunosuppressive medications such as corticosteroids, tacrolimus, and antibiotics (e.g., tobramycin) [14, 15]. Many patients in this cohort were underweight at the time of LTX and hence had suboptimal nutritional status. Although, weight status improved postLTX, deficits in nutritional intake and weight-bearing activity, ongoing pancreatic insufficiency and the use of corticosteroid therapy (typically 10-15 mg/d, but tapered down to alternative day therapy and/or discontinuation by 6-12 months), and/or Canadian Journal of Dietetic Practice and Research - Vol 77, 2016 3 Pagination not final (cite 001) / Pagination provisoire (citer Ie 001). REPORT / RApPORT other medications such as tacrolimus may have contributed to reduced BMD [9, 15-17]. Suboptimal vitD status is highly prevalent in northern climates like Alberta [18, 19]. Although patients in general had serum 25(OH)D levels above 75 nmol/L and normal PTH levels, higher vitD levels in conjunction with weight-bearing activities may be needed to optimize bone health pre- and post-LTX. Findings regarding poor bone health are similar to other LTX centres where ongoing nutritional challenges in adult LTX recipients place them at high risk for poor bone health [20]. A major limitation in this study includes the small sample size, which limits the overall generalizability of the findings. However, a post-hoc power test indicated sufficient power (~ > 0.8) to discriminate reduced BMD at the different sites pre- and post-LTX. Unique findings include the high prevalence of suboptimal vitK status post-LTX. These findings underscore the importance of routine follow-up by healthcare practitioners in patients with CF undergoing LTX. Future studies should focus on assessing adherence to vitamin therapy, and the impact of vitK supplementation on bone health parameters. '<, o RELEVANCE TO PRACTICE Patients with CF are at high risk for poor bone health and micronutrient insufficiency, This underscores the need for highly specialized medical teams to address ongoing micronutrient deficiencies in this population. Registered Dietitians are uniquely positioned to help optimize bone health and micronutrient status by developing effective nutrition care plans and exploring the barriers and facilitators to achieving nutritional goals in complex care populations. Acknowledgements The authors gratefully acknowledge the participants in this study. Funding: Canadian Lung Transplantation Study Group. Personal funding for ASA by the King Abdullah Program for Scholarship- Saudi Cultural Bureau is also gratefully acknowledged. Conflicts of interest: None to report. References 1. Elkin SL, Fairney A, Burnett S, Kemp M, Kyd P, Burgess J, et at. Vertebral deformities and low bone mineral density in adults with cystic fibrosis: a cross-sectional study. Osteoporos Int. 2001;12(5):366-72. doi: 10.10071 s001980170104. 2. Bianchi ML, Romano G, Saraifoger S, Costantini D, Limonta C, Colombo C. BMD and body composition in children and young patients affected by cystic fibrosis. J Bone Miner Res. 2006;21(3):388-96. doi: 10.13591 JBMR.051106. 4 Revue canadienne de la pratique et de la recherche en dietetique - Vol 77, 2016 3. Aris RM, Merkel PA, Bachrach LK, Borowitz DS, Boyle MP, Elkin SL, et at. Guide to bone health and disease in cystic fibrosis. J Clin Endocrinol Metab. 2005;90(3):1888-96. doi: 10.1210/jc.2004-1629. 4. Fok J, Brown NE, Zuberbuhler P, Tabak J, Tom M. Low bone mineral density in cystic fibrosis patients. Can J Diet Pract Res. 2002;63(4): 192-7. doi: 10.3148/63.4.2002.192. 5. Culhane S, George C, Pearo B, Spoede E. Malnutrition in cystic fibrosis: a review. Nutr Clin Pract. 2013;28(6):676-83. doi: 10.1177/0884533613507086. 6. Maqbool A, Stallings VA. Update on fat-soluble vitamins in cystic fibrosis. Curr Opin Pulm Med. 2008;14(6):574-81. doi: 10.1097/MCP. oto 13e3283136787. 7. Lowery EM, Bemiss B, Cascino T, Durazo-Arvizu RA, Forsythe SM, Alex C, et at. Low vitamin D levels are associated with increased rejection and infections after lung transplantation. J Heart Lung Transplant. 2012;31 (7):700-7. doi: 10.1016/j.healun.2012.02.012. 8. Ho T, Gupta S, Brotherwood M, Robert R, Cortes D, Verjee Z, et at. Increased serum vitamin A and E levels after lung transplantation. Transplantation. 2011;92(5):601-6. doi: 10.1097ITP.Ob013e31822790e3. 9. Fidalgo P, Ahmed M, Meyer SR, Lien D, Weinkauf J, Kapasi A, et al. Association between transient acute kidney injury and morbidity and mortality after lung transplantation: a retrospective cohort study. J Crit Care. 2014;29(6):1028-34. doi: 10.1016/j.jcrc.2014.07.024. 10. Santana MJ, Feeny D, Jackson K, Weinkauf J, Lien D. Improvement in health-related quality of life after lung transplantation. Can Respir J. 2009;16(5):153-8. doi: 10.1155/2009/843215. 11. Bertolaso C, Groleau V, Schall II, Maqbool A, Mascarenhas M, Latham NE, et at. Fat-soluble vitamins in cystic fibrosis and pancreatic insufficiency: efficacy of a nutrition intervention. I Pediatr Gastroenterol Nutr. 2014;58 (4):443-8. doi: 1O.1097/MPG.0000000000000272. 12. Hoffmann MR, [ackson ST, Iindal K, Senior PA, Mager DR. Vitamin D status, body composition and glycemic control in adults with diabetes and chronic kidney disease. Eur I Clin Nutr. 2015;70(6):743-749. doi: 1O.1038/ejcn.2015.185. 13. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et at. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. IClin Endocrinol Metab. 2011;96(7):1911-30. doi: 10.1210/jc.2011-0385. 14. Aringer M, Kiener HP, Koeller MD, Artemiou 0, Zuckermann A, Wieselthaler G, et al. High turnover bone disease following lung transplantation. Bone. 1998;23(5):485-8. doi: 10.1016/S8756-3282(98)00130-6. 15. Mazziotti G, Canalis E, Giustina A. Drug-induced osteoporosis: mechanisms and clinical implications. Am I Med. 2010;123(10):877-84. doi: 10. 1016/j.amjmed.20 10.02.028. 16. Mager DR, Alzaben AS, Roberts C, Gilmour SM, Yap). Bone mineral density and growth in children having undergone liver transplantation with a corticosteroid-free immunosuppressive protocol. JPEN J Parenteral Enteral Nutr. 2015;1-9. doi: 10.1177/0148607115609524. 17. Paccou I. Fardellone P, Cortet B. Cystic fibrosis-related bone disease. Curr Opin Pulm Med. 2013;19(6):681-6. doi: 10.1097/MCP.Ob013e328365ge35. 18. Langlois K, Greene-Finestone L, Little J, Hidiroglou N, Whiting S. Vitamin D status of Canadians as measured in the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2010;21(1):47-55. 19. Whiting SJ, Langlois KA, Vatanparast H, Greene-Finestone LS. The vitamin D status of Canadians relative to the 20 II Dietary Reference Intakes: an examination in children and adults with and without supplement use. Am J Clin Nutr. 2011;94(1):128-35. doi: 1O.3945/ajcn.llI.013268. 20. Wang TK, O'Sullivan 5, Gamble GD, Ruygrok PN. Bone density in heart or lung transplant recipients - a longitudinal study. Transplant Proe. 2013;45(6):2357-65. doi: 10.1016/j.transproceed.2012.09.117.